Clinical research trials constitute the fundamental framework of contemporary medicine, functioning as the principal mechanism for assessing the safety and effectiveness of novel treatments, pharmaceuticals, and medical devices. These trials represent carefully structured studies involving human subjects, executed systematically to collect data that advances healthcare knowledge and practice. This process proves essential not only for developing new therapeutic interventions but also for verifying that current treatments remain safe and effective for target patient populations.
The progression from laboratory research to clinical implementation involves multiple stages and demands comprehensive testing through sequential phases of clinical investigation. Clinical trials serve purposes that extend beyond regulatory approval of new medications. They provide critical insights into disease pathophysiology, reveal potential adverse effects, and establish optimal therapeutic dosing protocols.
Each phase of investigation builds systematically upon previous findings, establishing a robust evidence-based framework that directs researchers toward improved patient outcomes. Clinical trials therefore represent both a regulatory necessity and an ethical imperative, ensuring that new therapeutic interventions demonstrate clear benefits that outweigh potential risks for patients.
Key Takeaways
- Clinical research trials progress through phases 0 to IV, each focusing on different aspects like safety, dosage, efficacy, and long-term effects.
- Early phases (0 and I) primarily assess safety and appropriate dosage levels for new treatments.
- Phase II and III trials evaluate treatment effectiveness and compare new therapies to existing standards.
- Phase IV trials monitor treatments post-approval to identify long-term effects and ensure ongoing safety.
- Informed consent, ethical considerations, and regulatory approvals are critical to protecting participants and ensuring trial integrity.
Phase 0 and Phase I Trials: Exploring Safety and Dosage
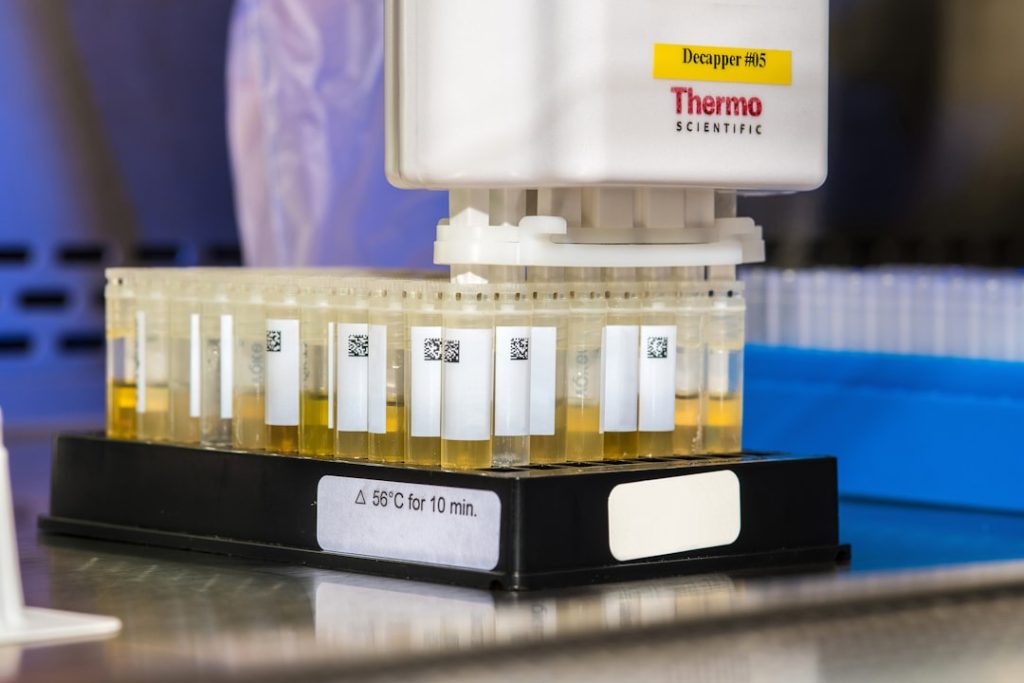
Phase 0 trials, often referred to as “microdosing” studies, represent an innovative approach in clinical research. These trials involve administering a very small dose of a drug to a limited number of participants, typically fewer than 15, to gather preliminary data on pharmacokinetics and pharmacodynamics. The primary goal is to understand how the drug behaves in the human body without exposing participants to significant risk.
