Ovarian cancer remains one of the most challenging malignancies to diagnose and treat, primarily due to its often asymptomatic nature in the early stages. Clinical trials play a pivotal role in advancing our understanding of this disease and developing new therapeutic strategies. These trials are essential for evaluating the safety and efficacy of novel treatments, ranging from chemotherapy regimens to cutting-edge immunotherapies.
They provide a structured environment for researchers to test hypotheses and gather data that can lead to improved patient outcomes. The landscape of ovarian cancer clinical trials is diverse, encompassing various phases that assess everything from drug safety to long-term efficacy. Phase I trials focus on determining the maximum tolerated dose of a new treatment, while Phase II trials evaluate its effectiveness in a larger group of patients.
Phase III trials are often the most critical, as they compare the new treatment against standard therapies to establish its superiority or equivalence. The participation of patients in these trials is crucial, as it not only contributes to scientific knowledge but also offers access to potentially life-saving therapies that may not yet be available through standard care.
Key Takeaways
- Ovarian cancer clinical trials are crucial for developing new, effective treatments.
- Targeted therapies and personalized medicine are improving treatment specificity and outcomes.
- Immunotherapy shows promise in enhancing the immune response against ovarian cancer.
- Advances in early detection and screening aim to diagnose ovarian cancer sooner.
- Combination therapies and genetic testing are key to optimizing patient-centered treatment strategies.
Targeted Therapies and Personalized Medicine
Targeted therapies represent a significant advancement in the treatment of ovarian cancer, focusing on specific molecular targets associated with tumor growth and progression. Unlike traditional chemotherapy, which indiscriminately affects rapidly dividing cells, targeted therapies aim to disrupt the specific pathways that cancer cells exploit for survival and proliferation. For instance, PARP inhibitors, such as olaparib and rucaparib, have shown remarkable efficacy in patients with BRCA1 or BRCA2 mutations, which are linked to hereditary breast and ovarian cancer syndromes.
These drugs work by exploiting the DNA repair deficiencies in cancer cells, leading to their death while sparing normal cells. Personalized medicine takes this concept a step further by tailoring treatment based on the individual characteristics of each patient’s tumor. This approach involves comprehensive genomic profiling to identify mutations and alterations that may influence treatment response.
For example, patients with high-grade serous ovarian carcinoma may benefit from therapies targeting specific genetic alterations, such as those involving the PI3K/AKT/mTOR pathway. By understanding the unique genetic makeup of a patient’s tumor, oncologists can select therapies that are more likely to be effective, thereby improving outcomes and minimizing unnecessary side effects.
Immunotherapy and Ovarian Cancer

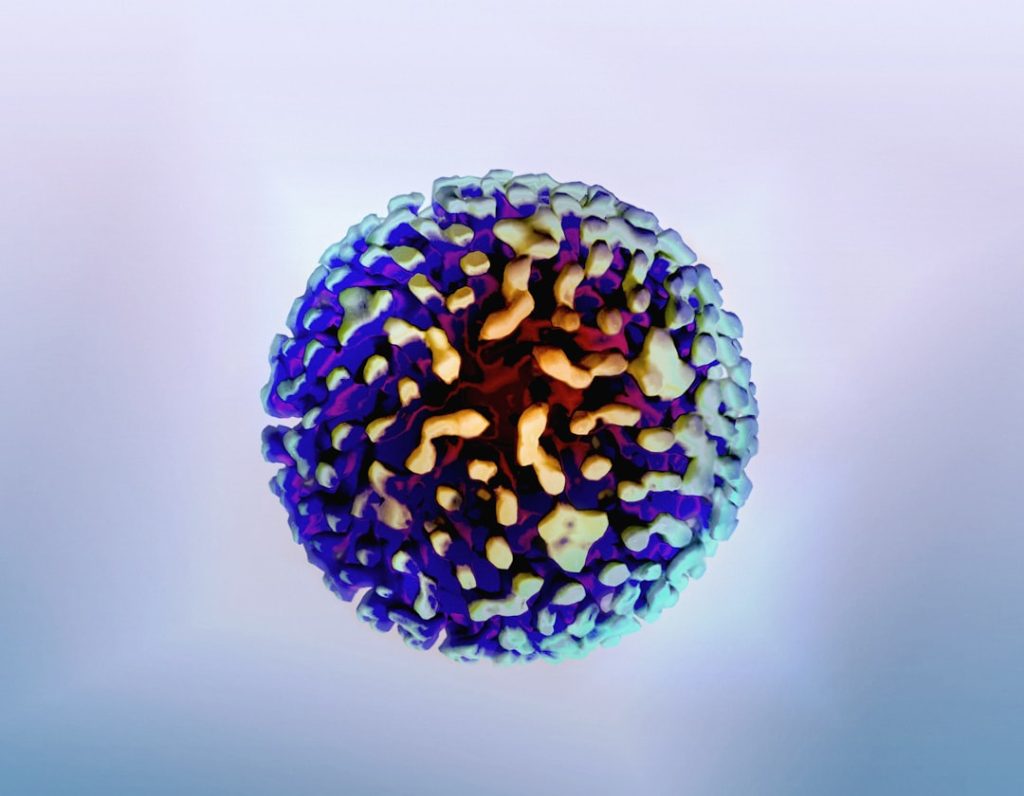
Immunotherapy has emerged as a promising avenue for treating ovarian cancer, harnessing the body’s immune system to recognize and attack cancer cells. Various strategies are being explored, including immune checkpoint inhibitors, which block proteins that inhibit immune responses, thereby enhancing the ability of T-cells to target tumors. Drugs like pembrolizumab and nivolumab have shown potential in clinical trials for ovarian cancer, particularly in patients with microsatellite instability or mismatch repair deficiency.
