Ovarian cancer, a complex and challenging disease, remains a significant health concern globally. For decades, treatment paradigms largely revolved around surgery and platinum-based chemotherapy. However, recent advancements in research and clinical trials are beginning to reshape this landscape, offering new avenues for diagnosis, treatment, and improved patient outcomes. This article explores key developments in ovarian cancer trials, highlighting the ongoing efforts to combat this disease.
The elusive nature of ovarian cancer often leads to diagnosis at advanced stages, significantly impacting prognosis. Early detection is a cornerstone of improved survival, and research continues to focus on identifying reliable biomarkers and screening methods.
Circulating Cell-Free DNA (cfDNA) Analysis
One promising area involves the analysis of circulating cell-free DNA (cfDNA). These fragments of DNA, shed by tumor cells into the bloodstream, can carry genetic alterations characteristic of the cancer. Researchers are exploring cfDNA as a “liquid biopsy,” a non-invasive method for early detection and disease monitoring. Studies are investigating the sensitivity and specificity of cfDNA analysis in discriminating between benign and malignant pelvic masses, as well as its utility in detecting recurrence. Trials are underway to validate algorithms that combine cfDNA methylation patterns and genomic alterations for enhanced diagnostic accuracy. For example, some studies are examining how specific methylation signatures in cfDNA could serve as an early alarm system, detectable even before a tumor is large enough to be visualized through imaging. This approach represents a potential paradigm shift from reactive diagnosis to proactive surveillance.
Proteomic Biomarkers
Beyond nucleic acids, proteomic biomarkers are also under investigation. Proteins secreted by ovarian cancer cells can be detected in blood samples, offering another potential avenue for early detection. Research focuses on identifying panels of proteins that, when analyzed together, provide a more robust diagnostic signal than individual markers. For instance, studies are evaluating panels that combine CA-125, HE4, and other novel protein markers, often integrating them with risk assessment algorithms. The aim is to create a more sophisticated “net” of markers that can catch early-stage disease with greater precision than current standard-of-care methods. This involves large-scale cohort studies to validate these protein panels across diverse patient populations, ensuring their applicability and generalizability.
Imaging Modalities and Artificial Intelligence
Advances in imaging technologies, alongside the integration of artificial intelligence (AI), are also contributing to early detection efforts. High-resolution imaging techniques, such as advanced MRI and PET scans, are being refined to better visualize minute tumor lesions. AI algorithms are being developed to analyze these images, identifying subtle patterns that might be missed by the human eye. This collaborative approach between imaging and AI acts as a magnifying glass, potentially revealing cancerous cells at their nascent stages. Clinical trials are evaluating the efficacy of these AI-enhanced imaging protocols in screening high-risk individuals and improving the characterization of indeterminate ovarian masses. The goal is to move beyond simply identifying a mass to accurately classifying its potential for malignancy.
Novel Therapeutic Approaches
While surgery and platinum-based chemotherapy remain central to ovarian cancer treatment, ongoing trials are exploring innovative therapeutic strategies, targeting disease pathways with increasing specificity. This represents a shift from broad-spectrum toxic therapies to more tailored, precise interventions.
PARP Inhibitors and Beyond
Poly (ADP-ribose) polymerase (PARP) inhibitors represent a significant breakthrough, particularly for patients with BRCA mutations or homologous recombination deficiency (HRD). These drugs leverage the Achilles’ heel of cancer cells with impaired DNA repair pathways. Clinical trials have established their role in maintenance therapy, significantly prolonging progression-free survival. Current research is expanding on this foundation, investigating PARP inhibitor combinations with other agents, such as anti-angiogenic drugs or immunotherapy, to overcome resistance and broaden their applicability. Consider the PARP inhibitor as a lock, and the BRCA mutation as the key that allows it to effectively halt the cancer cell’s ability to repair itself. Researchers are now looking for other “keys” or combinations of “keys” that can unlock similar vulnerabilities in a wider array of ovarian cancers.
Antibody-Drug Conjugates (ADCs)
Antibody-drug conjugates (ADCs) are emerging as a promising class of therapeutics. These agents consist of a monoclonal antibody precisely linked to a potent cytotoxic drug. The antibody component acts as a homing missile, selectively binding to specific tumor cell surface antigens, thereby delivering the chemotherapy payload directly to cancerous cells while minimizing damage to healthy tissues. Trials are evaluating ADCs targeting various antigens, such as FRα (folate receptor alpha), which is frequently overexpressed in ovarian cancer. The precision of ADCs offers the potential for improved efficacy with a more favorable side effect profile compared to conventional chemotherapy. Imagine a Trojan horse, where the antibody stealthily delivers its deadly cargo directly into the cancer cell, leaving normal cells largely untouched.
