Oncology clinical research is a vital field that focuses on the study of cancer, its causes, treatments, and outcomes. This area of research encompasses a wide range of activities, including laboratory studies, clinical trials, and epidemiological investigations. The primary goal is to improve the understanding of cancer biology and to develop more effective therapies that can enhance patient outcomes.
As cancer remains one of the leading causes of death worldwide, the importance of rigorous research in this domain cannot be overstated. The complexity of cancer, characterized by its heterogeneity and adaptability, necessitates a multifaceted approach to research that integrates various scientific disciplines. The landscape of oncology clinical research has evolved significantly over the past few decades.
Advances in technology, such as genomic sequencing and bioinformatics, have transformed the way researchers approach cancer studies. These innovations have enabled scientists to delve deeper into the molecular underpinnings of cancer, leading to the identification of novel biomarkers and therapeutic targets. Furthermore, the integration of patient data and real-world evidence into research frameworks has enhanced the relevance and applicability of findings, ultimately aiming to bridge the gap between laboratory discoveries and clinical practice.
Key Takeaways
- Oncology clinical research is crucial for developing new cancer treatments and improving patient outcomes.
- Innovations like immunotherapy and targeted therapies have transformed cancer treatment approaches.
- Personalized medicine tailors treatments based on individual genetic profiles, enhancing effectiveness.
- Early detection advancements improve diagnosis accuracy and increase survival rates.
- Ongoing clinical trials drive future progress and the evolution of precision oncology care.
Innovations in Cancer Treatment
The field of oncology has witnessed remarkable innovations in cancer treatment over recent years, driven by a combination of scientific breakthroughs and technological advancements. One notable innovation is the development of novel chemotherapeutic agents that are designed to be more effective while minimizing side effects. For instance, liposomal formulations of traditional chemotherapeutics have been developed to enhance drug delivery to tumor sites while reducing systemic toxicity.
This targeted approach not only improves patient tolerance but also increases the likelihood of achieving therapeutic efficacy. In addition to traditional chemotherapy, radiation therapy has also seen significant advancements. Techniques such as stereotactic body radiation therapy (SBRT) and intensity-modulated radiation therapy (IMRT) allow for precise targeting of tumors while sparing surrounding healthy tissues.
These innovations have led to improved outcomes for patients with localized cancers, reducing the incidence of treatment-related complications. Moreover, the integration of imaging technologies, such as PET and MRI, into radiation planning has further refined treatment delivery, ensuring that radiation is administered with utmost accuracy.
Personalized Medicine in Oncology
Personalized medicine represents a paradigm shift in oncology, moving away from a one-size-fits-all approach to a more tailored strategy that considers individual patient characteristics. This approach is grounded in the understanding that each patient’s cancer is unique, influenced by genetic, environmental, and lifestyle factors. By leveraging genomic profiling and molecular diagnostics, oncologists can identify specific mutations and alterations within a patient’s tumor, allowing for the selection of targeted therapies that are more likely to be effective.
For example, patients with non-small cell lung cancer (NSCLC) harboring mutations in the EGFR gene can benefit from targeted therapies such as erlotinib or gefitinib. These drugs specifically inhibit the aberrant signaling pathways activated by the mutated EGFR protein, leading to improved response rates compared to traditional chemotherapy. The success of personalized medicine in oncology underscores the importance of understanding tumor biology and highlights the need for ongoing research to identify new biomarkers that can guide treatment decisions.
