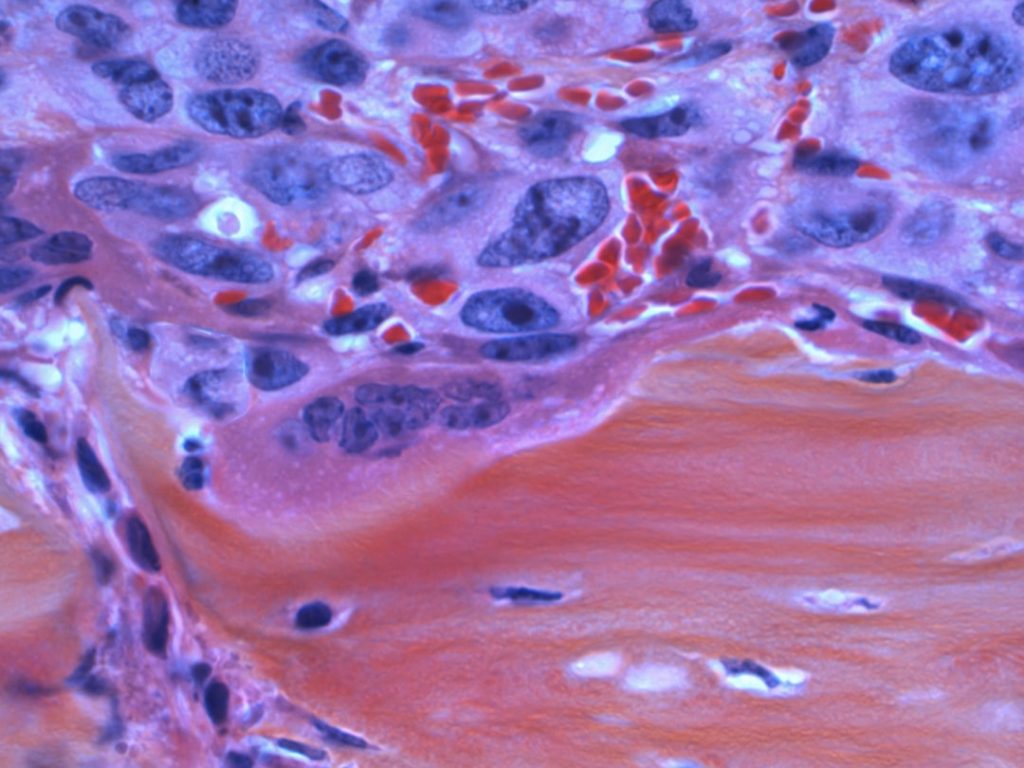
Melanoma, a malignant form of skin cancer, arises from melanocytes, the pigment-producing cells in the skin. It is known for its aggressive nature and potential to metastasize to other parts of the body, making early detection and treatment crucial. The incidence of melanoma has been rising globally, with factors such as increased sun exposure and the use of tanning beds contributing to this trend.
Clinical trials play a pivotal role in advancing our understanding of melanoma and developing new treatment modalities. These trials are essential for evaluating the safety and efficacy of novel therapies, providing hope for patients who may have limited options. Clinical trials in melanoma encompass a wide range of research efforts, from early-phase studies assessing new drugs to large-scale trials comparing existing treatments.
They are designed to answer specific scientific questions and often involve rigorous protocols to ensure patient safety and data integrity. The results from these trials can lead to significant changes in clinical practice, influencing treatment guidelines and improving patient outcomes. As researchers continue to explore innovative approaches to combat melanoma, the importance of clinical trials cannot be overstated; they are the backbone of evidence-based medicine in oncology.
Key Takeaways
- Clinical trials are essential for developing new melanoma treatments and improving patient outcomes.
- Targeted therapies and immunotherapies have revolutionized melanoma treatment options.
- Combination therapies show promise in enhancing treatment efficacy for melanoma patients.
- Precision medicine and emerging biomarkers enable more personalized and effective melanoma treatments.
- Patient participation is crucial for advancing melanoma research and discovering innovative therapies.
New Treatment Options in Melanoma: Clinical Trials
The landscape of melanoma treatment has evolved dramatically over the past decade, largely due to the insights gained from clinical trials. Traditional therapies such as surgery and chemotherapy have been supplemented by newer modalities that target the underlying mechanisms of cancer growth. For instance, the advent of immune checkpoint inhibitors has revolutionized the treatment paradigm for advanced melanoma.
