The landscape of cancer treatment is in constant flux, a testament to ongoing research and the incremental, yet significant, progress made in understanding and combating this complex disease. Clinical trials serve as the crucible where theoretical breakthroughs are tested, refined, and ultimately translated into tangible benefits for patients. This article explores recent advancements highlighted by these trials, offering a realistic perspective on their potential impact.
Precision medicine, often likened to a meticulously crafted key fitting a specific lock, represents a fundamental reorientation in cancer therapy. No longer is treatment a one-size-fits-all approach. Instead, it leverages an individual’s genetic makeup and the molecular characteristics of their tumor to tailor interventions. This targeted strategy aims to maximize efficacy while minimizing collateral damage to healthy tissues.
Genomic Profiling and Biomarker Identification
At the core of precision medicine lies comprehensive genomic profiling. This involves analyzing a patient’s tumor DNA and RNA to identify specific genetic mutations, fusions, or amplifications that drive cancer growth. These alterations act as biomarkers, guiding the selection of targeted therapies. For instance, the presence of an EGFR mutation in non-small cell lung cancer directs the use of EGFR inhibitors, a treatment strategy that has markedly improved patient outcomes compared to conventional chemotherapy in these specific subsets.
Targeted Therapies: Beyond General Cytotoxicity
Traditional chemotherapy operates like a broad-spectrum antibiotic, often harming healthy cells alongside cancerous ones. Targeted therapies, conversely, are designed to interrupt specific molecular pathways crucial for cancer cell survival and proliferation. Recent clinical trials have showcased the effectiveness of various new targeted agents. For example, PARP inhibitors have demonstrated significant benefit in patients with BRCA-mutated ovarian and breast cancers, by exploiting the cancer cells’ compromised DNA repair mechanisms. Similarly, BRAF inhibitors have revolutionized the treatment of metastatic melanoma with BRAF mutations.
Immunotherapy: Unleashing the Body’s Defenses
Immunotherapy has emerged as a powerful pillar in cancer treatment, shifting the focus from directly attacking cancer cells to empowering the patient’s own immune system to do so. This approach recognizes that cancer often develops by evading immune surveillance, and seeks to restore or enhance this natural defense mechanism.
Checkpoint Inhibitors: Lifting the Brakes on the Immune System
Immune checkpoints are molecular pathways that regulate the immune response, preventing it from attacking healthy tissues. Cancer cells often hijack these checkpoints to escape detection and destruction by the immune system. Checkpoint inhibitors, such as PD-1, PD-L1, and CTLA-4 inhibitors, act by blocking these inhibitory signals, effectively “lifting the brakes” on the immune system and allowing it to launch an attack against cancer. Clinical trials have expanded the application of these drugs across numerous cancer types, including melanoma, lung cancer, renal cell carcinoma, and certain lymphomas, often leading to durable responses in a subset of patients.
CAR T-Cell Therapy: Reprogramming Immune Cells
Chimeric Antigen Receptor (CAR) T-cell therapy represents a more personalized form of immunotherapy. It involves extracting a patient’s T-cells, engineering them in a laboratory to express a CAR protein that recognizes specific antigens on cancer cells, and then reinfusing these “super-charged” T-cells back into the patient. This technology is analogous to designing a highly specific guided missile to target cancer. Initially approved for certain blood cancers like relapsed or refractory acute lymphoblastic leukemia and large B-cell lymphoma, CAR T-cell therapy continues to be investigated for solid tumors, although challenges remain in this area.
Advanced Radiation Oncology Techniques
While radiation therapy has been a cornerstone of cancer treatment for decades, continuous technological advancements have refined its precision and reduced its toxicity. These improvements aim to deliver a higher, more conformal dose to the tumor while sparing surrounding healthy tissues.
Stereotactic Body Radiation Therapy (SBRT) and Stereotactic Radiosurgery (SRS)
SBRT and SRS involve delivering very high doses of radiation in a small number of fractions (typically 1-5) to precisely defined tumors. This precision is achieved through sophisticated imaging and treatment planning systems that allow for sub-millimeter accuracy. Think of it as using a laser scalpel instead of a broad blade. Clinical trials have demonstrated the efficacy of SBRT for early-stage lung cancer, liver metastases, and prostate cancer, often offering a less invasive alternative to surgery. SRS, a similar technique, is primarily used for brain tumors and other lesions within the skull.