Immunotherapy and its Impact on Cancer Treatment
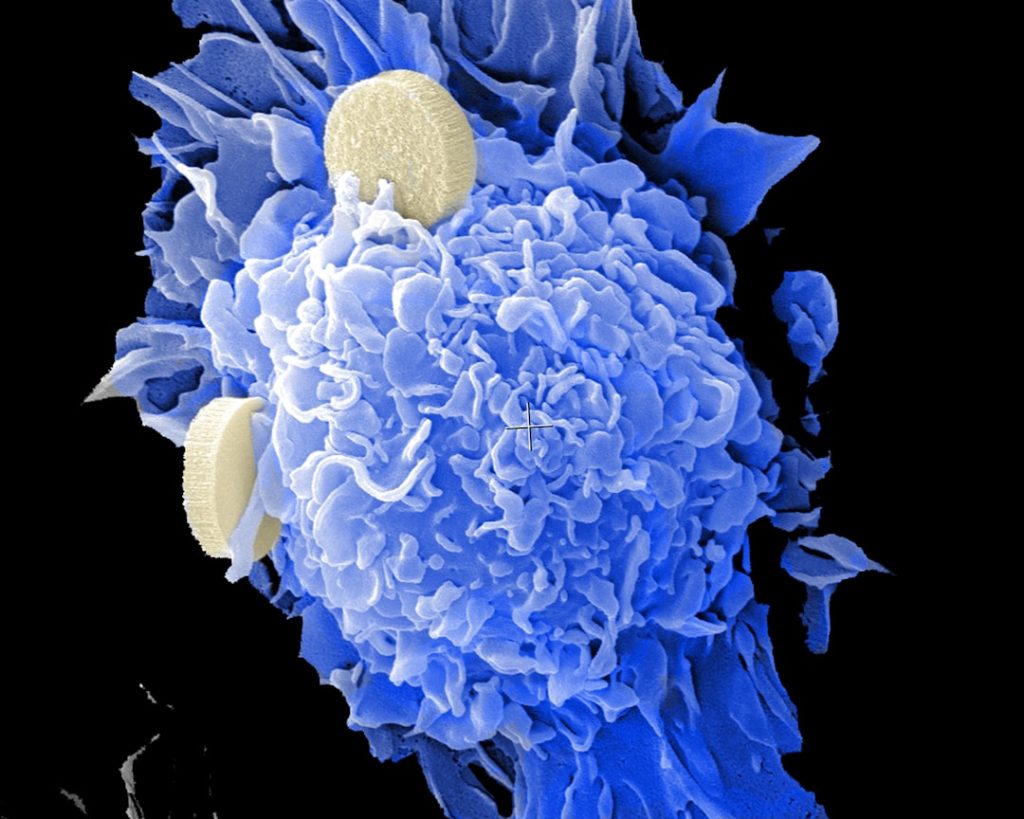
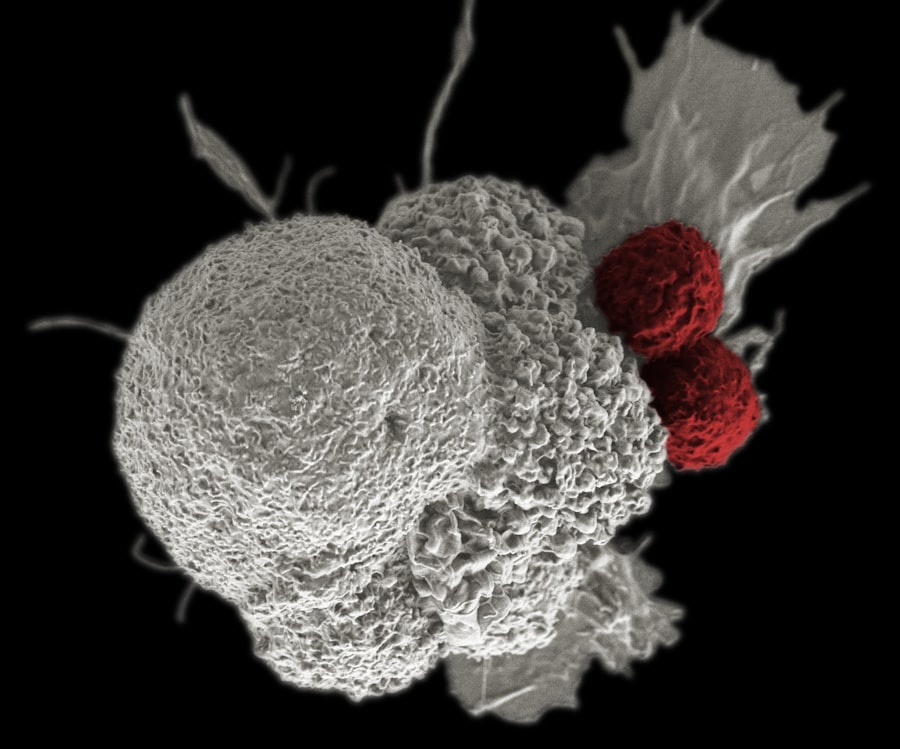
Immunotherapy has emerged as one of the most promising advancements in cancer treatment over the past decade. This innovative approach harnesses the body’s immune system to recognize and attack cancer cells. Unlike traditional therapies that directly target tumor cells, immunotherapy aims to enhance the immune response against cancer by utilizing various strategies, including checkpoint inhibitors, monoclonal antibodies, and CAR T-cell therapy.