Another innovative approach involves the use of therapeutic vaccines designed to stimulate an immune response specifically against ovarian cancer antigens. For instance, the vaccine known as OVAX has been investigated in clinical trials for its ability to elicit a robust immune response in patients with advanced ovarian cancer. Additionally, adoptive cell transfer techniques, such as CAR T-cell therapy, are being evaluated for their effectiveness in targeting ovarian cancer cells.
These therapies represent a shift towards more innovative treatment modalities that could significantly alter the prognosis for patients with this challenging disease.
Advancements in Early Detection and Screening
Early detection of ovarian cancer is critical for improving survival rates, yet it remains a significant challenge due to the lack of effective screening methods. Recent advancements in biomarker research have opened new avenues for identifying ovarian cancer at earlier stages. The CA-125 blood test has long been used as a tumor marker; however, its specificity is limited, leading to false positives and negatives.
Researchers are now investigating additional biomarkers, such as HE4 and the Risk of Ovarian Malignancy Algorithm (ROMA), which combine multiple factors to enhance diagnostic accuracy. Moreover, imaging technologies are evolving to improve early detection capabilities. Innovations in ultrasound techniques and magnetic resonance imaging (MRI) are being explored for their potential to identify ovarian masses more accurately.
The integration of artificial intelligence (AI) into imaging analysis is also showing promise in enhancing diagnostic precision by identifying subtle patterns that may be indicative of malignancy. These advancements could lead to earlier interventions and better outcomes for women diagnosed with ovarian cancer.
Combination Therapies and Treatment Approaches
| Metric | Value | Notes |
|---|---|---|
| Number of Active Clinical Trials | 350+ | Global count as of 2024 |
| Phases of Trials | Phase 1, Phase 2, Phase 3, Phase 4 | Distribution varies by trial |
| Common Trial Interventions | Targeted Therapy, Chemotherapy, Immunotherapy, Surgery | Multiple modalities tested |
| Average Enrollment Size | 50 – 300 participants | Depends on trial phase and design |
| Primary Outcome Measures | Progression-Free Survival, Overall Survival, Response Rate | Key efficacy endpoints |
| Trial Locations | North America, Europe, Asia, Australia | Multinational participation |
| Enrollment Criteria | Confirmed Ovarian Cancer Diagnosis, Age 18+, Performance Status | Varies by trial specifics |
| Common Biomarkers Studied | BRCA1/2, CA-125, HE4 | Used for patient stratification |
Combination therapies are increasingly recognized as a powerful strategy in the management of ovarian cancer, leveraging multiple mechanisms of action to enhance treatment efficacy. The rationale behind this approach is that using different agents can target various pathways involved in tumor growth and resistance, potentially overcoming limitations associated with single-agent therapies. For example, combining chemotherapy with targeted agents like bevacizumab has been shown to improve progression-free survival in certain patient populations.
