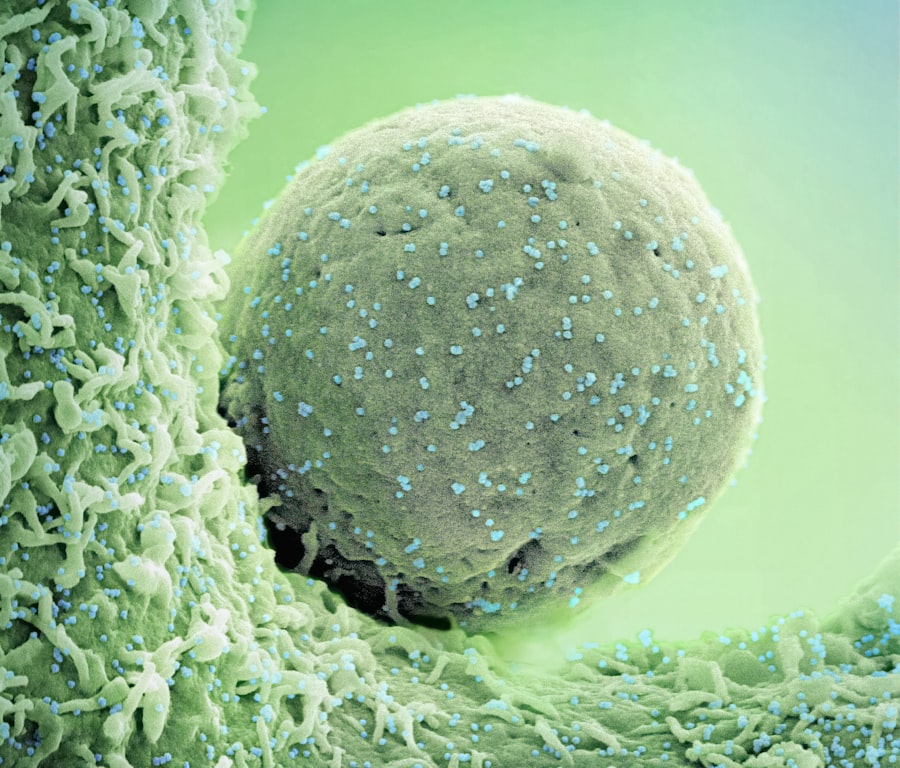
Bladder cancer is a significant health concern worldwide, ranking as the fourth most common cancer among men and the eighth among women in the United States. This malignancy originates in the bladder’s transitional cells, which line the bladder’s interior. The most prevalent form of bladder cancer is transitional cell carcinoma (TCC), accounting for approximately 90% of cases.
Other less common types include squamous cell carcinoma and adenocarcinoma. Risk factors for developing bladder cancer include smoking, exposure to certain chemicals, chronic bladder inflammation, and a family history of the disease. The symptoms often manifest as hematuria (blood in urine), frequent urination, and pelvic pain, prompting individuals to seek medical attention.
The diagnosis of bladder cancer typically involves a combination of imaging studies, such as CT scans or ultrasounds, and cystoscopy, where a thin tube with a camera is inserted into the bladder. Once diagnosed, the stage and grade of the cancer are determined, which are crucial for guiding treatment decisions. Staging ranges from superficial tumors confined to the bladder lining to invasive cancers that penetrate deeper layers or metastasize to distant organs.
Understanding these nuances is essential for both patients and healthcare providers as they navigate the complexities of treatment options available for bladder cancer.
Key Takeaways
- Bladder cancer treatment is evolving through ongoing clinical trials exploring new therapies.
- Current treatments include surgery, chemotherapy, immunotherapy, and radiation.
- Patient participation in clinical trials is crucial for advancing effective bladder cancer treatments.
- Challenges in trials include patient recruitment, side effects, and trial design complexities.
- Future research aims to improve outcomes with innovative therapies and personalized medicine approaches.
Current Treatment Options for Bladder Cancer
The treatment landscape for bladder cancer is multifaceted, primarily depending on the stage and grade of the tumor. For superficial bladder cancer, which is confined to the inner lining, intravesical therapy is often employed. This involves administering chemotherapy or immunotherapy directly into the bladder through a catheter.
Bacillus Calmette-Guérin (BCG) therapy is a well-established immunotherapy that has shown efficacy in preventing recurrence in patients with high-risk superficial tumors. BCG works by stimulating the immune system to attack cancer cells within the bladder. For muscle-invasive bladder cancer, treatment typically involves a more aggressive approach.
Radical cystectomy, which entails the surgical removal of the bladder along with surrounding tissues and lymph nodes, is often recommended. This procedure may be followed by urinary diversion methods to allow for normal urination post-surgery. In some cases, neoadjuvant chemotherapy is administered before surgery to shrink tumors and improve surgical outcomes.
Additionally, for patients who are not surgical candidates or prefer a non-invasive approach, systemic chemotherapy remains a viable option. The combination of cisplatin and gemcitabine is frequently used as a first-line treatment for advanced stages of the disease.
Importance of Clinical Trials in Advancing Bladder Cancer Treatment

Clinical trials play a pivotal role in advancing the understanding and treatment of bladder cancer. These studies are essential for evaluating new therapies, improving existing treatment protocols, and ultimately enhancing patient outcomes. By participating in clinical trials, patients gain access to cutting-edge treatments that may not yet be available through standard care pathways.
Moreover, clinical trials contribute significantly to the body of knowledge regarding the efficacy and safety of various interventions, helping to establish evidence-based practices in oncology. The process of clinical trials is meticulously designed to ensure patient safety while rigorously testing new hypotheses. Trials are typically conducted in phases, starting with small groups of participants to assess safety (Phase I), followed by larger groups to evaluate efficacy (Phase II), and finally comparing new treatments against standard care in large populations (Phase III).
