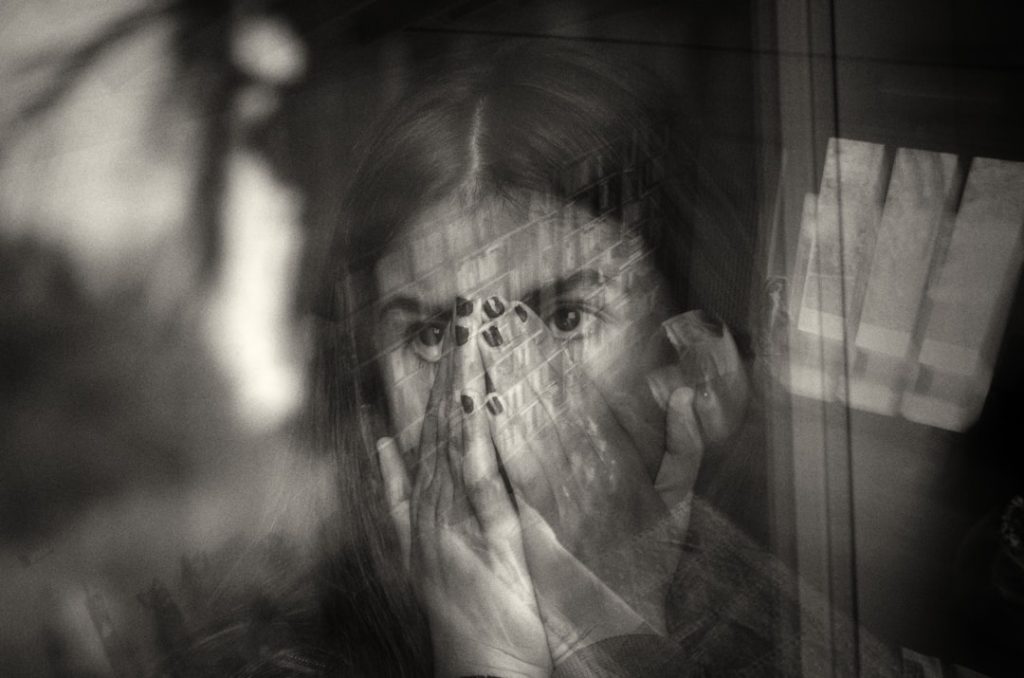
Schizophrenia is a complex and often misunderstood mental disorder that affects approximately 1% of the global population. Characterized by a range of symptoms, including delusions, hallucinations, disorganized thinking, and impaired functioning, schizophrenia can significantly disrupt an individual’s ability to lead a normal life. The onset of the disorder typically occurs in late adolescence or early adulthood, although it can manifest at any age.
The etiology of schizophrenia is multifaceted, involving a combination of genetic, neurobiological, and environmental factors. Research has shown that individuals with a family history of schizophrenia are at a higher risk of developing the disorder, suggesting a strong genetic component. The impact of schizophrenia extends beyond the individual, affecting families, communities, and healthcare systems.
Individuals with schizophrenia often face stigma and discrimination, which can exacerbate their condition and hinder their access to treatment. The disorder is not only debilitating but also costly, with significant economic implications due to healthcare expenses and lost productivity. Understanding schizophrenia requires a comprehensive approach that encompasses its biological underpinnings, psychological aspects, and social implications.
As research continues to evolve, it is crucial to explore innovative treatment options and improve the quality of life for those affected by this challenging condition.
Key Takeaways
- Schizophrenia treatment currently relies on antipsychotic medications and psychosocial interventions.
- Clinical trials are essential for developing and validating new therapies for schizophrenia.
- Emerging treatments show promise in improving symptoms and reducing side effects.
- Patient recruitment and ethical considerations are critical challenges in schizophrenia clinical research.
- Future research aims to personalize treatment and enhance long-term outcomes for patients.