Checkpoint inhibitors, such as pembrolizumab and nivolumab, have revolutionized the treatment landscape for several malignancies, including melanoma and lung cancer. These agents work by blocking proteins that inhibit immune responses, thereby unleashing T cells to target and destroy cancer cells. The remarkable success of these therapies has led to durable responses in some patients who previously had limited treatment options.
For instance, patients with advanced melanoma treated with nivolumab have shown significant improvements in overall survival rates compared to those receiving conventional therapies. CAR T-cell therapy represents another groundbreaking advancement in immunotherapy. This approach involves engineering a patient’s T cells to express chimeric antigen receptors (CARs) that specifically target tumor antigens.
The success of CAR T-cell therapy in hematological malignancies, such as acute lymphoblastic leukemia (ALL) and certain types of lymphoma, has demonstrated its potential to achieve complete remission in patients with otherwise refractory disease. The ongoing research into optimizing CAR T-cell therapy for solid tumors is an exciting area that holds promise for expanding its applicability.
Targeted Therapies and Precision Medicine
| Metric | Description | Typical Value/Range | Unit |
|---|---|---|---|
| Patient Enrollment Rate | Number of patients enrolled per month in oncology trials | 5 – 50 | patients/month |
| Trial Phases | Distribution of clinical trials by phase | Phase I: 20%, Phase II: 40%, Phase III: 30%, Phase IV: 10% | percentage |
| Median Progression-Free Survival (PFS) | Median time patients live without disease progression | 6 – 18 | months |
| Overall Survival (OS) | Median time patients survive after treatment | 12 – 36 | months |
| Adverse Event Rate | Percentage of patients experiencing significant side effects | 10% – 40% | percentage |
| Response Rate | Percentage of patients showing tumor size reduction | 20% – 60% | percentage |
| Trial Duration | Average length of oncology clinical trials | 12 – 48 | months |
| Biomarker Utilization | Percentage of trials using biomarkers for patient selection | 30% – 70% | percentage |
Targeted therapies are designed to interfere with specific molecular targets involved in cancer progression. These therapies are often developed based on a comprehensive understanding of the genetic alterations present in tumors. By focusing on these specific targets, oncologists can provide treatments that are more effective and less toxic than traditional chemotherapy.
One prominent example of targeted therapy is trastuzumab (Herceptin), which is used in HER2-positive breast cancer. This monoclonal antibody specifically binds to the HER2 protein overexpressed on the surface of cancer cells, inhibiting their growth and promoting apoptosis. The introduction of trastuzumab has significantly improved outcomes for patients with HER2-positive breast cancer, transforming it from a poor-prognosis disease into one with favorable outcomes when treated appropriately.