Proton Therapy: A Reduced Exit Dose
Proton therapy utilizes protons instead of photons (X-rays) for radiation delivery. Protons deposit most of their energy at a specific depth, known as the Bragg peak, before rapidly falling to zero. This characteristic results in a significantly reduced “exit dose” compared to photon therapy, meaning less radiation is delivered to tissues beyond the tumor. This advantage is particularly beneficial for treating cancers in sensitive locations, such as pediatric cancers, brain tumors, and head and neck cancers, where minimizing radiation exposure to healthy tissues is paramount to reducing long-term side effects. Ongoing clinical trials are further evaluating its cost-effectiveness and long-term outcomes compared to conventional radiotherapy.
Emerging Therapies and Future Directions

The field of oncology is a rapidly evolving domain, with numerous novel approaches under investigation. The journey from bench to bedside is arduous, but the potential rewards are substantial.
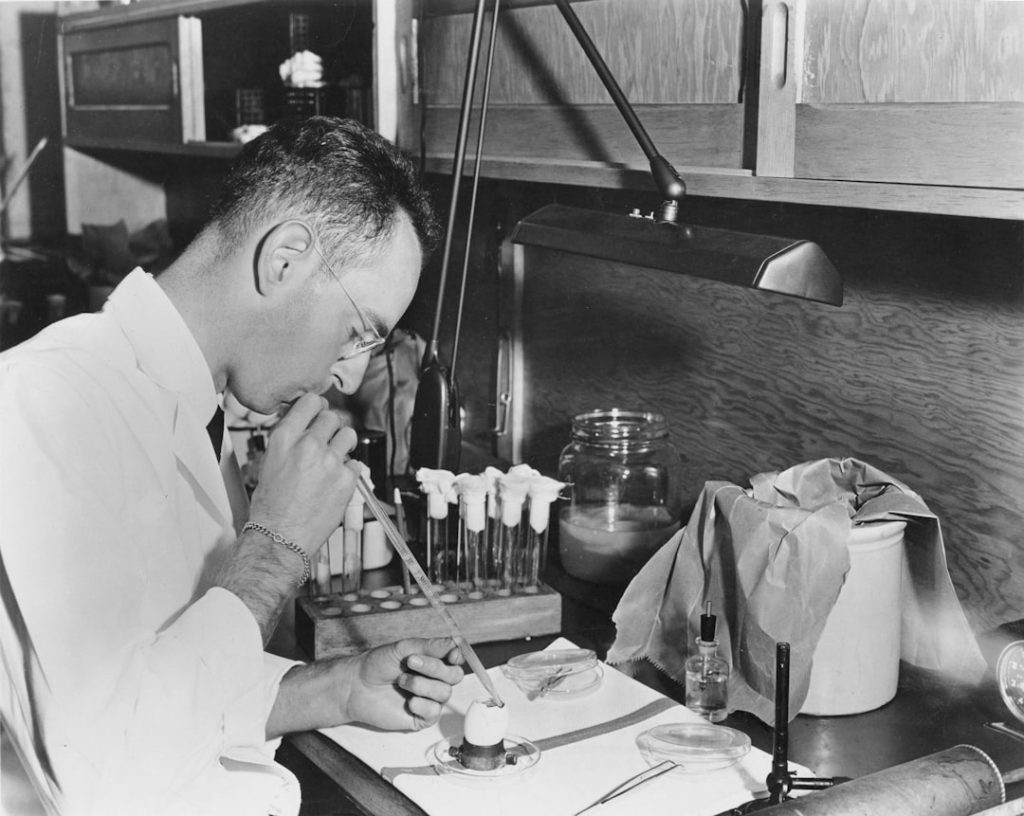
Oncolytic Viruses: Enlisting Viruses in the Fight
Oncolytic viruses are naturally occurring or genetically engineered viruses that selectively infect and replicate in cancer cells, ultimately leading to their destruction. These viruses often have the added benefit of stimulating an anti-tumor immune response. Clinical trials are exploring various oncolytic viruses for a range of cancers, including melanoma, glioblastoma, and breast cancer. The potential synergy between oncolytic viruses and other immunotherapies is also a subject of active research.
