Targeted therapies represent a significant evolution in cancer treatment, moving beyond the systemic and often indiscriminate cytotoxicity of conventional chemotherapy. These therapies operate by identifying and disabling specific molecular pathways or components critical for cancer cell growth, survival, and proliferation, while ideally sparing healthy cells. The Journal of Clinical Cancer Research frequently features studies exploring the nuances and advancements in this rapidly evolving field. This article examines key areas of progress, the challenges encountered, and future directions in targeted therapy research as documented within this prominent journal.
The concept of targeted therapy emerged from a deeper understanding of cancer biology at the molecular level. Early chemotherapy, while effective in some cancers, often resulted in broad toxicity due to its impact on rapidly dividing normal cells. The recognition that many cancers are driven by specific genetic alterations or aberrant protein activity opened the door for more precise interventions.
First-Generation Targeted Agents
Initial targeted therapies often focused on readily identifiable targets. Imatinib, a tyrosine kinase inhibitor (TKI) against BCR-ABL in chronic myeloid leukemia (CML), exemplifies this early success. This drug dramatically altered the prognosis for CML patients, demonstrating the power of molecularly guided treatment. Subsequent developments included gefitinib and erlotinib, epidermal growth factor receptor (EGFR) TKIs, which showed efficacy in non-small cell lung cancer (NSCLC) patients harboring specific EGFR mutations.
Broadening Target Spectrum
As genomic sequencing became more accessible, the catalog of actionable mutations and aberrant protein expressions expanded. This led to the development of inhibitors targeting various kinases beyond EGFR, including ALK, ROS1, BRAF, and MEK. The identification of these oncogenic drivers in diverse cancer types broadened the applicability of targeted approaches.
Mechanisms of Action and Key Targets
Targeted therapies operate through various mechanisms to disrupt cancer cell function. Understanding these mechanisms is crucial for appreciating the specificity of these treatments.
Kinase Inhibitors
Kinases are enzymes that regulate cellular processes through phosphorylation. Oncogenic kinases, often hyperactive or mutated, drive uncontrolled cell growth. Kinase inhibitors (TKIs for tyrosine kinases, or simply KIs for other kinases) block the ATP-binding site or induce conformational changes, thereby preventing substrate phosphorylation.
Tyrosine Kinase Inhibitors (TKIs)
- EGFR inhibitors: Primarily used in NSCLC. Mutations in exons 19 and 21 of the EGFR gene predict response. Resistance mechanisms often involve a secondary mutation, T790M, or activation of bypass pathways.
- ALK inhibitors: Effective in NSCLC with ALK rearrangements. Examples include crizotinib, ceritinib, and alectinib. Development of new generations addresses resistance.
- BRAF and MEK inhibitors: Crucial in melanoma and some colorectal cancers with BRAF V600E mutations. BRAF and MEK are components of the MAPK pathway; dual inhibition often mitigates resistance.
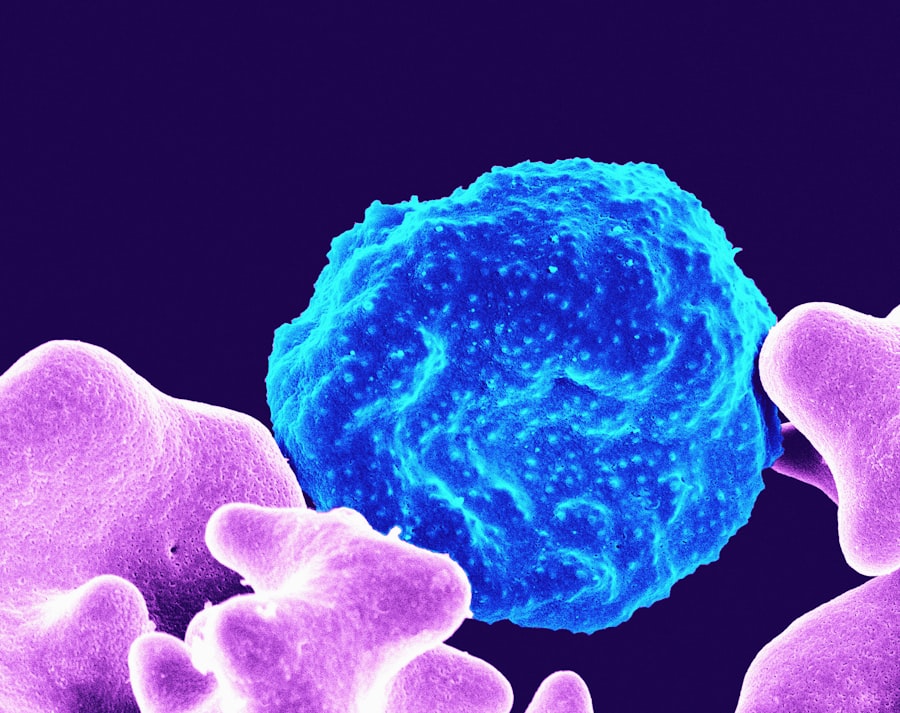
Monoclonal Antibodies
Monoclonal antibodies are proteins designed to bind specifically to antigens on cancer cells or to growth factors essential for cancer growth. This binding can trigger various anti-tumor effects.