This structured approach allows researchers to gather comprehensive data on how new therapies perform across diverse patient demographics and disease stages. The insights gained from these trials not only inform clinical practice but also guide regulatory approvals for new medications and treatment modalities.
Promising New Therapies in Bladder Cancer Clinical Trials
Recent advancements in bladder cancer research have led to the exploration of several promising new therapies currently undergoing clinical trials. One notable area of investigation is the use of immune checkpoint inhibitors, such as pembrolizumab and nivolumab. These agents work by blocking proteins that inhibit immune responses against cancer cells, thereby enhancing the body’s ability to fight tumors.
Early results from clinical trials have shown that these therapies can lead to durable responses in patients with advanced bladder cancer who have previously failed standard treatments. Another exciting avenue of research involves targeted therapies that focus on specific genetic mutations associated with bladder cancer. For instance, erdafitinib is an oral medication that targets fibroblast growth factor receptor (FGFR) alterations found in some bladder tumors.
Clinical trials have demonstrated its effectiveness in patients with metastatic bladder cancer harboring FGFR mutations, leading to significant tumor shrinkage in a subset of patients. Additionally, antibody-drug conjugates like enfortumab vedotin are being evaluated for their ability to deliver cytotoxic agents directly to cancer cells while minimizing damage to healthy tissues.
Patient Participation in Bladder Cancer Clinical Trials
| Trial Phase | Number of Trials | Primary Outcome Measures | Common Interventions | Average Enrollment | Trial Status |
|---|---|---|---|---|---|
| Phase 1 | 25 | Safety, Dosage, Side Effects | Immunotherapy, Chemotherapy | 30 | Recruiting/Completed |
| Phase 2 | 40 | Efficacy, Side Effects | Targeted Therapy, Immunotherapy | 80 | Recruiting/Completed |
| Phase 3 | 15 | Effectiveness, Safety | Combination Therapy, Surgery | 300 | Ongoing/Completed |
| Phase 4 | 5 | Long-term Effects, Quality of Life | Post-market Surveillance | 500 | Ongoing |
Patient participation in clinical trials is crucial for advancing bladder cancer research and improving treatment outcomes. Engaging patients in these studies not only provides them with access to innovative therapies but also empowers them to contribute to scientific knowledge that may benefit future generations. However, participation rates can be influenced by various factors, including patient awareness of available trials, perceived risks versus benefits, and logistical challenges such as travel requirements or time commitments.
To enhance participation rates, healthcare providers play a vital role in educating patients about ongoing clinical trials and addressing any concerns they may have regarding participation. Open discussions about potential side effects, the nature of the trial, and how it fits into their overall treatment plan can help demystify the process for patients. Furthermore, initiatives aimed at increasing diversity in clinical trial populations are essential to ensure that findings are applicable across different demographics and that all patients have equitable access to emerging therapies.
Challenges and Considerations in Conducting Bladder Cancer Clinical Trials
Conducting clinical trials for bladder cancer presents several challenges that researchers must navigate carefully. One significant hurdle is patient recruitment; finding eligible participants who meet specific criteria can be time-consuming and may delay trial timelines. Additionally, many patients may be hesitant to enroll due to fears about potential side effects or concerns about receiving a placebo instead of active treatment.
Another consideration is the complexity of bladder cancer itself, which can exhibit considerable heterogeneity among patients. Variations in tumor biology, genetic mutations, and responses to treatment necessitate tailored approaches in trial design and analysis. Researchers must account for these differences when interpreting results and determining the applicability of findings across diverse patient populations.
Furthermore, regulatory hurdles can complicate trial initiation and execution; obtaining necessary approvals from ethics boards and regulatory agencies requires meticulous planning and adherence to stringent guidelines.
Future Directions in Bladder Cancer Research and Clinical Trials
The future of bladder cancer research is poised for exciting developments as scientists continue to explore novel therapeutic strategies and refine existing treatments through clinical trials. One promising direction involves the integration of precision medicine approaches that leverage genetic profiling to tailor treatments based on individual tumor characteristics. By identifying specific mutations or biomarkers associated with bladder cancer, clinicians can select targeted therapies that are more likely to yield positive outcomes for each patient.
Additionally, there is growing interest in combining different therapeutic modalities to enhance treatment efficacy. For instance, combining immune checkpoint inhibitors with chemotherapy or targeted therapies may lead to synergistic effects that improve overall survival rates. Ongoing clinical trials are investigating these combination strategies, aiming to identify optimal regimens that maximize benefits while minimizing adverse effects.
Moreover, advancements in technology are revolutionizing how clinical trials are conducted. The use of digital health tools and telemedicine has expanded access to trials for patients who may face barriers related to travel or mobility. Remote monitoring and virtual visits can facilitate participation while ensuring patient safety during treatment evaluation.
The Impact of Clinical Trials on Bladder Cancer Treatment
Clinical trials represent a cornerstone of progress in bladder cancer treatment, driving innovation and improving patient outcomes through rigorous scientific inquiry. As researchers continue to explore new therapies and refine existing approaches, the importance of patient participation cannot be overstated; it is through their involvement that breakthroughs are made possible. The challenges inherent in conducting these trials underscore the need for ongoing collaboration among researchers, healthcare providers, and patients alike.
The future holds great promise for bladder cancer research as emerging therapies and novel treatment strategies continue to evolve. With an emphasis on precision medicine and innovative trial designs, there is hope for more effective treatments that can significantly enhance survival rates and quality of life for those affected by this disease. As we look ahead, it is clear that clinical trials will remain integral to shaping the landscape of bladder cancer care and ensuring that patients receive the best possible options available.