Oncology clinical research is a vital field that focuses on the study of cancer, its causes, and the development of effective treatments. This area of research encompasses a wide range of activities, including laboratory studies, clinical trials, and epidemiological investigations. The primary goal is to improve patient outcomes by advancing our understanding of cancer biology and developing innovative therapeutic strategies.
As cancer remains one of the leading causes of morbidity and mortality worldwide, the importance of oncology clinical research cannot be overstated. It serves as the backbone for translating scientific discoveries into clinical practice, ultimately aiming to enhance survival rates and quality of life for patients. The landscape of oncology clinical research has evolved significantly over the past few decades.
Historically, cancer treatment was largely based on empirical approaches, with limited understanding of the underlying mechanisms driving tumor growth and metastasis. However, with the advent of molecular biology and advancements in technology, researchers have gained unprecedented insights into the genetic and environmental factors contributing to cancer. This evolution has paved the way for more targeted and effective treatment modalities, shifting the paradigm from a one-size-fits-all approach to more personalized strategies that consider individual patient characteristics.
Key Takeaways
- Oncology clinical research has evolved to include diverse treatment modalities improving patient outcomes.
- Precision medicine enables personalized cancer treatments based on individual genetic profiles.
- Immunotherapy has revolutionized cancer care by harnessing the immune system to target tumors.
- Advances in early detection and screening enhance the chances of successful cancer treatment.
- Ongoing clinical trials and genomic research are critical for developing future oncology therapies.
Evolution of Treatment Modalities in Oncology
The evolution of treatment modalities in oncology has been marked by significant milestones that reflect the growing understanding of cancer biology. In the early 20th century, surgery was the primary treatment option for cancer patients, often accompanied by radiation therapy. These approaches were limited by their inability to address systemic disease or target specific tumor characteristics.
As research progressed, chemotherapy emerged as a revolutionary treatment modality in the mid-20th century, introducing cytotoxic agents that could target rapidly dividing cancer cells. While chemotherapy improved survival rates for many patients, it also came with a host of side effects due to its lack of specificity. In recent years, the development of targeted therapies has transformed the treatment landscape further.
These therapies are designed to interfere with specific molecular targets associated with cancer, such as mutated genes or overexpressed proteins. For instance, the introduction of trastuzumab (Herceptin) for HER2-positive breast cancer exemplifies how targeted therapies can significantly improve patient outcomes while minimizing adverse effects. The evolution from traditional chemotherapy to targeted therapies illustrates a broader trend in oncology toward more sophisticated and nuanced treatment options that are tailored to individual patient profiles.
Precision Medicine and Personalized Treatment Approaches
Precision medicine represents a paradigm shift in oncology that emphasizes the customization of healthcare, with medical decisions tailored to the individual patient based on their genetic makeup, lifestyle, and environment. This approach is grounded in the understanding that cancer is not a single disease but rather a collection of heterogeneous disorders that can vary significantly from one patient to another. By leveraging genomic information, clinicians can identify specific mutations or alterations within a patient’s tumor that may be driving its growth and progression.
One notable example of precision medicine in oncology is the use of next-generation sequencing (NGS) technologies to analyze tumor DNNGS allows for comprehensive profiling of genetic alterations in tumors, enabling oncologists to select targeted therapies that are most likely to be effective for a particular patient. For instance, patients with non-small cell lung cancer (NSCLC) harboring mutations in the EGFR gene may benefit from EGFR inhibitors like osimertinib. This personalized approach not only enhances treatment efficacy but also reduces unnecessary exposure to ineffective therapies, thereby improving overall patient care.
Immunotherapy and its Impact on Cancer Treatment
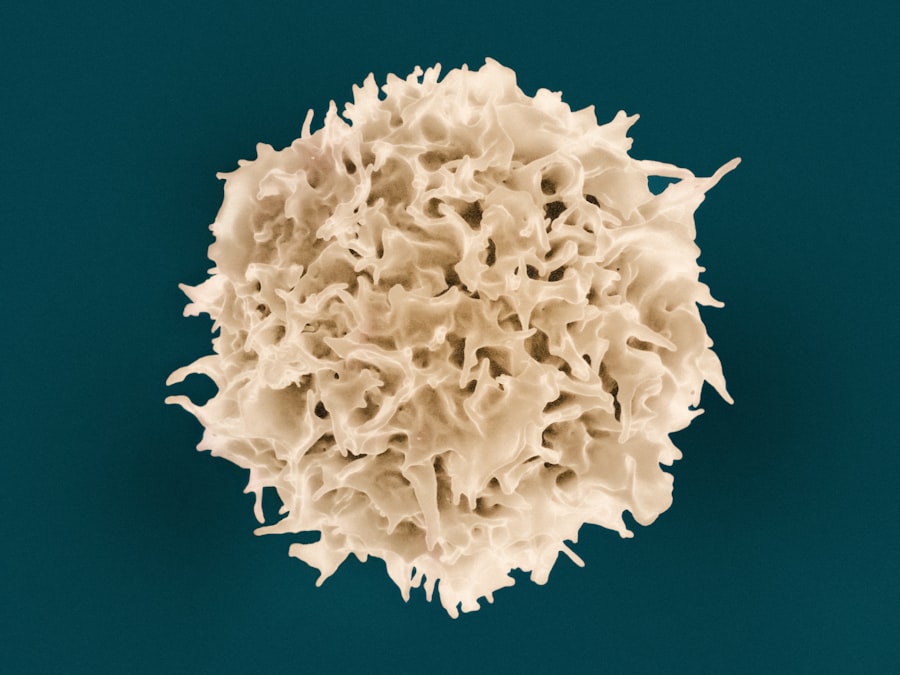
Immunotherapy has emerged as one of the most promising advancements in oncology, harnessing the body’s immune system to fight cancer more effectively. Unlike traditional treatments that directly target tumor cells, immunotherapy aims to enhance or restore the immune system’s ability to recognize and destroy cancer cells. This innovative approach has led to remarkable breakthroughs in treating various malignancies, including melanoma, lung cancer, and hematologic cancers.