Direct Receptor Blockade
- Trastuzumab (Herceptin): Targets the HER2 receptor, a transmembrane tyrosine kinase, overexpressed in a subset of breast and gastric cancers. It blocks downstream signaling and marks cancer cells for immune destruction.
- Cetuximab and Panitumumab: Target EGFR in colorectal cancer. They prevent ligand binding and receptor activation, modulating cell proliferation and survival pathways.
Antibody-Drug Conjugates (ADCs)
ADCs are sophisticated constructs that link a cytotoxic drug to a monoclonal antibody. The antibody delivers the “warhead” specifically to tumor cells expressing a particular antigen, enhancing drug potency while reducing systemic toxicity. Example: T-DM1 (trastuzumab emtansine) for HER2-positive breast cancer.
Other Targeted Modalities
Beyond kinase inhibitors and antibodies, other targeted approaches have emerged.
Proteasome Inhibitors
- Bortezomib: Inhibits the proteasome, a protein complex responsible for degrading cellular proteins. This leads to accumulation of misfolded proteins, inducing apoptosis in myeloma cells.
PARP Inhibitors
- Olaparib, niraparib: Target poly (ADP-ribose) polymerase (PARP), an enzyme involved in DNA repair. In cancers with defective BRCA1/2, PARP inhibition leads to synthetic lethality, effectively trapping the cell in a repair deficit that results in cell death. Primarily used in ovarian and breast cancers with BRCA mutations.
Challenges and Resistance Mechanisms
Despite the successes, targeted therapies face inherent challenges, most notably the development of resistance. Cancer cells are dynamic entities, capable of evolving under selective pressure.
Primary vs. Acquired Resistance
- Primary resistance: Where a tumor does not respond to the initial targeted therapy. This can be due to the absence of the target, concurrent activating mutations in bypass pathways, or intrinsic differences in tumor biology.
- Acquired resistance: The more common scenario, where a tumor initially responds but later progresses. This typically arises from new genetic mutations in the target gene (e.g., EGFR T790M), activation of alternative signaling pathways (e.g., MET amplification bypassing EGFR inhibition), or histological transformation.
Heterogeneity and Clonal Evolution
Tumors are not monolithic entities. Intratumoral heterogeneity refers to the presence of different subclones within a single tumor, each with distinct genetic and phenotypic characteristics. Targeted therapy, acting as a selective filter, can eliminate sensitive clones while allowing resistant ones to flourish, analogous to Darwinian selection. Monitoring clonal evolution through liquid biopsies (circulating tumor DNA) is a developing strategy to anticipate and manage resistance.
Toxicity Profile
While generally less toxic than chemotherapy, targeted therapies are not without side effects. These can be target-specific (e.g., rash with EGFR inhibitors, cardiac toxicity with HER2-targeted agents) or off-target due to inhibition of related pathways in normal cells. Careful management and dose adjustments are often required.
Advances in Precision Oncology and Biomarker Discovery
The cornerstone of targeted therapy is the identification of suitable patients through biomarkers. Advances in genomics and molecular diagnostics have been pivotal.
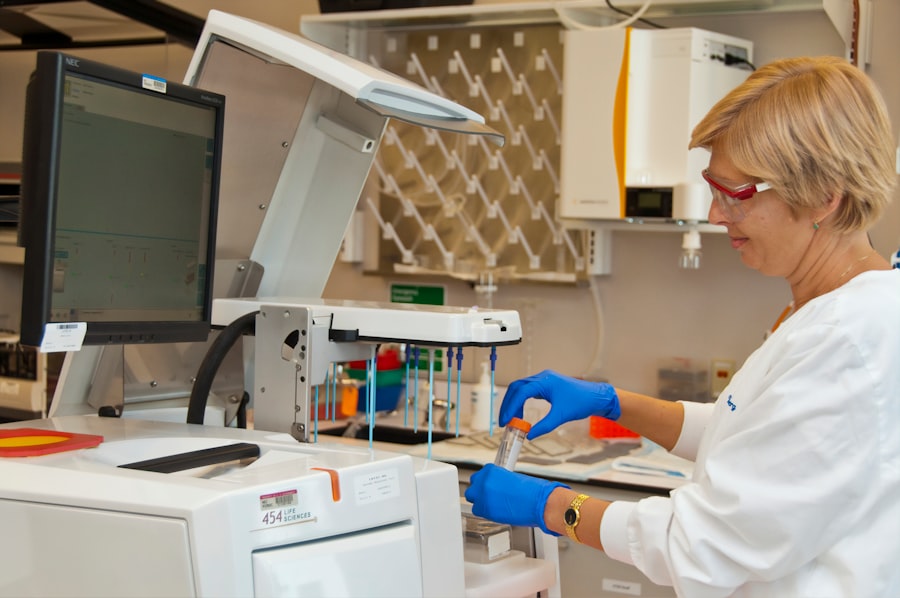
Companion Diagnostics
Companion diagnostics are tests that identify patients most likely to benefit from a specific targeted therapy. Examples include EGFR mutation testing for gefitinib and ALK rearrangement testing for crizotinib. The development and regulatory approval of these diagnostics go hand-in-hand with drug development.
