Medical research has continuously pushed the boundaries of human understanding, leading to a myriad of progressive breakthroughs that redefine disease treatment and prevention. This article explores some of the most impactful advancements, tracing their development and examining their current and potential implications for global health. We will delve into areas ranging from molecular biology to digital health, highlighting the ongoing evolution of medical science.
The ability to directly manipulate and understand the human genome has opened entirely new avenues for therapeutic intervention. This field, once a theoretical concept, is now a practical reality offering unprecedented precision in addressing disease at its root.
CRISPR-Cas9 Gene Editing: Precision and Potential
CRISPR-Cas9, an acronym for Clustered Regularly Interspaced Short Palindromic Repeats and CRISPR-associated protein 9, has revolutionized gene editing. This technology acts as a molecular “cut and paste” tool, allowing scientists to precisely target and modify specific DNA sequences. Its origins lie in bacterial immune systems, where it defends against viral invaders by cutting their genetic material.
- Mechanism of Action: When a guide RNA molecule, designed to match a target DNA sequence, binds to the Cas9 enzyme, the complex is directed to the specific DNA locus. Cas9 then cleaves both strands of the DNA, creating a double-strand break. The cell’s natural repair mechanisms then attempt to fix this break, which can be exploited to either disrupt a gene, insert new genetic material, or correct a mutation. This precision contrasts sharply with earlier gene editing techniques, which were far less specific and more prone to off-target effects.
- Therapeutic Applications: CRISPR-Cas9 is being investigated for a wide range of genetic disorders. Early clinical trials have shown promise in treating conditions such as sickle cell disease and beta-thalassemia by correcting the underlying genetic mutations in hematopoietic stem cells. Researchers are also exploring its use in muscular dystrophy, cystic fibrosis, and various cancers. The ability to edit germline cells, though controversial, represents a future frontier for preventing inherited diseases entirely.
- Ethical Considerations: The power of gene editing raises significant ethical questions. Concerns revolve around the potential for unintended off-target edits, the long-term safety of germline editing, and the societal implications of “designer babies.” International guidelines and robust public discourse are essential for navigating these complex ethical landscapes as the technology progresses.
Advanced Gene Sequencing: Unveiling the Blueprint
Beyond editing, the ability to rapidly and affordably sequence entire genomes has transformed diagnostics and personalized medicine. What once took years and billions of dollars can now be achieved in days for a fraction of the cost.
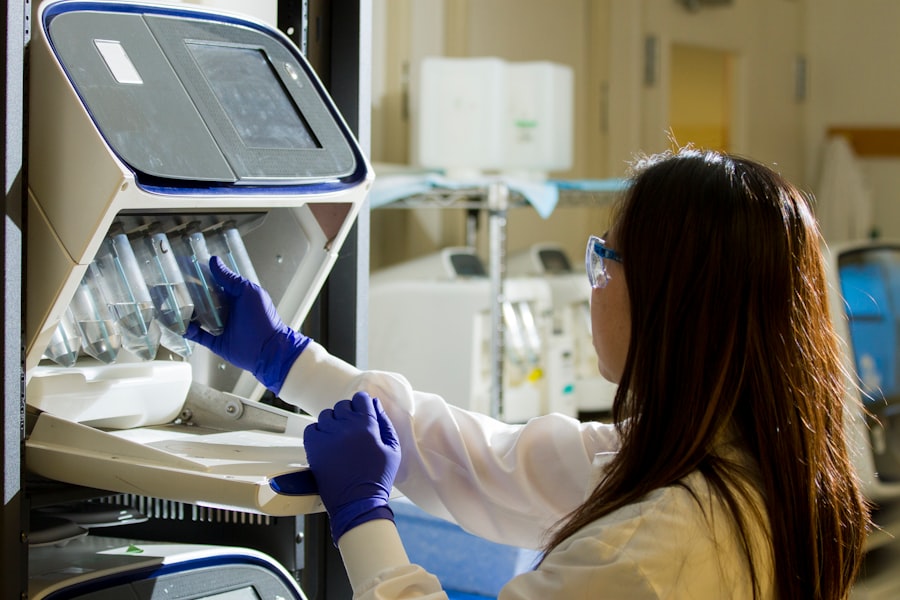
- Next-Generation Sequencing (NGS): NGS technologies allow for the parallel sequencing of millions of DNA fragments, dramatically increasing throughput and reducing sequencing costs. This has made whole-genome sequencing (WGS) and whole-exome sequencing (WES) accessible for research and clinical applications. NGS platforms employ various proprietary methods, but generally involve fragmenting DNA, attaching adapters, amplifying the fragments, and then sequencing them simultaneously.