One of the most notable classes of immunotherapy is immune checkpoint inhibitors, which work by blocking proteins that inhibit immune responses against tumors. For example, pembrolizumab (Keytruda) and nivolumab (Opdivo) are programmed cell death protein 1 (PD-1) inhibitors that have shown significant efficacy in treating advanced melanoma and NSCLThe success of these agents has not only improved survival rates but has also reshaped treatment paradigms, leading to their incorporation into first-line therapy for several cancers. The impact of immunotherapy extends beyond survival; it has also introduced the concept of durable responses, where some patients experience long-lasting remission even after discontinuing treatment.
Advancements in Early Detection and Screening
| Metric | Description | Typical Value/Range | Unit |
|---|---|---|---|
| Patient Enrollment Rate | Number of patients enrolled per month in oncology trials | 5 – 50 | patients/month |
| Trial Phases | Distribution of oncology clinical trials by phase | Phase I: 20%, Phase II: 40%, Phase III: 30%, Phase IV: 10% | percentage |
| Median Progression-Free Survival (PFS) | Median time patients live without disease progression | 6 – 18 | months |
| Overall Survival (OS) | Median overall survival time of patients in trials | 12 – 36 | months |
| Adverse Event Rate | Percentage of patients experiencing treatment-related adverse events | 30% – 70% | percentage |
| Response Rate | Percentage of patients showing tumor size reduction | 20% – 60% | percentage |
| Trial Duration | Average length of oncology clinical trials | 12 – 48 | months |
| Biomarker Testing Rate | Percentage of patients tested for relevant biomarkers | 50% – 90% | percentage |
Early detection and screening are critical components in the fight against cancer, as they can significantly improve treatment outcomes and survival rates. Advances in technology have led to the development of more sensitive and specific screening methods that can identify cancers at earlier stages when they are more amenable to treatment. For instance, mammography has long been a standard screening tool for breast cancer, but recent innovations such as digital mammography and breast MRI have enhanced detection rates, particularly in high-risk populations.
In addition to imaging techniques, liquid biopsies have emerged as a groundbreaking advancement in early detection. These minimally invasive tests analyze circulating tumor DNA (ctDNA) or other biomarkers present in blood samples, providing valuable insights into tumor dynamics without the need for invasive tissue biopsies. Liquid biopsies hold great promise for detecting cancers at earlier stages and monitoring treatment response or disease recurrence over time.
The integration of these advanced screening methods into routine clinical practice could revolutionize cancer detection and lead to earlier interventions that save lives.
Role of Genetics and Genomics in Oncology Research

The role of genetics and genomics in oncology research has become increasingly prominent as scientists seek to unravel the complex genetic underpinnings of cancer. Understanding the genetic alterations that drive tumorigenesis is essential for developing targeted therapies and improving patient outcomes. The Human Genome Project laid the groundwork for this field by mapping the entire human genome, providing researchers with invaluable resources to identify genes associated with various cancers.
One significant advancement in this area is the identification of hereditary cancer syndromes linked to specific genetic mutations. For example, mutations in BRCA1 and BRCA2 genes are well-known risk factors for breast and ovarian cancers. Genetic testing for these mutations allows for risk assessment and informed decision-making regarding preventive measures or early interventions for at-risk individuals.
Furthermore, genomic profiling of tumors can reveal actionable mutations that guide treatment decisions, exemplifying how genetics plays a crucial role in personalizing cancer care.
Clinical Trials and their Importance in Oncology Research
Clinical trials are fundamental to advancing oncology research and improving treatment options for patients with cancer. These carefully designed studies evaluate new therapies’ safety and efficacy before they become standard practice. Clinical trials can take various forms, including phase I trials that assess safety and dosage, phase II trials that evaluate efficacy in a specific population, and phase III trials that compare new treatments against standard therapies in larger cohorts.
Participation in clinical trials offers patients access to cutting-edge treatments that may not yet be available through conventional care pathways. Moreover, clinical trials contribute significantly to our understanding of cancer biology and treatment responses across diverse populations. For instance, recent trials investigating combination therapies have provided insights into synergistic effects that enhance treatment efficacy while minimizing toxicity.
The data generated from these trials not only inform clinical practice but also shape future research directions by identifying areas where further investigation is warranted.
Future Directions and Promising Developments in Oncology Clinical Research
The future of oncology clinical research is poised for exciting developments driven by technological advancements and a deeper understanding of cancer biology. One promising direction is the integration of artificial intelligence (AI) and machine learning into oncology research. These technologies can analyze vast datasets from genomic studies, clinical trials, and electronic health records to identify patterns that may inform treatment decisions or predict patient outcomes more accurately.
Additionally, ongoing research into novel therapeutic modalities such as CAR T-cell therapy exemplifies the potential for innovative approaches to revolutionize cancer treatment. CAR T-cell therapy involves engineering a patient’s T cells to recognize and attack cancer cells more effectively. This approach has shown remarkable success in treating certain hematologic malignancies and is being explored for solid tumors as well.
As we look ahead, collaboration among researchers, clinicians, and patients will be essential in driving progress in oncology clinical research. By fostering partnerships across disciplines and engaging patients in research initiatives, we can accelerate the translation of scientific discoveries into meaningful advancements in cancer care. The future holds great promise for improving outcomes for patients facing this complex disease through continued innovation and dedication to research excellence.