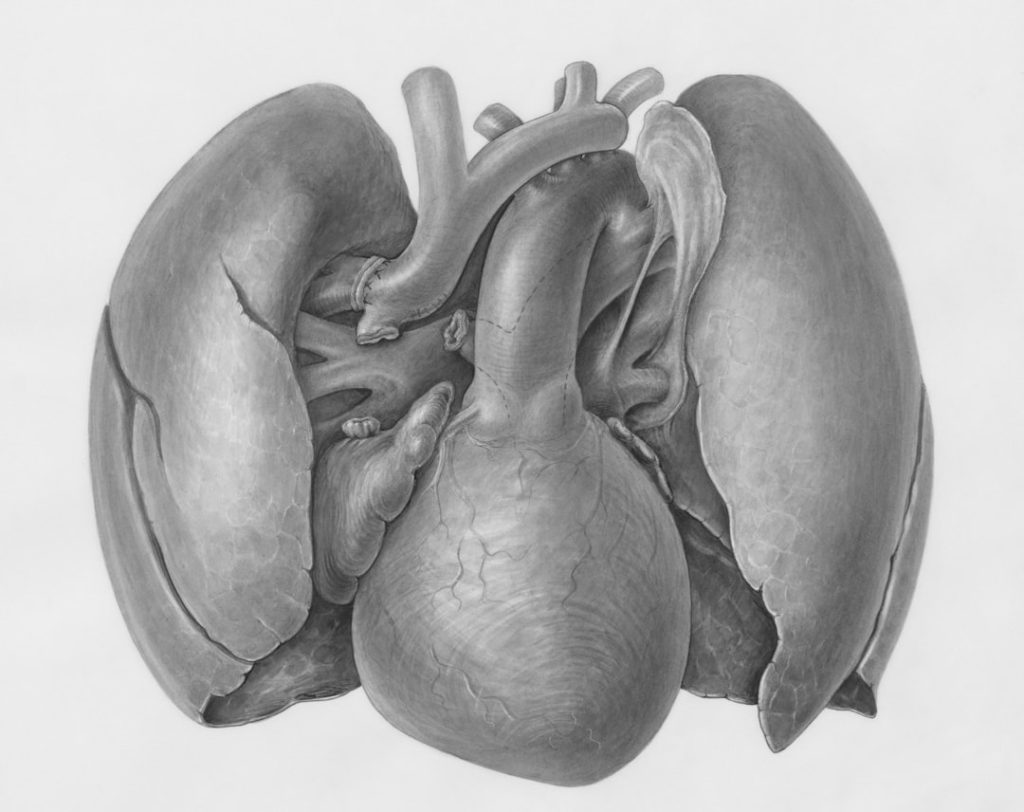
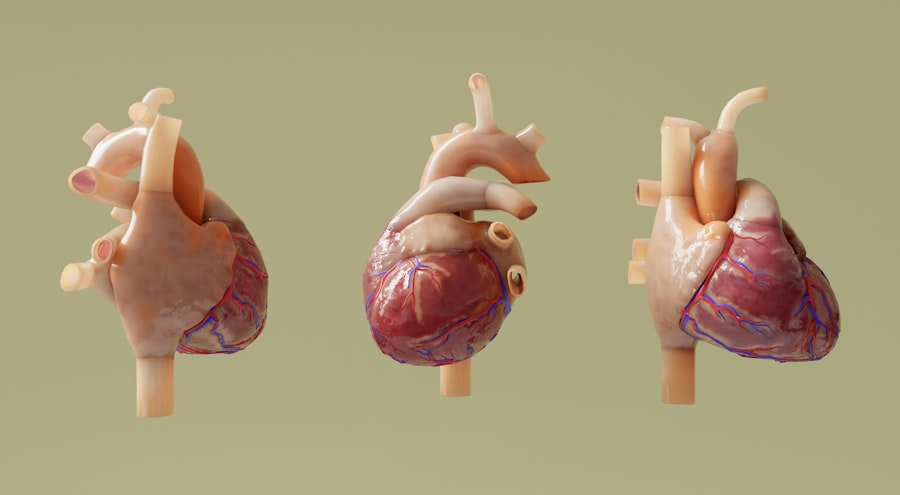
Heart failure (HF) is a complex clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s metabolic demands. This condition can arise from various underlying causes, including coronary artery disease, hypertension, and cardiomyopathy, leading to a spectrum of symptoms such as fatigue, dyspnea, and fluid retention. The prevalence of heart failure is alarmingly high, affecting millions of individuals worldwide, and it is a leading cause of morbidity and mortality.