- Diagnostic Power: Genomic sequencing is becoming a cornerstone of rare disease diagnosis, identifying causative mutations that would otherwise remain elusive. It also informs cancer treatment by characterizing tumor genomes, identifying actionable mutations, and predicting response to targeted therapies. For infectious diseases, pathogen sequencing aids in outbreak tracking and antibiotic resistance monitoring.
- Pharmacogenomics: Understanding an individual’s genetic makeup can predict their response to specific medications. Pharmacogenomics aims to optimize drug selection and dosage, minimizing adverse drug reactions and maximizing therapeutic efficacy. For example, genetic variations in drug-metabolizing enzymes can significantly alter how a patient processes certain chemotherapy agents or antidepressants. This represents a significant step towards truly personalized medicine, moving beyond a one-size-fits-all approach.
The Emergence of Advanced Immunotherapies
The immune system, a sophisticated defense mechanism, is now being intentionally leveraged and augmented to combat diseases, particularly cancer, with remarkable success. This represents a paradigm shift from traditional chemotherapy and radiation.
Chimeric Antigen Receptor (CAR) T-cell Therapy: Reprogramming Immunity
CAR T-cell therapy is a highly specialized cancer treatment that involves genetically engineering a patient’s own T cells to recognize and attack cancer cells. These modified T cells act as a living drug, continuously patrolling and eradicating malignant cells.
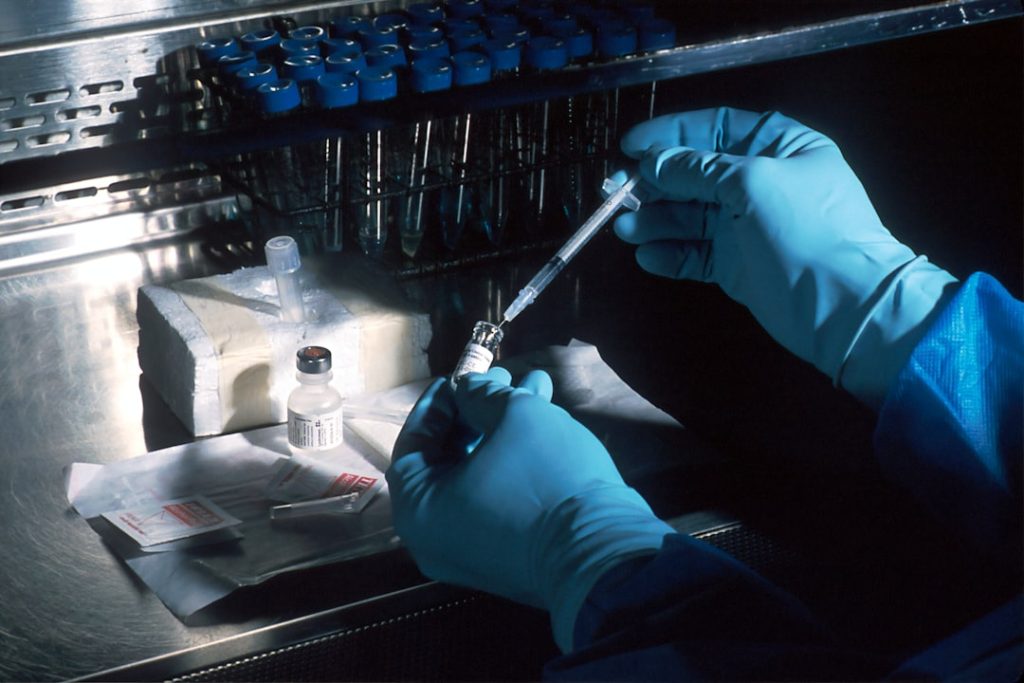
- Process and Design: The process begins with drawing blood from the patient to collect T cells. These T cells are then sent to a laboratory where they are genetically engineered with a chimeric antigen receptor (CAR). The CAR is a synthetic receptor designed to bind to a specific protein (antigen) found on the surface of cancer cells. Once engineered, the CAR T cells are expanded in large quantities and infused back into the patient. The CAR on the T cell acts as a “smart weapon,” directly guiding the T cell to the tumor.