Drugs like pembrolizumab and nivolumab have shown remarkable efficacy in clinical trials, leading to durable responses in a subset of patients who previously had limited options. In addition to immune checkpoint inhibitors, clinical trials are exploring other innovative treatment options, including oncolytic virus therapy and personalized vaccines. Oncolytic viruses are engineered to selectively infect and kill cancer cells while sparing normal tissues.
Trials investigating these therapies have demonstrated promising results, with some patients experiencing significant tumor regression. Personalized vaccines, which aim to stimulate the immune system against specific tumor antigens, are also being evaluated in clinical settings. These new treatment options represent a shift towards more targeted and individualized approaches in melanoma management, highlighting the dynamic nature of ongoing research.
Targeted Therapies and Immunotherapies for Melanoma
Targeted therapies and immunotherapies have emerged as two cornerstone strategies in the management of melanoma, particularly for patients with advanced disease. Targeted therapies focus on specific genetic mutations that drive tumor growth. For example, BRAF inhibitors such as vemurafenib and dabrafenib have been developed for patients with BRAF V600E mutations, which are present in approximately 40-60% of melanoma cases.
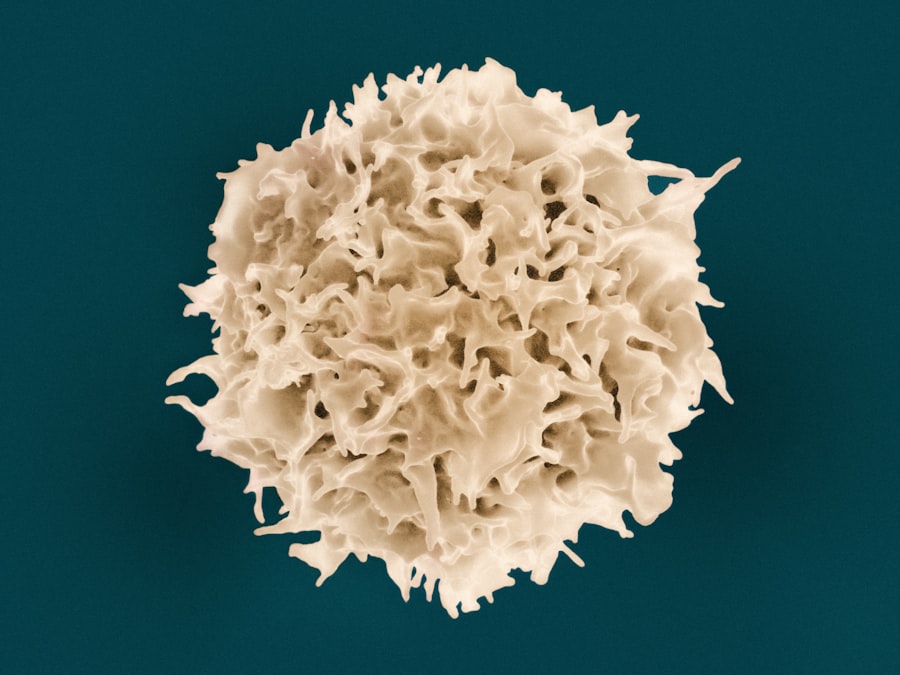
Clinical trials have demonstrated that these agents can lead to significant tumor shrinkage and improved survival rates compared to traditional chemotherapy. On the other hand, immunotherapies harness the body’s immune system to fight cancer. Immune checkpoint inhibitors, which block proteins that inhibit immune responses, have shown remarkable success in clinical trials.
Nivolumab and ipilimumab, when used in combination, have resulted in higher response rates than either drug alone. The CheckMate 067 trial is a landmark study that highlighted the benefits of this combination therapy, showing improved overall survival compared to monotherapy. The dual approach not only enhances the immune response against melanoma but also provides a framework for exploring further combinations with other therapeutic agents.
Advancements in Combination Therapies for Melanoma
Combination therapies represent a promising frontier in melanoma treatment, aiming to enhance therapeutic efficacy while minimizing resistance. The rationale behind combining different modalities—such as targeted therapies with immunotherapies—stems from the understanding that melanoma can employ various mechanisms to evade treatment. By attacking the cancer from multiple angles, researchers hope to overcome resistance and achieve more durable responses.
Recent clinical trials have explored various combinations, including those involving targeted agents like BRAF inhibitors alongside immune checkpoint inhibitors. For instance, studies have shown that combining dabrafenib with trametinib (a MEK inhibitor) can lead to improved outcomes in patients with BRAF-mutant melanoma. Furthermore, ongoing trials are investigating combinations of immunotherapies with other agents such as oncolytic viruses or novel small molecules that modulate the tumor microenvironment.
