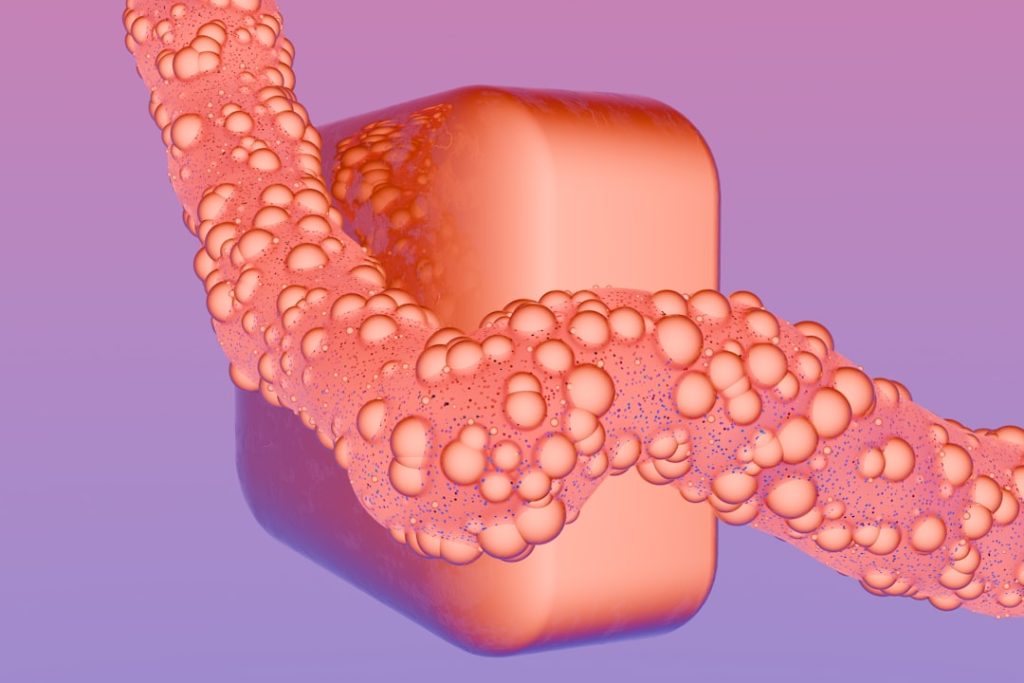
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by inflammation and ulceration of the colonic mucosa. This condition primarily affects the large intestine, leading to a range of debilitating symptoms, including abdominal pain, diarrhea, rectal bleeding, and weight loss. The etiology of UC remains complex and multifactorial, involving genetic predisposition, environmental factors, and dysregulation of the immune system.
The disease can manifest in various forms, with some patients experiencing mild symptoms while others endure severe complications that significantly impair their quality of life. The onset of ulcerative colitis typically occurs in young adulthood, although it can develop at any age. The disease course is often marked by periods of remission interspersed with flare-ups, which can be unpredictable and vary in intensity.
The chronic nature of UC necessitates ongoing management strategies to control symptoms and prevent complications such as colorectal cancer, which is a known risk associated with long-standing disease. Understanding the pathophysiology of UC is crucial for developing effective treatment modalities and improving patient outcomes.
Key Takeaways
- Ulcerative colitis is a chronic inflammatory bowel disease with various treatment options available.
- Clinical trials are essential for developing and validating new therapies for ulcerative colitis.
- Emerging treatments show promise in improving patient outcomes beyond current standard care.
- Patient involvement in clinical trials is crucial for advancing research and accessing novel therapies.
- Findings from clinical trials significantly influence future management strategies and research directions.
Current Treatment Options
The management of ulcerative colitis has evolved significantly over the years, with a variety of treatment options available to address the diverse needs of patients. The primary goal of treatment is to induce and maintain remission while minimizing side effects. First-line therapies typically include 5-aminosalicylic acid (5-ASA) compounds, such as mesalamine, which are effective in reducing inflammation in the colon.
These medications are often well-tolerated and can be administered orally or rectally, depending on the extent of the disease. In cases where 5-ASA agents are insufficient, corticosteroids may be prescribed to manage acute flare-ups due to their potent anti-inflammatory properties. However, long-term use of corticosteroids is associated with significant side effects, including osteoporosis, weight gain, and increased susceptibility to infections.
For patients who do not respond adequately to these conventional therapies, immunosuppressive agents such as azathioprine or mercaptopurine may be introduced to modulate the immune response. More recently, biologic therapies targeting specific pathways in the inflammatory process have emerged as a game-changer in UC management. Agents like infliximab and adalimumab have shown remarkable efficacy in inducing remission and maintaining long-term control of symptoms.
Role of Clinical Trials in Advancing Treatment
Clinical trials play a pivotal role in advancing the understanding and treatment of ulcerative colitis. These studies are essential for evaluating the safety and efficacy of new therapies, providing a structured framework for scientific inquiry into the disease’s complexities. By enrolling diverse patient populations, clinical trials can yield valuable insights into how different demographics respond to various treatments, ultimately guiding personalized medicine approaches.
The process of clinical trials typically involves several phases, each designed to answer specific research questions. Phase I trials focus on assessing safety and dosage in a small group of participants, while Phase II trials evaluate efficacy in a larger cohort. Phase III trials are crucial for comparing new treatments against standard therapies to determine their relative effectiveness.