- Clinical Successes: CAR T-cell therapy has achieved significant remission rates in certain blood cancers, particularly B-cell acute lymphoblastic leukemia (ALL) and large B-cell lymphoma, in patients who have exhausted other treatment options. These treatments have moved from experimental to FDA-approved therapies, offering a lifeline to patients with aggressive and refractory malignancies.
- Challenges and Future Directions: While effective, CAR T-cell therapy can cause severe side effects such as cytokine release syndrome (CRS) and neurotoxicity, requiring careful management. Research is ongoing to improve the safety profile, expand its applicability to solid tumors (a more challenging endeavor due to the heterogeneous nature of solid tumors and the immunosuppressive tumor microenvironment), and develop off-the-shelf CAR T-cell therapies using allogeneic (donor) cells.
Immune Checkpoint Inhibitors: Unleashing the Body’s Defenses
Immune checkpoint inhibitors are a class of drugs that block proteins (checkpoints) that normally prevent the immune system from attacking healthy cells. By “releasing the brakes” on the immune response, these drugs allow a patient’s own T cells to recognize and destroy cancer cells.
- Mechanism of Action: Cancer cells often exploit immune checkpoints, such as PD-1 (Programmed Death-1) and CTLA-4 (Cytotoxic T-Lymphocyte Antigen 4), to evade detection and destruction by the immune system. Checkpoint inhibitor drugs, typically monoclonal antibodies, block these interactions. For instance, anti-PD-1 antibodies prevent the PD-1 receptor on T cells from binding to its ligand (PD-L1) on cancer cells, thereby re-activating the T cells’ anti-tumor activity.
- Broad Impact: These therapies have transformed the treatment landscape for numerous cancers, including melanoma, lung cancer, kidney cancer, and Hodgkin lymphoma, often leading to durable responses where traditional treatments failed. They have fundamentally altered prognosis for many patients with advanced disease.
- Combination Therapies and Biomarkers: Current research focuses on combining checkpoint inhibitors with other immunotherapies, chemotherapy, or radiation to enhance efficacy. Identifying biomarkers that predict response to these therapies is crucial to stratify patients and guide treatment decisions, maximizing benefit and minimizing unnecessary exposure to side effects.
The Digital Transformation of Healthcare

The integration of advanced computing, artificial intelligence, and sophisticated data analysis into medical practice is creating a paradigm shift in how we diagnose, treat, and monitor patients. This digital revolution extends beyond the clinic, empowering individuals to take a more active role in their health management.
Artificial Intelligence (AI) and Machine Learning (ML) in Diagnostics
AI and ML algorithms are increasingly being applied to medical imaging, pathology, and patient data analysis, offering tools to enhance diagnostic accuracy and efficiency.
- Image Analysis: AI algorithms can analyze medical images (X-rays, CT scans, MRIs, pathology slides) with remarkable speed and precision, often detecting subtle abnormalities that might be missed by the human eye. For example, AI can assist in the early detection of diabetic retinopathy from retinal scans, identify suspicious lesions in mammograms, and characterize tumors in CT scans. This acts as a powerful “second pair of eyes” for clinicians, improving sensitivity and specificity.
- Predictive Analytics: ML models can analyze vast datasets of patient information (electronic health records, genomic data, lifestyle factors) to predict disease risk, prognosis, and treatment response. This capability moves us closer to proactive healthcare, identifying individuals at high risk for certain conditions before symptoms manifest. For instance, algorithms can predict sepsis onset in critical care settings or identify patients at risk of readmission.
