Bladder cancer is a significant health concern worldwide, ranking as the fourth most common cancer among men and the eighth among women in the United States. The disease originates in the bladder’s transitional cells, which line the bladder’s interior and are responsible for its ability to stretch and contract. The most prevalent form of bladder cancer is transitional cell carcinoma (TCC), accounting for approximately 90% of cases.
Other less common types include squamous cell carcinoma and adenocarcinoma. Risk factors for developing bladder cancer include smoking, exposure to certain chemicals, chronic bladder inflammation, and a family history of the disease. The symptoms often manifest as hematuria (blood in urine), frequent urination, and pelvic pain, prompting individuals to seek medical attention.
The diagnosis of bladder cancer typically involves a combination of imaging studies, such as ultrasound or CT scans, and cystoscopy, where a thin tube with a camera is inserted into the bladder to visualize any abnormalities. Once diagnosed, the stage of the cancer is determined, which is crucial for deciding on the appropriate treatment strategy. Staging ranges from superficial tumors confined to the bladder lining to invasive cancers that penetrate deeper layers or metastasize to distant organs.
Understanding the complexity of bladder cancer is essential for both patients and healthcare providers as they navigate treatment options and consider participation in clinical trials aimed at improving outcomes.
Key Takeaways
- Bladder cancer treatment is evolving with new therapies emerging from recent clinical trials.
- Standard treatments include surgery, chemotherapy, and immunotherapy, but novel approaches show promise.
- Patient eligibility criteria are crucial for clinical trial participation and impact recruitment success.
- Participating in trials offers potential benefits but also carries risks that patients should carefully consider.
- Ongoing research and resources are available to support patients interested in exploring clinical trial options.
Current Standard Treatment for Bladder Cancer
The standard treatment for bladder cancer varies significantly based on the stage and grade of the tumor. For superficial bladder cancer, which is confined to the inner lining, transurethral resection of bladder tumor (TURBT) is often the first-line treatment. This minimally invasive procedure involves removing the tumor through the urethra, allowing for immediate pathological evaluation.
Following TURBT, intravesical therapy may be employed, where medications such as Bacillus Calmette-Guérin (BCG) or chemotherapy agents are directly instilled into the bladder to reduce recurrence rates. For muscle-invasive bladder cancer, radical cystectomy is frequently recommended. This surgical procedure entails the removal of the entire bladder along with surrounding tissues and lymph nodes.