The World Health Organization estimates that approximately 64 million people globally are living with heart failure, a number that is expected to rise as populations age and the burden of cardiovascular diseases increases. The pathophysiology of heart failure is multifaceted, involving neurohormonal activation, myocardial remodeling, and systemic inflammation. These processes contribute to the progressive decline in cardiac function and the eventual development of symptoms.
Heart failure can be classified into two main categories: heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). HFrEF is characterized by a significant reduction in the heart’s pumping ability, while HFpEF presents with preserved ejection fraction but impaired diastolic function. Understanding these distinctions is crucial for tailoring treatment strategies and improving patient outcomes.
Key Takeaways
- Heart failure clinical trials have evolved significantly, incorporating innovative therapies and patient-centered approaches.
- Current challenges include patient recruitment, diverse populations, and complex trial designs.
- Technological advancements enhance monitoring and data collection, improving trial accuracy and efficiency.
- Regulatory changes are shaping trial protocols and approval processes, impacting study timelines.
- Future research focuses on personalized treatments and integrating new technologies to optimize heart failure management.
Evolution of Heart Failure Clinical Trials
The landscape of clinical trials in heart failure has undergone significant transformation over the past few decades. Historically, early trials focused primarily on pharmacological interventions aimed at improving survival and reducing hospitalizations. Landmark studies such as the CONSENSUS trial in the late 1980s established the efficacy of angiotensin-converting enzyme (ACE) inhibitors in HFrEF, paving the way for subsequent research that would explore a broader array of therapeutic options.
As our understanding of heart failure has evolved, so too have the methodologies employed in clinical trials. In recent years, there has been a shift towards more comprehensive trial designs that incorporate diverse patient populations and real-world settings. This evolution reflects a growing recognition of the need for research that mirrors the complexities of clinical practice.
For instance, contemporary trials often include patients with comorbidities such as diabetes, chronic kidney disease, and obesity—conditions that are frequently encountered in heart failure populations but were historically underrepresented in clinical studies. Additionally, adaptive trial designs have gained traction, allowing for modifications based on interim results, which can expedite the development of effective therapies.
Current Challenges in Heart Failure Clinical Trials

Despite advancements in the design and execution of heart failure clinical trials, several challenges persist that can hinder the progress of research in this field. One significant issue is the heterogeneity of heart failure itself. Patients present with varying degrees of severity, different underlying etiologies, and a wide range of comorbid conditions.
This variability complicates the identification of appropriate endpoints and can lead to difficulties in generalizing findings across diverse populations. For example, a treatment that proves effective in a trial population with predominantly HFrEF patients may not yield similar results in those with HFpEF or mixed phenotypes. Another challenge lies in patient recruitment and retention.
Heart failure patients often experience significant physical limitations and may have multiple appointments with various healthcare providers, making participation in clinical trials logistically challenging. Moreover, the burden of managing chronic illness can lead to fatigue and reluctance to engage in additional healthcare activities. To address these issues, researchers are increasingly exploring strategies to enhance recruitment efforts, such as utilizing telehealth platforms for remote monitoring and follow-up visits, which can reduce the burden on patients while maintaining engagement in clinical research.
Innovative Therapies and Treatments
The field of heart failure has witnessed remarkable advancements in innovative therapies aimed at improving patient outcomes. One notable development is the emergence of novel pharmacological agents that target specific pathways involved in heart failure pathophysiology. For instance, sodium-glucose cotransporter-2 (SGLT2) inhibitors, originally developed for diabetes management, have shown significant benefits in heart failure patients by reducing hospitalizations and improving cardiovascular outcomes.
The DAPA-HF trial demonstrated that dapagliflozin reduced the risk of worsening heart failure or cardiovascular death in patients with HFrEF, leading to its approval for this indication. In addition to pharmacotherapy, device-based interventions have also evolved significantly. Cardiac resynchronization therapy (CRT) has become a cornerstone treatment for select patients with HFrEF who exhibit electrical dyssynchrony.
Recent advancements in device technology have led to improved outcomes through enhanced pacing algorithms and remote monitoring capabilities. Furthermore, left ventricular assist devices (LVADs) have emerged as a viable option for patients with advanced heart failure who are not candidates for heart transplantation. These devices provide mechanical support to the failing heart and have been shown to improve quality of life and survival rates.