The results from these trials not only contribute to the scientific community’s understanding of ulcerative colitis but also inform clinical guidelines and practice standards that shape patient care.
Promising New Therapies
Recent advancements in research have led to the development of several promising new therapies for ulcerative colitis that offer hope for improved patient outcomes. One such class of medications is Janus kinase (JAK) inhibitors, which target specific pathways involved in the inflammatory response. Tofacitinib, the first oral JAK inhibitor approved for UC, has demonstrated significant efficacy in inducing remission in patients who have not responded to conventional therapies.
Its mechanism of action involves blocking intracellular signaling pathways that contribute to inflammation, thereby reducing symptoms and promoting mucosal healing. Another exciting area of research involves the use of biologics that target specific components of the immune system. For instance, vedolizumab is an integrin inhibitor that selectively blocks the migration of inflammatory cells into the gut, effectively reducing inflammation without compromising systemic immunity.
Clinical trials have shown that vedolizumab can lead to sustained remission in patients with moderate to severe UC who have failed other treatments. Additionally, newer agents such as ustekinumab, which targets interleukin-12 and interleukin-23 pathways, are being investigated for their potential benefits in managing UC.
Patient Participation in Clinical Trials
| Trial Name | Phase | Number of Participants | Intervention | Primary Outcome | Duration (weeks) | Status |
|---|---|---|---|---|---|---|
| UC-Study-001 | Phase 3 | 450 | Biologic Therapy (Anti-TNF) | Clinical remission at week 8 | 52 | Completed |
| UC-Study-002 | Phase 2 | 120 | JAK Inhibitor | Endoscopic improvement at week 12 | 24 | Recruiting |
| UC-Study-003 | Phase 1 | 60 | Oral Small Molecule | Safety and tolerability | 12 | Completed |
| UC-Study-004 | Phase 3 | 500 | Integrin Antagonist | Clinical remission at week 10 | 52 | Ongoing |
| UC-Study-005 | Phase 2 | 150 | Microbiome Therapy | Reduction in Mayo score | 16 | Recruiting |
Patient participation in clinical trials is crucial for advancing research and improving treatment options for ulcerative colitis. By enrolling in these studies, patients contribute to the collective understanding of the disease and help identify effective therapies that may benefit future generations. Participation can also provide access to cutting-edge treatments that are not yet available through standard care pathways.
However, enrolling in a clinical trial is not a decision to be taken lightly. Patients must consider various factors, including eligibility criteria, potential risks, and the commitment required for follow-up visits and assessments. Healthcare providers play an essential role in guiding patients through this process by providing comprehensive information about ongoing trials and helping them weigh the potential benefits against any uncertainties involved.
Open communication between patients and their healthcare teams fosters an environment where informed decisions can be made regarding participation in clinical research.
Potential Risks and Benefits of Clinical Trials
While clinical trials offer numerous benefits, they also come with inherent risks that must be carefully considered by potential participants. One significant risk is the possibility of experiencing adverse effects from experimental treatments that may not yet be fully understood. Unlike established therapies with known safety profiles, new medications may carry unforeseen risks that could impact a patient’s health.
On the other hand, the benefits of participating in clinical trials can be substantial. Patients may gain access to innovative therapies that could lead to improved symptom control or even remission when conventional treatments have failed. Additionally, participants often receive close monitoring from healthcare professionals throughout the trial period, which can enhance their overall care experience.
Furthermore, contributing to research efforts can provide a sense of purpose and empowerment for patients who are navigating the challenges of living with ulcerative colitis.
Impact of Clinical Trial Findings on Ulcerative Colitis Management
The findings from clinical trials have a profound impact on the management of ulcerative colitis by shaping treatment guidelines and influencing clinical practice. As new therapies are validated through rigorous research, healthcare providers can incorporate these evidence-based approaches into their treatment plans, offering patients more effective options tailored to their specific needs. For instance, the introduction of biologic therapies has transformed the landscape of UC management by providing alternatives for patients who do not respond to traditional medications.
Clinical trial data demonstrating the efficacy and safety profiles of these agents have led to their inclusion in treatment algorithms endorsed by professional organizations such as the American College of Gastroenterology (ACG) and the European Crohn’s and Colitis Organisation (ECCO). As a result, patients now have access to a broader range of therapeutic options that can significantly improve their quality of life.
Future Directions in Ulcerative Colitis Research
Looking ahead, future directions in ulcerative colitis research hold great promise for enhancing our understanding of this complex disease and developing more effective treatments. Ongoing investigations into the microbiome’s role in UC pathogenesis are particularly intriguing, as emerging evidence suggests that gut bacteria may influence inflammation and disease activity. By exploring how alterations in microbial composition affect immune responses, researchers hope to identify novel therapeutic targets that could lead to more personalized treatment strategies.
Additionally, advancements in precision medicine are likely to play a crucial role in shaping future research efforts. By leveraging genetic profiling and biomarkers, clinicians may be able to predict which patients are most likely to respond to specific therapies, thereby optimizing treatment outcomes while minimizing unnecessary side effects. As technology continues to evolve, integrating artificial intelligence and machine learning into clinical research may further enhance our ability to analyze complex data sets and identify patterns that inform therapeutic decision-making.
In summary, ulcerative colitis remains a challenging condition requiring ongoing research and innovation in treatment approaches. The collaborative efforts between researchers, healthcare providers, and patients will be instrumental in driving progress toward more effective management strategies that ultimately improve the lives of those affected by this chronic disease.