In some cases, neoadjuvant chemotherapy may be administered before surgery to shrink tumors and improve surgical outcomes. Post-surgery, patients may require additional treatments such as chemotherapy or radiation therapy to eliminate any remaining cancer cells. The choice of treatment is influenced by various factors, including the patient’s overall health, preferences, and specific tumor characteristics.
Overview of Recent Clinical Trials for Bladder Cancer
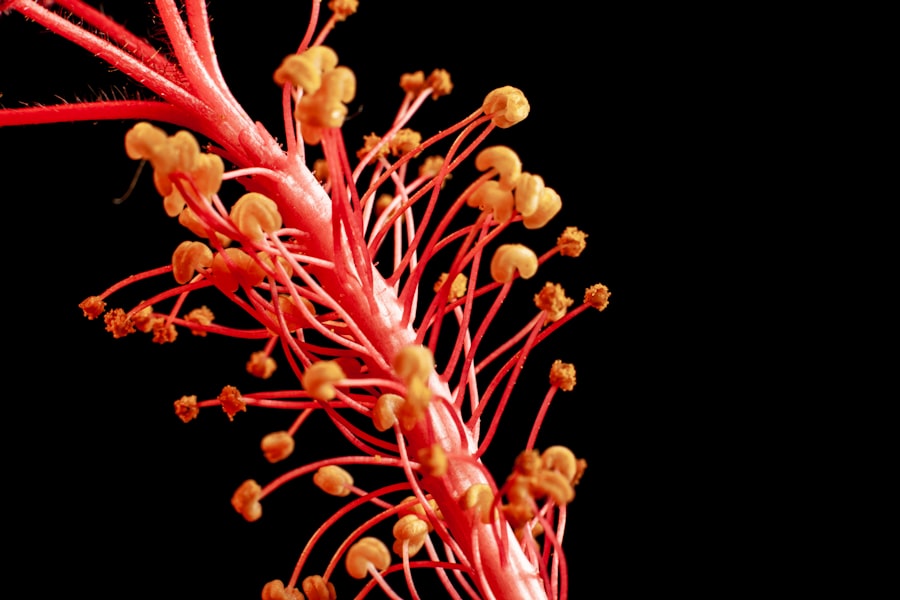
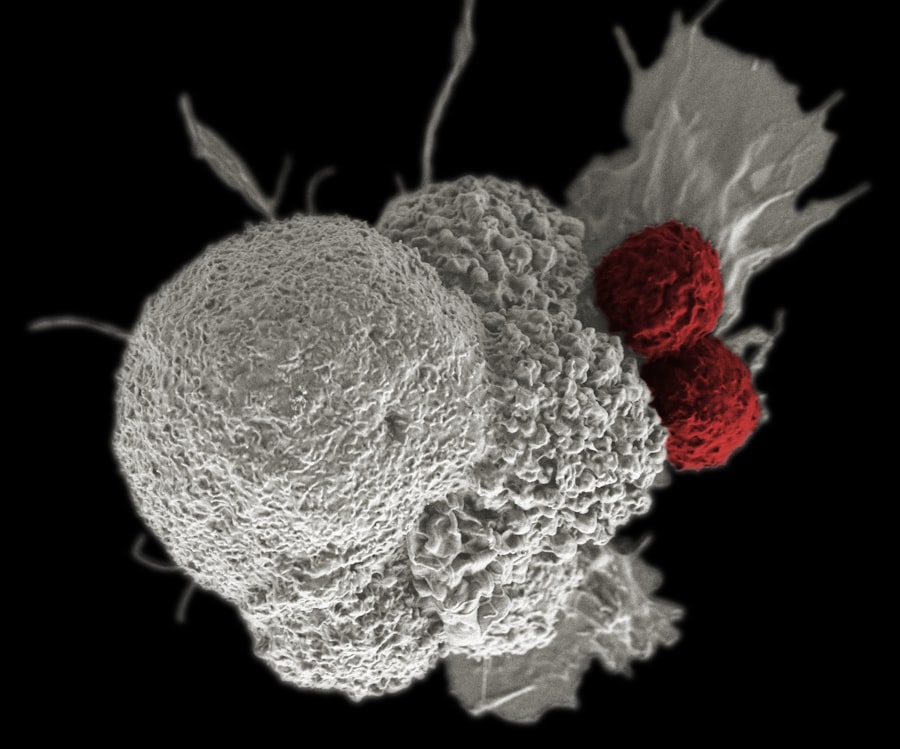
Recent clinical trials have been pivotal in advancing our understanding and treatment of bladder cancer. These trials often explore new drugs, combinations of existing therapies, or novel approaches such as immunotherapy. For instance, studies investigating immune checkpoint inhibitors like pembrolizumab and nivolumab have shown promise in treating advanced bladder cancer by enhancing the body’s immune response against tumor cells.
These agents target proteins that inhibit immune activation, allowing T-cells to recognize and attack cancer cells more effectively. Additionally, ongoing trials are examining the efficacy of targeted therapies that focus on specific genetic mutations associated with bladder cancer. For example, trials involving erdafitinib have demonstrated effectiveness in patients with FGFR3 mutations, leading to significant tumor shrinkage in some cases.
The landscape of clinical trials is continually evolving, with researchers exploring combinations of therapies to enhance efficacy while minimizing side effects. The results from these trials not only contribute to the development of new treatment protocols but also provide valuable insights into patient responses and long-term outcomes.
Promising New Therapies and Treatment Approaches
The landscape of bladder cancer treatment is rapidly changing with the introduction of promising new therapies and innovative approaches. One notable advancement is the use of immunotherapy, which harnesses the body’s immune system to fight cancer more effectively. Agents such as atezolizumab and durvalumab have been approved for use in patients with advanced or metastatic bladder cancer who have previously undergone chemotherapy.
These therapies have shown significant improvements in overall survival rates compared to traditional treatments. In addition to immunotherapy, researchers are investigating combination therapies that pair immunotherapeutic agents with chemotherapy or targeted therapies. This approach aims to enhance treatment efficacy by attacking cancer cells through multiple mechanisms simultaneously.
For instance, combining checkpoint inhibitors with chemotherapy has shown synergistic effects in clinical trials, leading to improved response rates in patients with muscle-invasive bladder cancer. Furthermore, ongoing research into personalized medicine—tailoring treatments based on individual genetic profiles—holds great promise for optimizing therapeutic outcomes in bladder cancer patients.