Patient-Centered Approaches in Clinical Trials
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Duration (months) | Status |
|---|---|---|---|---|---|---|
| PARADIGM-HF | Phase 3 | 8442 | LCZ696 (Sacubitril/Valsartan) vs Enalapril | Composite of cardiovascular death or heart failure hospitalization | 27 | Completed |
| EMPEROR-Reduced | Phase 3 | 3730 | Empagliflozin vs Placebo | Time to cardiovascular death or heart failure hospitalization | 16 | Completed |
| SHIFT | Phase 3 | 6505 | Ivabradine vs Placebo | Composite of cardiovascular death or heart failure hospitalization | 23 | Completed |
| GALACTIC-HF | Phase 3 | 8258 | Omecamtiv Mecarbil vs Placebo | Composite of time to first heart failure event or cardiovascular death | 21 | Completed |
| VITALITY-HFpEF | Phase 2 | 257 | Vericiguat vs Placebo | Change in KCCQ physical limitation score | 24 | Completed |
The paradigm shift towards patient-centered approaches in clinical trials has gained momentum in recent years, emphasizing the importance of incorporating patient perspectives into research design and implementation. This approach recognizes that patients are not merely subjects but active participants whose experiences and preferences should inform trial methodologies. Engaging patients in the development of trial protocols can lead to more relevant endpoints that reflect what matters most to them, such as symptom relief and functional improvement.
Moreover, patient-centered approaches extend beyond trial design to encompass recruitment strategies and informed consent processes. Researchers are increasingly utilizing qualitative methods to understand patient motivations and barriers to participation. By addressing these factors, clinical trials can become more accessible and appealing to potential participants.
For instance, providing educational resources that clarify the purpose and potential benefits of participation can help demystify the process and encourage enrollment among diverse populations.
Technological Advancements in Monitoring and Data Collection
Technological innovations have revolutionized the way researchers monitor patients and collect data in heart failure clinical trials. Wearable devices, mobile health applications, and remote monitoring systems have emerged as powerful tools for capturing real-time data on patient health status and treatment adherence. These technologies enable continuous monitoring of vital signs such as heart rate, blood pressure, and weight—parameters critical for managing heart failure.
The integration of telehealth solutions has also facilitated more frequent interactions between patients and healthcare providers, allowing for timely interventions when necessary. For example, remote monitoring systems can alert clinicians to early signs of worsening heart failure, enabling proactive management strategies that may prevent hospitalizations. Additionally, data collected through these technologies can enhance trial outcomes by providing a more comprehensive understanding of treatment effects in real-world settings.
Regulatory Changes and Impact on Clinical Trials
Regulatory agencies play a crucial role in shaping the landscape of clinical trials for heart failure therapies. Recent changes in regulatory frameworks have aimed to streamline the approval process for innovative treatments while ensuring patient safety remains paramount. The U.S. Food and Drug Administration (FDA) has introduced initiatives such as the Breakthrough Therapy designation, which expedites the development and review of drugs that demonstrate substantial improvement over existing therapies for serious conditions. These regulatory changes have significant implications for heart failure clinical trials. For instance, sponsors may now have greater flexibility in trial design, allowing for smaller sample sizes or shorter study durations when appropriate evidence supports such modifications. This adaptability can accelerate the availability of new therapies to patients who desperately need them. However, it also necessitates rigorous post-marketing surveillance to monitor long-term safety and efficacy once these therapies are introduced into broader clinical practice.
Future Directions in Heart Failure Clinical Research
Looking ahead, the future of heart failure clinical research is poised for exciting developments driven by ongoing advancements in science and technology. One promising area is the exploration of personalized medicine approaches tailored to individual patient characteristics. Genetic profiling and biomarker discovery hold potential for identifying patients who are most likely to benefit from specific therapies, thereby optimizing treatment strategies.
Furthermore, there is an increasing emphasis on integrating social determinants of health into clinical research frameworks. Understanding how factors such as socioeconomic status, access to care, and cultural influences impact heart failure outcomes can inform more equitable approaches to treatment and research participation. By addressing these broader determinants, researchers can work towards reducing disparities in heart failure care.
As we move forward into an era characterized by rapid technological advancements and evolving healthcare paradigms, collaboration among stakeholders—including researchers, clinicians, patients, and regulatory bodies—will be essential for advancing heart failure research. By fostering an environment conducive to innovation while prioritizing patient-centered care, we can aspire to improve outcomes for individuals living with this challenging condition.