mRNA Vaccines for Cancer: Lessons from the Pandemic
The success of mRNA vaccines during the COVID-19 pandemic has accelerated research into their application in cancer treatment. These vaccines can be designed to present specific tumor antigens to the immune system, thereby training T-cells to recognize and attack cancer cells. Personalized mRNA vaccines, tailored to an individual’s unique tumor mutations, are also under investigation. This technology, still in its early stages for cancer, holds promise for both therapeutic and preventative applications. Imagine teaching your body’s immune system a mugshot of the enemy so it can identify and eliminate it.
Artificial Intelligence and Machine Learning in Oncology
AI and machine learning are increasingly being integrated into various aspects of oncology, from early detection and diagnosis to treatment planning and drug discovery. AI algorithms can analyze vast datasets, identify subtle patterns in medical images, and predict treatment responses with a level of precision that surpasses human capabilities in certain contexts. For example, AI-powered tools are being developed to optimize radiation therapy planning, stratify patients for clinical trials, and identify novel drug targets. This technological integration is akin to providing clinicians with a powerful, data-driven co-pilot.
Challenges and Considerations
| Metric | Value | Description |
|---|---|---|
| Number of IITs Registered | 350+ | Total investigator-initiated trials registered in the last 5 years |
| Average Enrollment per Trial | 120 Participants | Mean number of participants enrolled in each IIT |
| Completion Rate | 78% | Percentage of IITs completed as per protocol |
| Publication Rate | 65% | Percentage of IITs resulting in peer-reviewed publications |
| Common Therapeutic Areas | Cardiology, Oncology, Neurology | Most frequent medical fields studied in IITs |
| Average Duration | 18 Months | Typical length of an IIT from initiation to completion |
| Funding Sources | Academic Grants, Institutional Funds | Primary sources of financial support for IITs |
While these advancements represent significant progress, it is important to acknowledge the inherent challenges in cancer treatment and clinical research. The road to effective therapies is often long and fraught with complexities.
Overcoming Treatment Resistance
Cancer cells are adept at evolving and developing resistance to therapies, often through molecular alterations or by activating alternative survival pathways. This ongoing battle against resistance necessitates continuous research into combination therapies and sequential treatment strategies.
Managing Toxicity and Side Effects
Even targeted therapies and immunotherapies, while generally better tolerated than conventional chemotherapy, can cause significant side effects. Managing these toxicities and improving patient quality of life remain crucial aspects of clinical care and ongoing research.
Accessibility and Cost of Novel Therapies
The development of innovative cancer treatments often comes with a substantial cost. Ensuring equitable access to these life-saving therapies, particularly in resource-limited settings, is a critical societal challenge that needs to be addressed alongside scientific progress.
The Heterogeneity of Cancer
Cancer is not a single disease, but a collection of hundreds of distinct diseases, each with its own unique molecular signature and clinical behavior. This heterogeneity makes developing universal cures exceptionally difficult and underscores the need for personalized approaches. For instance, a drug that works well for one patient’s lung cancer may be ineffective for another patient’s lung cancer, if their underlying molecular drivers differ.
Conclusion
The ongoing clinical trials in oncology represent a collective global effort to incrementally dismantle the formidable challenge posed by cancer. While euphoria should be tempered with an appreciation for the complexities, the continuous stream of novel therapies, refined techniques, and deeper understanding of cancer biology offers tangible hope. Precision medicine, immunotherapy, advanced radiation techniques, and emerging approaches are not just scientific curiosities; they are the bedrock upon which future improvements in patient care will be built. As we move forward, the collaborative spirit of researchers, clinicians, and patients, all working within the rigorous framework of clinical trials, will continue to shape the trajectory of cancer treatment, transforming a once-grim prognosis into a more manageable and, in many cases, treatable condition.