Immunotherapy and Combination Strategies
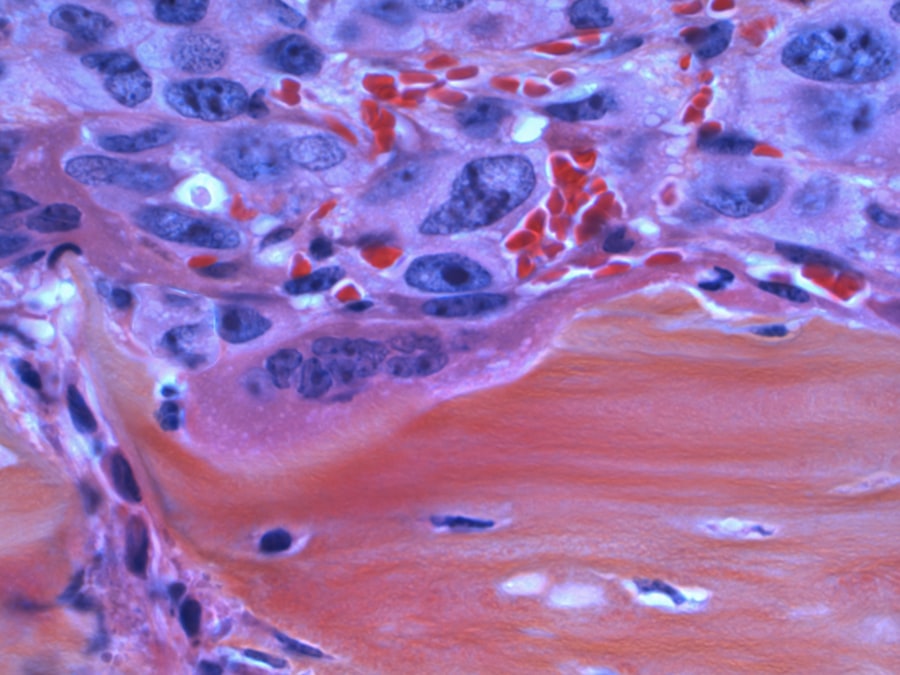
Immunotherapy, which harnesses the body’s own immune system to fight cancer, has shown benefit in various malignancies. In ovarian cancer, its efficacy as a standalone treatment has been modest. However, ongoing trials are exploring immunotherapy in combination with other modalities, such as chemotherapy, PARP inhibitors, or anti-angiogenic agents. The rationale is to create a more hospitable tumor microenvironment for immune cell infiltration and activation. For example, some trials are examining the combination of immune checkpoint inhibitors with PARP inhibitors, hypothesizing that the PARP inhibitor’s DNA damage induction might increase tumor immunogenicity, making the cancer cells more visible to the immune system. This multifaceted approach seeks to dismantle the tumor’s defenses from multiple angles.
Personalized Medicine and Genomic Profiling

The notion of “one-size-fits-all” treatment is increasingly being replaced by a personalized approach, driven by a deeper understanding of the molecular heterogeneity of ovarian cancer. Genomic profiling is acting as a compass, guiding treatment decisions.
Molecular Subtyping of Ovarian Cancer
Ovarian cancer is not a single disease but a collection of distinct entities with varying molecular characteristics and clinical behaviors. Genomic profiling allows for the molecular subtyping of tumors, identifying specific genetic alterations, gene expression patterns, and epigenetic modifications. This granular understanding enables the selection of targeted therapies that are most likely to be effective for an individual patient’s tumor. For example, a patient with a specific gene fusion might respond favorably to a targeted inhibitor that would be ineffective in a patient without that alteration. This shifts the focus from treating the organ to treating the molecular signature of the disease.
Tumor Mutational Burden (TMB) and Microsatellite Instability (MSI)
Tumor mutational burden (TMB) and microsatellite instability (MSI) are emerging as predictive biomarkers for response to immunotherapy in certain cancers. While their role in ovarian cancer is still being elucidated, clinical trials are actively investigating their utility in identifying patients who are more likely to benefit from immune checkpoint inhibitors. High TMB or MSI suggests a greater number of genetic errors within the tumor, potentially making it more recognizable to the immune system. Analyzing these markers allows clinicians to discern which patients might have a “window” of opportunity for effective immunotherapy. This stratification helps avoid unnecessary toxicities in patients unlikely to respond.
Germline and Somatic Testing
Comprehensive germline and somatic genetic testing is becoming standard practice. Germline testing identifies inherited genetic mutations, such as BRCA1 and BRCA2, which predispose individuals to ovarian cancer and inform treatment decisions, particularly regarding PARP inhibitors. Somatic testing, performed on tumor tissue, reveals acquired mutations specific to the cancer, guiding the selection of targeted therapies. This dual approach provides a comprehensive molecular blueprint of both the patient’s inherent risk and the tumor’s unique vulnerabilities, acting as a detailed roadmap for personalized treatment strategies.