These advancements underscore a shift towards more integrative treatment strategies that leverage the strengths of different therapeutic approaches.
The Role of Precision Medicine in Melanoma Clinical Trials
| Trial Phase | Number of Trials | Primary Endpoint | Common Treatments Tested | Average Enrollment | Trial Duration (Months) |
|---|---|---|---|---|---|
| Phase 1 | 45 | Safety and Dosage | Immunotherapy, Targeted Therapy | 30 | 12 |
| Phase 2 | 60 | Efficacy and Side Effects | Checkpoint Inhibitors, Combination Therapies | 100 | 18 |
| Phase 3 | 35 | Effectiveness and Monitoring | Immunotherapy, Targeted Therapy, Chemotherapy | 300 | 24 |
| Phase 4 | 10 | Post-Marketing Surveillance | Approved Melanoma Treatments | 500 | 36 |
Precision medicine has become a cornerstone of modern oncology, particularly in the context of melanoma clinical trials. This approach tailors treatment based on individual patient characteristics, including genetic makeup and tumor biology. In melanoma, understanding specific mutations and molecular profiles can guide therapeutic decisions and improve outcomes.
For example, patients with identified BRAF mutations are directed towards targeted therapies that specifically inhibit this pathway. Clinical trials are increasingly incorporating precision medicine principles by utilizing genomic profiling to stratify patients based on their tumor characteristics. This allows for more personalized treatment plans that align with the unique biology of each patient’s cancer.
Additionally, ongoing research is focused on identifying new biomarkers that can predict response to specific therapies, further enhancing the precision medicine approach in melanoma management. As these strategies evolve, they hold the potential to transform how clinicians approach treatment decisions and improve overall patient care.
Emerging Biomarkers and Predictive Testing in Melanoma Trials

The identification of emerging biomarkers is critical for advancing melanoma research and improving patient outcomes. Biomarkers can provide insights into tumor behavior, predict treatment response, and inform prognosis. In recent years, several biomarkers have gained attention in clinical trials for melanoma, including PD-L1 expression levels and tumor mutational burden (TMB).
PD-L1 is a protein that can indicate how likely a tumor is to respond to immune checkpoint inhibitors; higher levels often correlate with better responses to these therapies. Tumor mutational burden is another promising biomarker that reflects the number of mutations within a tumor’s DNStudies have suggested that a higher TMB may be associated with improved responses to immunotherapy due to an increased likelihood of neoantigen formation, which can elicit a stronger immune response. Clinical trials are actively exploring these biomarkers to refine patient selection for specific treatments and enhance therapeutic outcomes.
As research continues to uncover new biomarkers and refine predictive testing methods, the potential for personalized treatment strategies in melanoma becomes increasingly tangible.
Challenges and Future Directions in Melanoma Clinical Trials
Despite significant advancements in melanoma research through clinical trials, several challenges remain that must be addressed to optimize patient outcomes further. One major challenge is the heterogeneity of melanoma itself; tumors can vary widely in their genetic makeup and response to treatment. This variability complicates trial design and necessitates larger sample sizes to ensure robust conclusions can be drawn across diverse patient populations.
Additionally, patient recruitment and retention pose ongoing challenges in clinical trials. Many eligible patients may be unaware of available trials or may hesitate to participate due to concerns about potential side effects or the experimental nature of treatments. Efforts to improve awareness and education about clinical trials are essential for enhancing participation rates.
Future directions in melanoma clinical trials will likely focus on integrating real-world evidence with traditional trial data, utilizing digital health technologies for remote monitoring, and exploring novel endpoints that reflect patient-reported outcomes.
The Importance of Patient Participation in Melanoma Clinical Trials
Patient participation is fundamental to the success of clinical trials in melanoma research. Without willing participants, it would be impossible to gather the necessary data to evaluate new treatments effectively or understand their impact on various populations. Engaging patients not only accelerates the pace of research but also ensures that diverse perspectives are considered in trial design and implementation.
Moreover, patient involvement can lead to more relevant research questions being addressed, as patients often have unique insights into their experiences with disease and treatment options. Advocacy groups play a crucial role in facilitating communication between researchers and patients, helping to bridge gaps in understanding and fostering a collaborative environment for research advancement. As clinical trials continue to evolve, prioritizing patient engagement will be essential for driving innovation and improving outcomes in melanoma care.