Next-Generation Sequencing (NGS)
NGS has revolutionized biomarker discovery. Rather than testing for individual genes, NGS panels can simultaneously analyze hundreds of genes, identifying various mutations, fusions, and amplifications. This comprehensive molecular profiling allows for a broader assessment of potential therapeutic targets and helps in identifying resistance mechanisms. It is akin to mapping a complex city rather than just checking a few street signs.
Liquid Biopsies
Analysis of circulating tumor DNA (ctDNA) from blood samples offers a non-invasive method for molecular profiling. It provides a real-time snapshot of tumor evolution, aids in detecting minimal residual disease, and can identify emerging resistance mutations, often before clinical or radiological progression. This offers a dynamic window into the cancer’s adaptive strategies.
Immunotherapy-Targeted Therapy Combinations
The realization that targeted therapies can modulate the tumor microenvironment and enhance immune recognition has led to investigations into combination strategies. For example, some TKIs can upregulate PD-L1 expression on tumor cells, making them more susceptible to checkpoint blockade. This synergistic approach aims to overcome limitations of single-agent therapies.
Future Directions and Emerging Concepts
| Metric | Value | Year | Source |
|---|---|---|---|
| Impact Factor | 10.199 | 2023 | Journal Citation Reports |
| 5-Year Impact Factor | 11.345 | 2023 | Journal Citation Reports |
| h-index | 120 | 2023 | Scopus |
| Acceptance Rate | 18% | 2023 | Journal Website |
| Average Time to Publication | 45 days | 2023 | Journal Website |
| Publisher | American Association for Cancer Research | – | Journal Website |
| Frequency | Monthly | – | Journal Website |
The field of targeted therapies continues to evolve rapidly, pushing the boundaries of precision oncology.
Overcoming Resistance
Strategies to overcome resistance are a major focus. This includes the development of next-generation inhibitors designed to address common resistance mutations (e.g., third-generation EGFR TKIs like osimertinib), rational combination therapies, and sequential drug strategies. The goal is to stay one step ahead of the cancer’s adaptive capacity.
Pan-Cancer Approaches and Basket Trials
Rather than developing drugs for specific tumor types, some targeted therapies are being investigated across different cancers that share a common molecular alteration. Basket trials enroll patients based on their tumor’s molecular profile, irrespective of the anatomical site of origin. An example is pembrolizumab for microsatellite instability-high (MSI-H) tumors, approved across multiple tumor types.
Multi-Targeted Agents
While many early targeted therapies focused on a single target, multi-targeted agents or rational combinations are being developed to hit multiple pathways simultaneously. This aims to reduce the likelihood of resistance emerging from bypass pathways. However, the complexity of managing toxicity with multi-targeted approaches is a significant consideration.
Epigenetic Modulators
Beyond genetic mutations, epigenetic alterations (changes in gene expression without altering the DNA sequence) also drive cancer. Therapies targeting epigenetic enzymes, such as histone deacetylase inhibitors (HDACi) and DNA methyltransferase inhibitors (DNMTi), are being investigated to restore normal gene expression patterns in cancer cells. These are like resetting the control panel rather than replacing individual broken parts.
Artificial Intelligence and Machine Learning
AI and machine learning are poised to play an increasing role in precision oncology. These technologies can analyze vast genomic, proteomic, and clinical datasets to identify novel targets, predict patient response to therapy, and design optimal treatment sequences. They expedite the discovery process and personalize treatment decisions to an unprecedented degree.
Conclusion
The journey of targeted therapies, as chronicled in journals like Journal of Clinical Cancer Research, reflects the remarkable progress in our understanding and treatment of cancer. From rudimentary molecular insights to sophisticated multi-omic analyses, the specificity and efficacy of these treatments have dramatically improved patient outcomes in many settings. However, the adaptive nature of cancer, manifested through resistance mechanisms, remains a formidable adversary. The future of targeted therapies lies in further unraveling the intricate molecular landscape of cancer, developing even more precise and adaptive therapeutic agents, and integrating these with other modalities like immunotherapy. For the reader, understanding these developments is crucial for appreciating the ongoing paradigm shift from a “one-size-fits-all” approach to highly individualized cancer care. The persistent pursuit of precision in cancer treatment continues to define this field.