Current Treatment Options for Schizophrenia
The treatment landscape for schizophrenia has evolved significantly over the past few decades, primarily focusing on pharmacological interventions and psychosocial therapies. Antipsychotic medications remain the cornerstone of treatment for schizophrenia, with two main categories: typical (first-generation) and atypical (second-generation) antipsychotics. Typical antipsychotics, such as haloperidol and chlorpromazine, primarily target dopamine receptors in the brain to alleviate positive symptoms like hallucinations and delusions.
However, they are often associated with severe side effects, including extrapyramidal symptoms and tardive dyskinesia. Atypical antipsychotics, including risperidone, olanzapine, and aripiprazole, have gained prominence due to their improved side effect profiles and efficacy in treating both positive and negative symptoms of schizophrenia. These medications work on multiple neurotransmitter systems, including serotonin and dopamine pathways, which may contribute to their broader therapeutic effects.
Despite their advantages, many patients experience challenges with medication adherence due to side effects or a lack of insight into their illness. Consequently, psychosocial interventions such as cognitive-behavioral therapy (CBT), family therapy, and supported employment programs are essential components of a comprehensive treatment plan. These therapies aim to enhance coping skills, improve social functioning, and provide support for both patients and their families.
Importance of Clinical Trials in Advancing Schizophrenia Treatment

Clinical trials play a pivotal role in advancing our understanding of schizophrenia and developing new treatment modalities. These research studies are designed to evaluate the safety and efficacy of new medications or therapeutic approaches before they can be approved for widespread use. By systematically investigating various aspects of treatment, clinical trials contribute to evidence-based practice in psychiatry.
They provide critical data that can inform clinical guidelines and help clinicians make informed decisions about patient care. Moreover, clinical trials offer hope to individuals with schizophrenia who may not respond adequately to existing treatments. Participation in these studies can provide access to cutting-edge therapies that are not yet available on the market.
For instance, recent trials have explored novel pharmacological agents targeting glutamate receptors or neuroinflammation pathways, which may offer new avenues for treatment. Additionally, clinical trials often incorporate innovative methodologies such as biomarker identification and neuroimaging techniques to better understand the underlying mechanisms of schizophrenia. This research not only enhances our knowledge of the disorder but also paves the way for personalized medicine approaches tailored to individual patient profiles.
Promising New Therapies and Medications in Development
The landscape of schizophrenia treatment is continually evolving, with numerous promising therapies and medications currently under investigation. One area of focus is the development of novel antipsychotic agents that target different neurotransmitter systems beyond dopamine. For example, compounds that modulate the glutamatergic system have garnered attention due to their potential to address both positive and negative symptoms of schizophrenia.
Drugs like ketamine and its derivatives have shown rapid antidepressant effects in treatment-resistant cases and are being studied for their efficacy in alleviating psychotic symptoms. Another exciting avenue of research involves the exploration of anti-inflammatory agents as adjunctive treatments for schizophrenia. Emerging evidence suggests that neuroinflammation may play a role in the pathophysiology of the disorder.
Consequently, medications that target inflammatory pathways could provide additional benefits for patients with schizophrenia who experience persistent symptoms despite conventional treatment. Furthermore, advancements in gene therapy and personalized medicine hold promise for tailoring interventions based on an individual’s genetic makeup or specific symptom profile. As these new therapies progress through clinical trials, they offer hope for improved outcomes and enhanced quality of life for individuals living with schizophrenia.
Patient Recruitment and Participation in Clinical Trials
| Metric | Value | Description |
|---|---|---|
| Number of Clinical Trials | 1,250+ | Total registered clinical trials related to schizophrenia |
| Phases Distribution | Phase 1: 15%, Phase 2: 40%, Phase 3: 35%, Phase 4: 10% | Percentage of trials in each clinical phase |
| Average Trial Duration | 18 months | Mean length of clinical trials for schizophrenia treatments |
| Common Interventions | Antipsychotics, Cognitive Behavioral Therapy, Digital Therapeutics | Types of interventions most frequently studied |
| Primary Outcome Measures | Symptom Reduction, Quality of Life, Functional Improvement | Key endpoints assessed in trials |
| Enrollment Size | 50 – 500 participants | Typical range of participant numbers per trial |
| Geographic Distribution | North America: 45%, Europe: 30%, Asia: 20%, Others: 5% | Regions where trials are predominantly conducted |
| Completion Rate | Approximately 70% | Percentage of trials that reach completion |
Recruiting participants for clinical trials in schizophrenia poses unique challenges due to the nature of the disorder itself. Many individuals with schizophrenia may have difficulty recognizing their illness or may be hesitant to participate in research due to stigma or fear of side effects from experimental treatments. Additionally, logistical barriers such as transportation issues or lack of support systems can further complicate recruitment efforts.