Overcoming Treatment Resistance
A significant challenge in ovarian cancer treatment is the development of resistance to chemotherapy and targeted therapies. Trials are actively investigating mechanisms of resistance and developing strategies to circumvent them.
Re-sensitization Strategies
For patients who develop resistance to platinum-based chemotherapy, re-sensitization strategies are a critical area of research. This involves identifying agents that can restore sensitivity to platinum compounds or other cytotoxic drugs. For instance, some trials are exploring the use of inhibitors of DNA repair pathways or epigenetic modulators in combination with platinum agents, aiming to “reset” the tumor’s vulnerability. This is akin to finding the “off button” for the resistance mechanism, allowing previously effective drugs to work again.
Targeting Alternative Pathways
When tumor cells develop resistance to a particular drug, they often rely on alternative signaling pathways to survive and proliferate. Researchers are investigating these compensatory pathways as potential therapeutic targets. This involves a continuous cycle of observation, hypothesis-testing, and the development of new inhibitors. For example, if a tumor becomes resistant to a PARP inhibitor, scientists might investigate whether it has upregulated a different DNA repair mechanism that can then be targeted with a new drug. This adaptive approach is crucial as cancer cells are adept at finding workarounds.
Combination Therapies to Prevent Resistance
A proactive strategy to combat resistance involves the use of rational combination therapies upfront. By simultaneously targeting multiple pathways or engaging different mechanisms of action, the aim is to prevent the emergence of resistant clones. This is like building a multi-layered defense system, where if one barrier fails, others are still in place to contain the threat. Trials are exploring various combinations, including targeted therapy with chemotherapy, immunotherapy with PARP inhibitors, and combinations of different targeted agents. The challenge lies in identifying combinations that offer synergistic efficacy with manageable toxicity.
Supportive Care and Quality of Life
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Status |
|---|---|---|---|---|---|
| OV-101 | Phase III | 500 | PARP Inhibitor vs Placebo | Progression-Free Survival | Completed |
| GOG-3005 | Phase II | 200 | Immunotherapy + Chemotherapy | Overall Survival | Recruiting |
| OV-202 | Phase I | 50 | Targeted Therapy | Safety and Tolerability | Active, not recruiting |
| ICON8 | Phase III | 800 | Weekly vs 3-weekly Chemotherapy | Progression-Free Survival | Completed |
| AGO-OVAR 12 | Phase III | 1300 | Bevacizumab + Chemotherapy | Overall Survival | Completed |
While focusing on curative treatments is paramount, improving the quality of life for ovarian cancer patients throughout their journey is an equally important aspect of clinical trials.
Management of Treatment-Related Toxicities
Chemotherapy and targeted therapies, while effective, can cause significant side effects that impact a patient’s well-being. Clinical trials are investigating novel supportive care interventions to mitigate these toxicities. This includes studies on new antiemetics to control nausea and vomiting, agents to prevent neuropathy, and strategies to manage fatigue and pain. The goal is not just to extend life but to ensure that extended life is lived with dignity and minimal discomfort. Imagine a robust support system around the patient, absorbing the shocks and stresses of aggressive treatment.
Psychosocial Support and Survivorship Programs
The emotional and psychological burden of an ovarian cancer diagnosis and treatment can be substantial. Clinical trials are exploring the efficacy of various psychosocial interventions, including counseling, support groups, and mind-body therapies, to address anxiety, depression, and body image concerns. Furthermore, survivorship programs are being developed and evaluated to address long-term physical and mental health challenges faced by patients after completing active treatment. This holistic approach recognizes that ovarian cancer affects not just the body but the entire person, and that support extends far beyond the confines of the treatment room.
Patient-Reported Outcomes (PROs) and Shared Decision-Making
Patient-reported outcomes (PROs) are gaining increasing recognition in clinical trials. By directly capturing patients’ perspectives on their symptoms, functional status, and quality of life, PROs provide invaluable data that complements objective clinical measures. This allows for a more comprehensive understanding of treatment impact. Coupled with shared decision-making frameworks, where patients are actively involved in treatment choices based on their values and preferences, this approach ensures that care aligns with individual patient needs and priorities. This represents a fundamental shift towards patient-centric care, where the patient’s voice is not just heard, but actively shapes the course of their treatment.
In conclusion, the landscape of ovarian cancer research is undergoing a profound transformation. From refined early detection strategies and increasingly precise therapeutic agents to a greater emphasis on personalized medicine and quality of life, clinical trials are the engine driving progress. While challenges remain, the ongoing dedication of researchers, clinicians, and patients offers a beacon of hope for improved outcomes in this complex disease.