Moreover, precision medicine extends beyond targeted therapies; it encompasses a broader approach that integrates genetic profiling with clinical decision-making. The use of next-generation sequencing (NGS) allows for comprehensive analysis of tumor DNA, identifying actionable mutations that can guide therapy selection. For instance, patients with metastatic colorectal cancer may benefit from targeted agents like cetuximab or panitumumab if they possess specific KRAS wild-type mutations.
This level of precision ensures that patients receive treatments tailored to their unique tumor characteristics.
Advancements in Early Detection and Diagnosis

Early detection of cancer is crucial for improving survival rates and treatment outcomes. Recent advancements in diagnostic technologies have significantly enhanced our ability to identify cancers at earlier stages when they are more amenable to treatment. Liquid biopsies represent one such innovation; these tests analyze circulating tumor DNA (ctDNA) or other biomarkers present in blood samples, providing a non-invasive method for detecting malignancies.
Liquid biopsies have shown promise in various cancers, including lung and breast cancers. For instance, studies have demonstrated that ctDNA analysis can detect mutations associated with resistance to targeted therapies even before clinical progression is evident. This capability allows for timely adjustments in treatment strategies, potentially improving patient outcomes.
In addition to liquid biopsies, advancements in imaging technologies have also played a pivotal role in early detection. Techniques such as digital mammography and 3D tomosynthesis have improved breast cancer screening by providing clearer images and reducing false positives. Similarly, advancements in MRI technology have enhanced the detection of prostate cancer through multiparametric imaging techniques that assess both anatomical and functional characteristics of tumors.
Clinical Trials and their Role in Oncology Research
Clinical trials are the cornerstone of oncology research, serving as a critical mechanism for evaluating new treatments and interventions. These studies are designed to assess the safety and efficacy of novel therapies while adhering to rigorous scientific standards. The process typically involves several phases: Phase I trials focus on safety and dosage; Phase II trials evaluate efficacy; and Phase III trials compare new treatments against standard care.
Participation in clinical trials offers patients access to cutting-edge therapies that may not yet be available through standard treatment protocols. For example, many patients with advanced cancers enroll in trials testing new immunotherapies or targeted agents that show promise based on preclinical data. The results from these trials not only contribute to scientific knowledge but also have the potential to change clinical practice guidelines if they demonstrate significant benefits.
Moreover, clinical trials are essential for understanding the diverse responses among different patient populations. By including diverse cohorts in trials—considering factors such as age, ethnicity, and comorbidities—researchers can gain insights into how various demographics respond to treatments. This information is crucial for developing inclusive treatment strategies that address health disparities within oncology.
Future Directions in Oncology Clinical Research
The future of oncology clinical research is poised for transformative changes driven by technological advancements and an increasing understanding of cancer biology. One promising direction is the integration of artificial intelligence (AI) and machine learning into research methodologies. These technologies can analyze vast datasets from genomic studies, clinical trials, and patient records to identify patterns that may not be apparent through traditional analysis methods.
AI-driven algorithms could assist in predicting patient responses to specific treatments based on their genetic profiles. Additionally, there is a growing emphasis on collaborative research efforts across institutions and disciplines. Initiatives such as The Cancer Genome Atlas (TCGA) have demonstrated the power of large-scale collaborations in generating comprehensive datasets that can inform future studies.
By pooling resources and expertise from various stakeholders—including academic institutions, pharmaceutical companies, and regulatory agencies—oncology research can accelerate the development of innovative therapies. Furthermore, patient-centered approaches are becoming increasingly important in shaping future research directions. Engaging patients in the design and implementation of clinical trials ensures that their perspectives are considered throughout the research process.
This shift towards patient involvement not only enhances recruitment efforts but also fosters a sense of ownership among participants regarding their treatment journeys. In conclusion, oncology clinical research continues to evolve rapidly, driven by innovations in treatment modalities and an enhanced understanding of cancer biology. As researchers strive to unravel the complexities of this disease, ongoing collaboration and technological integration will be essential for advancing patient care and improving outcomes across diverse populations affected by cancer.