Patient Eligibility and Recruitment for Clinical Trials
| Trial Phase | Number of Trials | Primary Endpoint | Common Interventions | Average Enrollment | Trial Status |
|---|---|---|---|---|---|
| Phase 1 | 25 | Safety and Dosage | Immunotherapy, Chemotherapy | 40 | Recruiting/Active |
| Phase 2 | 40 | Efficacy and Side Effects | Targeted Therapy, Immunotherapy | 80 | Recruiting/Active |
| Phase 3 | 30 | Effectiveness and Monitoring | Combination Therapy, Surgery | 300 | Recruiting/Active/Completed |
| Phase 4 | 10 | Post-Marketing Surveillance | Approved Drugs | 500 | Completed |
Patient eligibility for clinical trials is a critical aspect that ensures the safety and efficacy of new treatments being tested. Each trial has specific inclusion and exclusion criteria based on factors such as age, overall health status, previous treatments received, and specific characteristics of the cancer itself. For example, some trials may focus exclusively on patients with metastatic disease who have not responded to standard therapies, while others may target those with early-stage tumors.
Recruitment for clinical trials can be challenging due to various factors including patient awareness and misconceptions about clinical research. Many patients may be hesitant to participate due to fears about potential side effects or a lack of understanding regarding the trial process. To address these concerns, healthcare providers play a crucial role in educating patients about the benefits and risks associated with clinical trial participation.
Additionally, organizations dedicated to bladder cancer research often provide resources and support to help patients navigate their options and make informed decisions about participating in clinical trials.
Potential Benefits and Risks of Participating in Clinical Trials
Participating in clinical trials offers several potential benefits for patients with bladder cancer. One significant advantage is access to cutting-edge therapies that may not yet be available through standard treatment protocols. Patients enrolled in trials often receive close monitoring from healthcare professionals, which can lead to early detection of any adverse effects or complications associated with new treatments.
Moreover, participation contributes to advancing medical knowledge and improving future treatment options for others facing similar diagnoses. However, there are inherent risks associated with clinical trial participation that patients must consider carefully. New therapies may not be as effective as anticipated or could lead to unforeseen side effects that are not yet fully understood.
Additionally, some trials may involve randomization into control groups receiving placebo treatments or standard care rather than experimental therapies. This uncertainty can be daunting for patients who are eager for effective treatment options. It is essential for patients to have open discussions with their healthcare providers about these risks and benefits before making a decision regarding participation in a clinical trial.
Future Directions in Bladder Cancer Research
The future of bladder cancer research is poised for significant advancements as scientists continue to explore innovative treatment modalities and improve patient outcomes. One promising direction involves the integration of genomic profiling into clinical practice, allowing for more personalized treatment approaches based on individual tumor characteristics. By identifying specific genetic mutations or alterations within tumors, researchers can tailor therapies that target these unique features more effectively.
Additionally, there is growing interest in understanding the tumor microenvironment and its role in bladder cancer progression and treatment resistance. Investigating how immune cells interact with tumor cells can provide insights into developing combination therapies that enhance immune responses while overcoming resistance mechanisms. Furthermore, advancements in technology such as artificial intelligence and machine learning are being leveraged to analyze large datasets from clinical trials and patient records, potentially identifying new biomarkers for early detection and treatment response prediction.
Resources for Patients Interested in Clinical Trials
For patients interested in exploring clinical trial options for bladder cancer, numerous resources are available to facilitate their journey. The National Cancer Institute (NCI) provides a comprehensive database of ongoing clinical trials across various cancer types, including bladder cancer. Patients can search for trials based on specific criteria such as location, eligibility requirements, and treatment focus.
Additionally, organizations such as the Bladder Cancer Advocacy Network (BCAN) offer valuable information about clinical trials along with support services for patients and their families. These organizations often host educational events and webinars that provide insights into emerging research and treatment options. Engaging with support groups can also help patients connect with others who have navigated similar experiences, fostering a sense of community while empowering them to make informed decisions about their care options.
In conclusion, navigating the complexities of bladder cancer requires a multifaceted approach that encompasses understanding current treatments, exploring innovative research avenues, and considering participation in clinical trials as a viable option for improving outcomes. As research continues to evolve, patients are encouraged to stay informed about emerging therapies and resources available to them on their journey toward recovery.