For instance, a Phase 0 trial might involve a novel cancer drug that has shown promise in preclinical studies. By observing how the drug is absorbed, distributed, metabolized, and excreted in humans, researchers can make informed decisions about whether to proceed to larger trials. Phase I trials follow Phase 0 and are primarily concerned with assessing the safety of a new treatment.
These trials usually involve a larger group of participants, often ranging from 20 to 100 healthy volunteers or patients with the condition being studied. The focus is on determining the maximum tolerated dose (MTD) and identifying any adverse effects associated with the treatment. For example, in a Phase I trial for a new chemotherapy agent, researchers would gradually increase the dosage given to participants while closely monitoring for side effects such as nausea, fatigue, or more severe reactions.
This phase is critical as it lays the groundwork for subsequent trials by establishing safe dosage ranges and identifying potential toxicity.
Phase II Trials: Assessing Efficacy and Side Effects

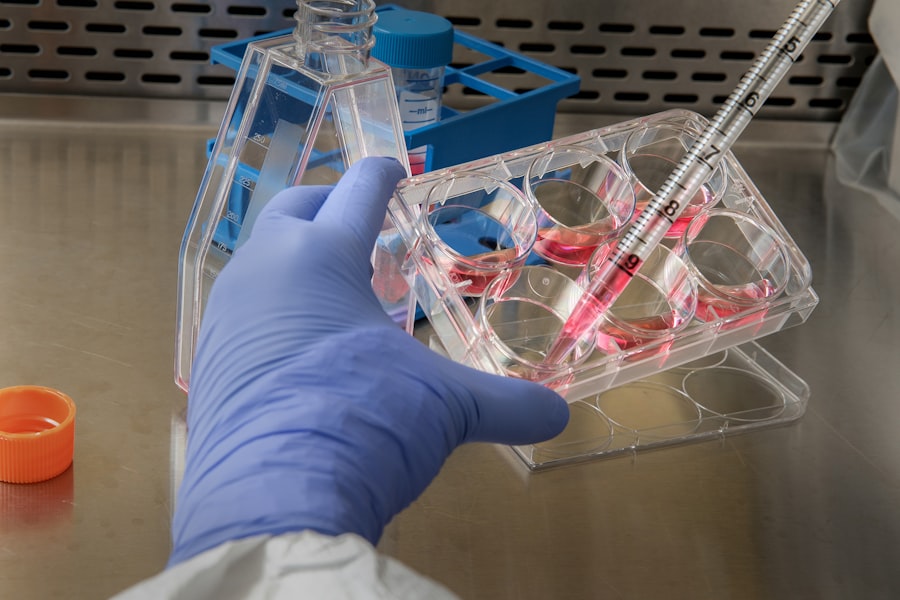
Once a treatment has successfully passed through Phase I trials, it enters Phase II, where the focus shifts from safety to efficacy. This phase typically involves several hundred participants and aims to determine whether the treatment has a beneficial effect on the targeted condition. Researchers will often use specific endpoints, such as tumor shrinkage in cancer patients or improvement in symptoms for chronic diseases, to measure efficacy.
For instance, in a Phase II trial for a new antidepressant, researchers might assess changes in patients’ mood scores over several weeks to evaluate whether the drug provides significant relief compared to a placebo. In addition to efficacy, Phase II trials continue to monitor side effects and adverse reactions. This dual focus is essential because while a treatment may show promise in alleviating symptoms or improving health outcomes, it must also be safe for widespread use.
Researchers collect detailed data on any adverse events reported by participants, which can range from mild side effects like headaches to more serious complications that could impact patient safety. The information gathered during this phase is crucial for refining treatment protocols and determining whether the drug should advance to Phase III trials.
Phase III Trials: Comparing New Treatment to Standard of Care
Phase III trials are often considered the most critical stage in the clinical trial process, as they involve large populations and are designed to compare the new treatment against the current standard of care. These trials typically enroll thousands of participants across multiple sites and are randomized and controlled to minimize bias. The primary objective is to provide definitive evidence regarding the efficacy and safety of the new treatment compared to existing therapies.
For example, in a Phase III trial for a new diabetes medication, researchers would compare blood sugar control in patients receiving the new drug against those receiving an established treatment. The design of Phase III trials can vary significantly depending on the condition being studied and the treatment being tested. Some trials may use a placebo control group, while others may compare two active treatments head-to-head.
The results from these trials are pivotal; they not only inform regulatory agencies about whether a drug should be approved for public use but also guide clinical practice by providing evidence-based recommendations for healthcare providers. The data collected during this phase can lead to changes in treatment guidelines and influence how diseases are managed on a broader scale.