To address these challenges, researchers must employ innovative strategies to engage potential participants effectively. Outreach efforts that involve collaboration with community organizations, mental health clinics, and advocacy groups can help raise awareness about ongoing clinical trials and their potential benefits. Providing clear information about the trial process, including what participation entails and the safeguards in place to protect participants’ rights and well-being, is essential for building trust within this population.
Moreover, utilizing technology such as telehealth platforms can facilitate participation by allowing individuals to engage in assessments or follow-up appointments from the comfort of their homes. By addressing barriers to participation and fostering an inclusive environment, researchers can enhance recruitment efforts and ensure diverse representation in clinical trials.
Challenges and Considerations in Conducting Schizophrenia Clinical Trials

Conducting clinical trials in schizophrenia presents several challenges that researchers must navigate to ensure valid results and participant safety. One significant challenge is the heterogeneity of the disorder itself; schizophrenia manifests differently across individuals in terms of symptomatology, severity, and response to treatment. This variability can complicate the design of clinical trials and make it difficult to draw generalizable conclusions from study findings.
Additionally, maintaining participant retention throughout the trial is crucial for obtaining reliable data but can be particularly challenging in this population. Factors such as fluctuating symptoms, medication side effects, or personal circumstances may lead participants to withdraw from studies prematurely. Researchers must implement strategies to enhance retention rates, such as regular communication with participants, providing support services, or offering incentives for continued participation.
Furthermore, ensuring that trial protocols are sensitive to the needs of individuals with schizophrenia is essential for fostering a positive research experience.
Ethical and Regulatory Considerations in Schizophrenia Clinical Trials
Ethical considerations are paramount when conducting clinical trials involving individuals with schizophrenia due to their vulnerability and potential cognitive impairments. Researchers must prioritize informed consent processes that ensure participants fully understand the nature of the study, potential risks involved, and their right to withdraw at any time without penalty. Special attention should be given to assessing participants’ capacity to provide informed consent; when necessary, involving legal guardians or advocates may be appropriate.
Regulatory oversight also plays a critical role in safeguarding participants’ rights and well-being during clinical trials. Institutional Review Boards (IRBs) are responsible for reviewing study protocols to ensure ethical standards are met before research can commence. These boards evaluate factors such as risk-benefit ratios, recruitment methods, and data privacy protections.
Compliance with regulatory guidelines is essential not only for participant safety but also for maintaining public trust in the research process.
Future Directions in Schizophrenia Treatment Research
As our understanding of schizophrenia continues to evolve, future directions in treatment research will likely focus on several key areas aimed at improving outcomes for individuals living with this complex disorder. One promising avenue is the integration of biological markers into clinical practice to guide treatment decisions. Identifying specific biomarkers associated with treatment response could enable clinicians to tailor interventions more effectively based on individual patient profiles.
Additionally, there is growing interest in exploring the role of digital health technologies in managing schizophrenia. Mobile applications that facilitate symptom tracking or provide cognitive behavioral interventions may enhance self-management strategies for patients while also offering valuable data for researchers studying treatment efficacy. Furthermore, collaborative care models that involve multidisciplinary teams—including psychiatrists, psychologists, social workers, and peer support specialists—may provide more comprehensive support for individuals with schizophrenia.
In conclusion, ongoing research into innovative therapies and treatment approaches holds great promise for improving the lives of those affected by schizophrenia. By addressing existing challenges in clinical trial design and participant recruitment while adhering to ethical standards, researchers can continue to advance our understanding of this complex disorder and develop more effective interventions tailored to individual needs.