Clinical trials are a cornerstone of modern medical research, serving as the primary method for evaluating the safety and efficacy of new treatments, drugs, and medical devices. These meticulously designed studies are essential for determining whether a new intervention is effective and safe for human use before it can be approved for widespread clinical application. The process of clinical trials is governed by strict regulatory frameworks and ethical guidelines to ensure the protection of participants and the integrity of the data collected.
As the landscape of medicine continues to evolve, clinical trials remain pivotal in translating scientific discoveries into tangible health benefits. The journey of a new treatment from the laboratory bench to the patient’s bedside is fraught with challenges, and clinical trials play a critical role in navigating this complex pathway. They are typically categorized into distinct phases, each with specific objectives and methodologies.
This structured approach allows researchers to gather comprehensive data on a treatment’s effects, identify potential side effects, and ultimately determine its viability as a therapeutic option. The importance of clinical trials cannot be overstated; they not only contribute to the advancement of medical knowledge but also provide hope for patients with conditions that currently lack effective treatments.
Key Takeaways
- Clinical trials progress through phases I to IV, each focusing on safety, efficacy, comparison, and post-market monitoring.
- Phase I trials primarily assess safety and dosage in a small group of participants.
- Phase II and III trials evaluate treatment effectiveness and compare new therapies to existing standards.
- Phase IV trials monitor long-term effects and safety after a treatment is approved.
- Ethical, regulatory, and participant considerations are crucial for the integrity and success of clinical trials.
Phase I Clinical Trials: Exploring Safety and Dosage
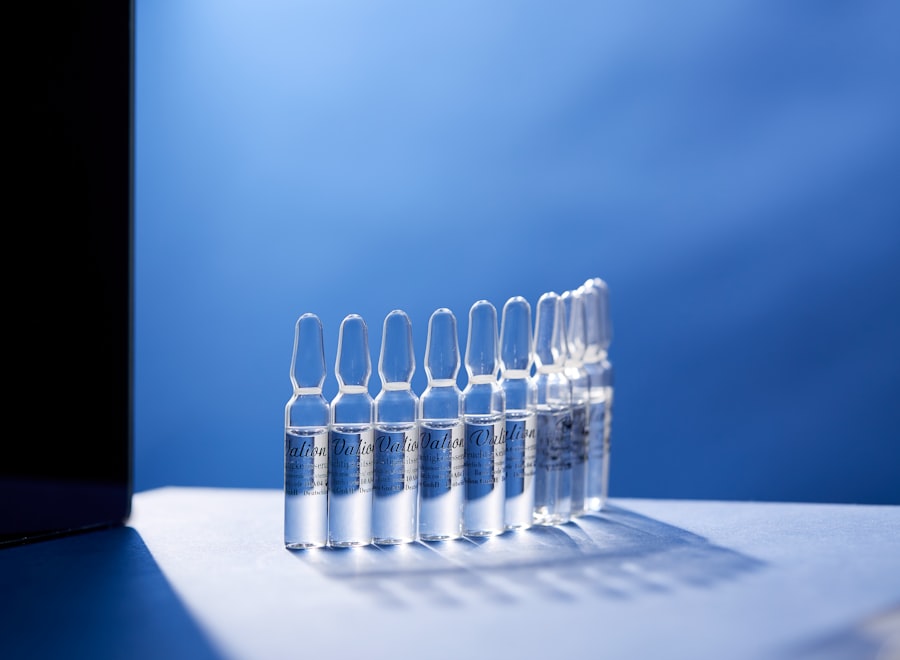
Phase I clinical trials are the first step in testing a new drug or treatment in humans, primarily focusing on safety and dosage. These trials typically involve a small group of healthy volunteers or patients, usually ranging from 20 to 100 participants. The primary goal is to assess how the drug is metabolized and excreted by the body, as well as to identify any potential side effects.
Researchers carefully monitor participants for adverse reactions, which can provide critical insights into the drug’s safety profile. In addition to safety assessments, Phase I trials also aim to establish the optimal dosage range for further testing. This involves administering varying doses of the drug to different groups within the trial to determine which dose produces the desired therapeutic effect with minimal side effects.
For instance, in a Phase I trial for a new cancer drug, researchers might start with a low dose and gradually increase it while closely monitoring participants for any adverse reactions. This iterative process helps to identify the maximum tolerated dose, which will be crucial for subsequent phases of testing.
Phase II Clinical Trials: Assessing Efficacy and Side Effects

Once a treatment has successfully passed Phase I trials, it progresses to Phase II, where the focus shifts from safety to efficacy. This phase typically involves a larger group of participants, often ranging from 100 to 300 individuals who have the condition that the treatment aims to address. The primary objective of Phase II trials is to evaluate whether the treatment is effective in producing a beneficial effect on the disease or condition being studied.