Phase IV Trials: Post-Market Surveillance and Long-Term Effects
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 0 | Microdosing to understand pharmacodynamics and pharmacokinetics | 10-15 | Several months | Safety and biological activity | Varies |
| Phase I | Assess safety, dosage range, and side effects | 20-100 healthy volunteers | Several months | Safety and dosage | 70% |
| Phase II | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Efficacy and side effects | 33% |
| Phase III | Confirm effectiveness, monitor adverse reactions, compare to standard treatments | 1,000-3,000 patients | 1-4 years | Effectiveness and safety | 25-30% |
| Phase IV | Post-marketing surveillance to detect long-term effects | Various (thousands) | Ongoing | Long-term safety and effectiveness | N/A |
Phase IV trials occur after a treatment has received regulatory approval and is available on the market. These post-marketing studies are essential for monitoring long-term effects and gathering additional data on safety and efficacy in diverse populations over extended periods. While Phase III trials provide valuable insights into how a drug performs in controlled environments, Phase IV trials assess its performance in real-world settings where patient demographics and comorbidities may differ significantly from those in earlier trials.
For instance, after a new cardiovascular drug is approved, Phase IV studies may reveal rare side effects that were not apparent during earlier phases due to limited sample sizes or shorter follow-up periods. These studies can also help identify specific populations that may benefit more from the treatment or those who may be at higher risk for adverse effects. Regulatory agencies often require these post-marketing studies as part of their commitment to ensuring ongoing patient safety and effective treatment options.
Understanding Informed Consent and Ethical Considerations
Informed consent is a fundamental ethical principle in clinical research that ensures participants are fully aware of what their involvement entails before agreeing to participate in a trial. This process involves providing potential participants with comprehensive information about the study’s purpose, procedures, risks, benefits, and their rights as participants. It is crucial that this information is presented in clear language that is easily understandable, allowing individuals to make informed decisions about their participation.
Ethical considerations extend beyond informed consent; they encompass issues such as participant selection, risk minimization, and equitable access to trials. Researchers must ensure that vulnerable populations are not exploited and that all participants have equal opportunities to benefit from advancements in medical research. Institutional Review Boards (IRBs) play a vital role in overseeing clinical trials by reviewing study protocols to ensure ethical standards are upheld throughout the research process.
Navigating the Regulatory Approval Process
The regulatory approval process for new treatments is complex and varies by country but generally involves several key steps designed to ensure that new therapies are safe and effective before they reach the market. In the United States, for example, the Food and Drug Administration (FDA) oversees this process. After completing all necessary clinical trial phases, sponsors submit a New Drug Application (NDA) or Biologics License Application (BLA) that includes comprehensive data from all phases of testing.
The FDA reviews this data meticulously, assessing both efficacy and safety profiles before making a decision on approval. This review process can take several months or even years, depending on the complexity of the data submitted and any additional information requested by regulatory officials. In some cases, expedited pathways such as Breakthrough Therapy Designation or Fast Track status may be available for treatments addressing unmet medical needs or serious conditions, allowing for faster access to potentially life-saving therapies.
The Role of Participants and the Importance of Clinical Trial Participation
Participants play an indispensable role in clinical research trials; without their willingness to volunteer, advancements in medicine would be severely hindered. Each participant contributes valuable data that can lead to breakthroughs in understanding diseases and developing new treatments. Their involvement not only helps researchers gather essential information but also provides an opportunity for individuals to access cutting-edge therapies that may not yet be available through standard care.
Moreover, participation in clinical trials can empower individuals by giving them an active role in their healthcare journey. Many participants report feeling a sense of purpose knowing they are contributing to scientific knowledge that could benefit future patients. However, it is essential for potential participants to weigh the risks and benefits carefully before enrolling in a trial.
Understanding what participation entails—such as time commitments, potential side effects, and the nature of randomization—can help individuals make informed choices about their involvement in clinical research. In conclusion, clinical research trials are an intricate yet vital component of medical advancement. From initial safety assessments in Phase I trials through post-marketing surveillance in Phase IV studies, each phase serves a distinct purpose in ensuring that new treatments are both effective and safe for public use.
Ethical considerations surrounding informed consent and participant rights remain paramount throughout this process, underscoring the importance of transparency and respect for individuals who contribute their time and health to advance medical science.