- Drug Discovery and Development: AI is significantly accelerating drug discovery by sifting through vast chemical libraries to identify potential drug candidates, predicting their properties, and optimizing molecular structures. This drastically reduces the time and cost associated with traditional drug development pipelines, acting as a “smart sieve” for potential therapeutic molecules.
Telemedicine and Remote Patient Monitoring: Expanding Access
The COVID-19 pandemic significantly accelerated the adoption of telemedicine and remote patient monitoring, demonstrating their critical role in delivering healthcare beyond traditional clinic walls.
- Virtual Consultations: Telemedicine platforms enable patients to connect with healthcare providers remotely via video, audio, or text. This improves access to care, particularly for individuals in rural areas, those with mobility issues, or during public health crises. It reduces travel time and costs for patients, and optimizes provider schedules.
- Wearable Devices and Sensors: Wearable devices and biosensors continuously collect physiological data (heart rate, blood pressure, glucose levels, activity levels) from patients in their natural environment. This data can be transmitted to healthcare providers, allowing for proactive intervention and real-time monitoring of chronic conditions. For example, continuous glucose monitors have transformed diabetes management, and smartwatches can detect atrial fibrillation. This continuous data stream offers a more holistic view of a patient’s health, rather than snapshots from periodic clinic visits.
- Personalized Health Management: The confluence of telemedicine and remote monitoring empowers individuals to manage their own health more effectively. Patients can track their progress, receive personalized feedback, and communicate easily with their care team, fostering greater adherence to treatment plans and promoting healthier lifestyles.
Nanomedicine and Targeted Drug Delivery
The ability to engineer materials at the nanoscale (one billionth of a meter) is opening new frontiers in diagnostics and therapeutics, offering unprecedented precision in drug delivery and disease detection.
Nanoparticles for Precision Therapeutics
Nanoparticles, typically 1 to 100 nanometers in size, can be engineered to carry drugs directly to target cells or tissues, minimizing systemic side effects and increasing therapeutic efficacy.
- Drug Encapsulation: Nanoparticles can encapsulate drugs, protecting them from degradation in the bloodstream and releasing them specifically at the disease site. For example, liposomes (lipid-based nanoparticles) are used to deliver chemotherapy drugs directly to tumors, thereby concentrating the therapeutic agent where it is needed most and sparing healthy tissues. This is akin to a “stealth delivery truck” that only unloads its cargo at specific coordinates.
- Targeted Delivery Mechanisms: Nanoparticles can be functionalized with specific ligands or antibodies that recognize receptors overexpressed on cancer cells or inflammatory sites. This active targeting mechanism ensures that the drug preferentially accumulates in the diseased tissue, further enhancing efficacy and reducing toxicity.
- Vaccine Development: Nanoparticles have proven instrumental in vaccine development, particularly mRNA vaccines. Lipid nanoparticles (LNPs) encapsulate fragile mRNA molecules, protecting them from degradation and facilitating their delivery into cells to stimulate an immune response. This innovative delivery system was critical to the rapid development of COVID-19 vaccines.
Nanosensors for Early Disease Detection
Miniaturized sensors capable of detecting biomarkers at very low concentrations hold promise for earlier and more accurate disease diagnosis.
- High Sensitivity and Specificity: Nanosensors exploit the unique physicochemical properties of nanomaterials to detect specific molecules (proteins, DNA, metabolites) with extreme sensitivity and specificity. This allows for the detection of disease markers before symptoms become apparent, offering a window for earlier intervention. For example, nanoscale biosensors are being developed to detect early cancer biomarkers in blood or urine, or to identify viral particles from a breath sample.
- Point-of-Care Diagnostics: The small size and potential for cost-effective manufacturing make nanosensors ideal for point-of-care diagnostic devices. These devices could enable rapid and accurate testing outside of traditional laboratory settings, particularly in resource-limited environments. Imagine a handheld device that can diagnose a communicable disease within minutes from a small biological sample.