In addition to assessing efficacy, Phase II trials continue to monitor participants for side effects, providing valuable data on the treatment’s safety profile as it is used in a larger population. For example, in a Phase II trial for a new antidepressant, researchers would not only measure improvements in depressive symptoms but also track any adverse effects experienced by participants. This dual focus allows researchers to refine their understanding of the treatment’s therapeutic window—the range of doses that provide efficacy without unacceptable side effects—before moving on to larger-scale testing in Phase
Phase III Clinical Trials: Comparing New Treatment to Standard of Care
| Phase | Purpose | Number of Participants | Duration | Key Focus | Success Rate |
|---|---|---|---|---|---|
| Phase 1 | Assess safety and dosage | 20-100 healthy volunteers | Several months | Safety, side effects, pharmacokinetics | 70% |
| Phase 2 | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Effectiveness, optimal dose | 33% |
| Phase 3 | Confirm effectiveness and monitor adverse reactions | 1,000-3,000 patients | 1-4 years | Comparison with standard treatments | 25-30% |
| Phase 4 | Post-marketing surveillance | Various (thousands) | Ongoing | Long-term effects, rare side effects | N/A |
Phase III clinical trials represent a critical juncture in the development of new treatments, as they involve large-scale testing designed to compare the new intervention against the current standard of care. These trials typically enroll hundreds to thousands of participants across multiple sites, providing a robust dataset that can yield statistically significant results. The primary aim is to determine whether the new treatment offers a meaningful benefit over existing therapies in terms of efficacy, safety, and overall patient outcomes.
In these trials, participants are often randomly assigned to receive either the new treatment or the standard therapy, which helps eliminate bias and ensures that any observed differences in outcomes can be attributed to the treatment itself rather than other variables. For instance, in a Phase III trial evaluating a new medication for diabetes management, researchers would compare blood sugar control between patients receiving the new drug and those receiving established treatments. The results from Phase III trials are crucial for regulatory approval; they provide the evidence needed for health authorities like the FDA or EMA to assess whether the new treatment should be made available to the public.
Phase IV Clinical Trials: Post-Market Surveillance
Phase IV clinical trials occur after a treatment has received regulatory approval and is available on the market. These studies are essential for ongoing monitoring of the drug’s long-term safety and effectiveness in a broader population. While earlier phases focus on controlled environments with selected participants, Phase IV trials often involve diverse patient populations that reflect real-world conditions.
This phase aims to identify any rare or long-term side effects that may not have been evident during earlier trials due to limited sample sizes or shorter follow-up periods. For example, after a vaccine is approved for public use, Phase IV studies may be conducted to monitor its effectiveness across different demographics and geographic regions. These studies can reveal important information about how well the vaccine works in various populations and whether any unexpected adverse events occur over time.
Additionally, Phase IV trials can help identify potential drug interactions when patients are taking multiple medications, providing critical insights that can inform clinical practice and patient safety.
Key Considerations for Participants in Clinical Trials
Participating in a clinical trial can be an important decision for individuals seeking new treatment options or contributing to medical research. However, potential participants should carefully consider several factors before enrolling. One key consideration is understanding the purpose and design of the trial.
Participants should be informed about what is expected of them, including any procedures they will undergo, how long the trial will last, and what types of data will be collected. Informed consent is another crucial aspect of participation in clinical trials. Participants must be provided with comprehensive information about the risks and benefits associated with the trial, allowing them to make an educated decision about their involvement.
It is essential for individuals to feel comfortable asking questions and seeking clarification about any uncertainties they may have regarding their participation. Additionally, potential participants should consider their eligibility based on inclusion and exclusion criteria outlined by researchers, as these criteria are designed to ensure participant safety and data integrity.
Ethical and Regulatory Considerations in Clinical Trials
The ethical conduct of clinical trials is paramount in ensuring participant safety and maintaining public trust in medical research. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) establish guidelines that govern how clinical trials should be conducted.
These regulations require that trials adhere to principles such as respect for persons, beneficence, and justice—ensuring that participants are treated ethically and fairly throughout the research process. One significant ethical consideration is ensuring that participants are not subjected to undue risk. Researchers must weigh potential benefits against possible harms when designing studies and must implement rigorous monitoring protocols to safeguard participant welfare.
Additionally, ethical review boards or institutional review boards (IRBs) play a critical role in overseeing clinical trials by reviewing study protocols before they begin. These boards assess whether studies meet ethical standards and whether informed consent processes are adequate, ensuring that participant rights are protected throughout the trial.
The Importance of Clinical Trials in Advancing Medicine
Clinical trials are indispensable in advancing medical science and improving patient care. They provide a systematic approach to evaluating new treatments that can lead to breakthroughs in disease management and prevention strategies. By rigorously testing hypotheses through well-designed studies, researchers can generate evidence-based conclusions that inform clinical practice guidelines and shape healthcare policies.
Moreover, clinical trials contribute significantly to our understanding of diseases themselves. They often uncover new insights into disease mechanisms, identify biomarkers for patient stratification, and pave the way for personalized medicine approaches tailored to individual patient needs. As medicine continues to evolve with advancements in technology and scientific knowledge, clinical trials will remain at the forefront of innovation—driving progress toward more effective therapies and improved health outcomes for patients worldwide.