Clinical trials are actively investigating various combinations of therapies, including the pairing of immunotherapies with traditional chemotherapy or targeted agents. The rationale is that chemotherapy can induce immunogenic cell death, making tumors more susceptible to immune-mediated destruction when followed by immunotherapy. Additionally, combining PARP inhibitors with other agents such as immunotherapies or anti-angiogenic drugs is being explored to enhance treatment responses in patients with BRCA mutations or homologous recombination deficiency.
The Role of Genetic Testing in Clinical Trials

Genetic testing has become an integral component of clinical trials for ovarian cancer, providing critical insights into tumor biology and guiding treatment decisions. Testing for specific genetic mutations, such as BRCA1 and BRCA2, not only informs eligibility for targeted therapies like PARP inhibitors but also helps identify patients who may benefit from preventive measures or family screening programs. The identification of other genetic alterations through comprehensive genomic profiling can further refine treatment strategies and improve patient outcomes.
In clinical trial settings, genetic testing allows researchers to stratify patients based on their molecular profiles, ensuring that those most likely to respond to a particular therapy are included in relevant studies. This precision medicine approach enhances the likelihood of successful outcomes while minimizing exposure to ineffective treatments. Furthermore, ongoing research into novel biomarkers continues to expand the landscape of genetic testing, paving the way for more personalized approaches in clinical trials.
Patient-Centered Research and Quality of Life
As the field of oncology evolves, there is an increasing recognition of the importance of patient-centered research that prioritizes quality of life alongside clinical outcomes. Ovarian cancer clinical trials are increasingly incorporating patient-reported outcomes (PROs) to assess how treatments impact patients’ daily lives, emotional well-being, and overall satisfaction with care. This shift acknowledges that survival is not the sole measure of success; how patients feel during and after treatment is equally important.
Incorporating quality-of-life assessments into clinical trials allows researchers to gain valuable insights into the side effects and burdens associated with various treatments. For instance, studies may evaluate how different chemotherapy regimens affect fatigue levels or emotional distress among patients. By understanding these factors, clinicians can make more informed decisions about treatment options and provide supportive care tailored to individual needs.
This holistic approach fosters a more compassionate healthcare environment where patient experiences are valued alongside clinical efficacy.
Future Directions and Promising Developments
The future of ovarian cancer research is bright, with numerous promising developments on the horizon that hold the potential to transform treatment paradigms. Advances in precision medicine continue to evolve rapidly, with ongoing efforts to identify novel biomarkers that can predict treatment responses more accurately. The integration of multi-omics approaches—combining genomics, proteomics, and metabolomics—may provide deeper insights into tumor biology and facilitate more personalized therapeutic strategies.
Additionally, ongoing research into novel therapeutic agents is expanding the arsenal available for treating ovarian cancer. Investigational drugs targeting emerging pathways involved in tumorigenesis are being evaluated in clinical trials, offering hope for patients who have exhausted standard treatment options. Furthermore, collaborations between academic institutions and pharmaceutical companies are fostering innovation and accelerating the development of new therapies.
As we look ahead, it is clear that a multidisciplinary approach will be essential in tackling ovarian cancer effectively. By combining insights from genetics, immunology, and patient-centered care, researchers and clinicians can work together to develop comprehensive strategies that not only extend survival but also enhance the quality of life for those affected by this challenging disease. The commitment to advancing research through clinical trials remains a cornerstone in the fight against ovarian cancer, promising a future where early detection and effective treatments become a reality for all patients.