- Continuous Monitoring: Some nanosensor technologies are being developed for continuous in-vivo monitoring, allowing for real-time tracking of physiological parameters or disease progression. This could provide invaluable data for personalized treatment adjustments and improved patient outcomes.
Regenerative Medicine and Tissue Engineering
| Year | Research Area | Key Metric | Progress Indicator | Notes |
|---|---|---|---|---|
| 2020 | Gene Therapy | Number of Clinical Trials | 150 | Increased focus on rare genetic disorders |
| 2021 | Immunotherapy | FDA Approvals | 12 | New cancer treatments approved |
| 2022 | CRISPR Technology | Published Research Papers | 320 | Significant advancements in gene editing |
| 2023 | Personalized Medicine | Patient Enrollment in Trials | 5,000 | Growing adoption of tailored treatments |
| 2024 | AI in Diagnostics | Accuracy Improvement (%) | 18% | Enhanced diagnostic precision using AI |
The ability to repair, replace, or regenerate damaged tissues and organs represents a transformative frontier in medicine, offering solutions for conditions previously deemed incurable.
Stem Cell Therapies: Repairing and Rebuilding
Stem cells, with their unique ability to differentiate into various cell types, are at the forefront of regenerative medicine. They act as the body’s internal repair system.
- Types of Stem Cells: Research focuses on various types, including embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), and adult stem cells (e.g., hematopoietic stem cells, mesenchymal stem cells). iPSCs, generated from adult somatic cells, have significant potential as they can be patient-specific, circumventing ethical concerns associated with ESCs and reducing immunological rejection.
- Current Applications: Hematopoietic stem cell transplantation (HSCT) has been a standard treatment for blood cancers and certain genetic disorders for decades. However, the field is expanding. Clinical trials are exploring stem cell therapies for conditions such as spinal cord injuries, Parkinson’s disease, heart failure, and macular degeneration, aiming to replace damaged cells or stimulate tissue repair. For example, iPSC-derived retinal cells are being tested to restore vision in patients with age-related macular degeneration.
- Challenges and Future Outlook: Challenges include ensuring the safety and efficacy of transplanted cells, controlling their differentiation pathways, and preventing tumor formation. Standardization of protocols and rigorous clinical trials are crucial for bringing these therapies to widespread clinical use. The future envisions “off-the-shelf” stem cell therapies and engineered tissues derived from stem cells.
Organoids and Bioprinting: Creating Tissues in Vitro
Organoids and 3D bioprinting represent advanced approaches to creating functional tissues and organs, both for research and potential transplantation.
- Organoids as Disease Models: Organoids are three-dimensional, self-organizing tissue cultures derived from stem cells that mimic the structure and function of actual organs. They provide invaluable tools for studying disease mechanisms, testing new drugs, and understanding organ development without directly experimenting on living subjects. Researchers have grown “mini-brains,” “mini-guts,” and “mini-kidneys,” offering unprecedented insight into human biology.
- 3D Bioprinting for Tissue Engineering: 3D bioprinting uses biomaterials and living cells (bio-inks) to create complex tissue structures layer by layer. This technology holds promise for generating patient-specific tissues for transplantation (e.g., skin grafts, cartilage) and for building functional organ models for drug testing. The vision is to print entire functional organs for transplantation, addressing the critical shortage of donor organs. This is analogous to a sophisticated biological inkjet printer.
- Path to Functional Organs: While early successes in printing simple tissues are evident, creating fully functional, vascularized (with blood vessels) and innervated (with nerves) organs remains a formidable challenge. Overcoming issues of vascularization and integration with the host body are ongoing research priorities.
In conclusion, the trajectory of medical research is characterized by an accelerating pace of discovery and translation. From the precision of gene editing that acts as a molecular surgeon, to immunotherapies that unleash the body’s own defenses, to digital tools that augment human capabilities in diagnosis, and regenerative approaches that aim to rebuild, these progressive breakthroughs collectively paint a picture of a future where disease is managed with greater effectiveness, personalized care becomes the norm, and health outcomes are dramatically improved. Navigating the ethical implications and ensuring equitable access to these advancements will be critical as we move forward.