Advancing to the next stage in clinical research is a pivotal moment in the lifecycle of any medical or pharmaceutical innovation. This transition is not merely a procedural step; it represents a significant leap from theoretical frameworks and preclinical studies into the realm of human application. The importance of this advancement cannot be overstated, as it is during this phase that hypotheses are rigorously tested, and the potential for real-world impact becomes tangible.
The successful transition to clinical research can lead to groundbreaking therapies that address unmet medical needs, ultimately improving patient outcomes and enhancing the quality of life for countless individuals. Moreover, the advancement to clinical research is often a reflection of the cumulative efforts of multidisciplinary teams, including scientists, clinicians, and regulatory experts. Each member plays a crucial role in ensuring that the transition is not only successful but also efficient and compliant with established guidelines.
This collaborative effort underscores the importance of communication and coordination among various stakeholders, which is essential for navigating the complexities of clinical trials. The ability to move forward effectively can determine the trajectory of a project, influencing funding opportunities, partnerships, and the overall success of the therapeutic intervention being developed.
Key Takeaways
- Advancing to the next stage in clinical research is crucial for developing effective medical treatments.
- Successful transition depends on thorough preparation, clear objectives, and strong collaboration among stakeholders.
- Overcoming challenges requires addressing regulatory, ethical, and logistical hurdles proactively.
- Data analysis plays a vital role in validating results and guiding decision-making during clinical advancement.
- Ethical considerations and regulatory compliance are essential to ensure patient safety and research integrity.
Key Factors for Successful Transition to Clinical Research
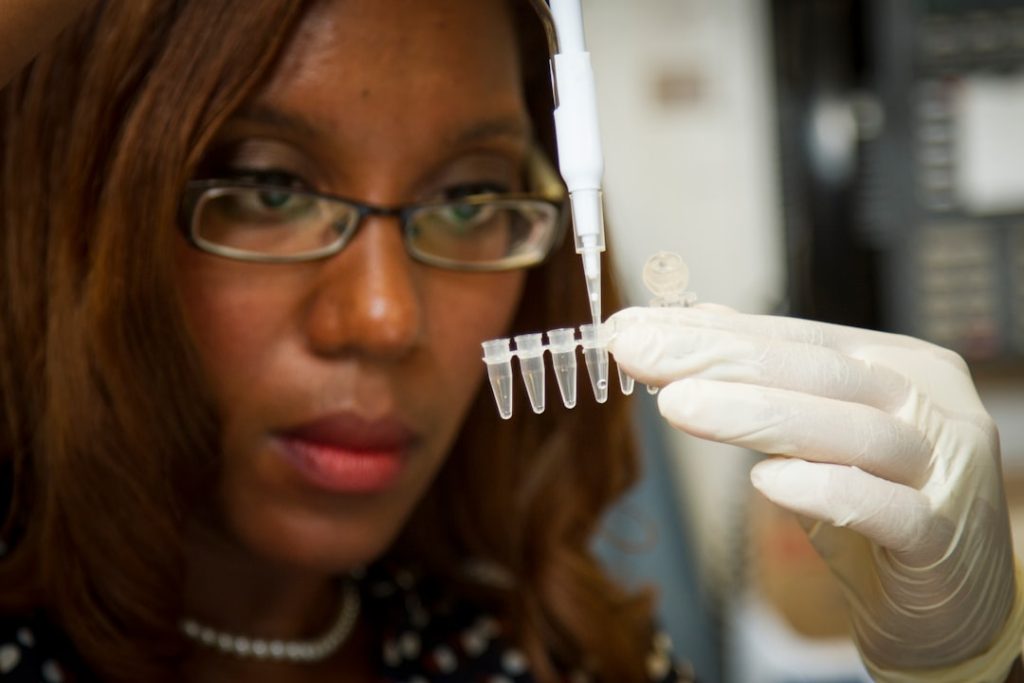
Several key factors contribute to a successful transition from preclinical studies to clinical research. One of the most critical elements is robust preclinical data that demonstrates safety and efficacy. Before any clinical trial can commence, researchers must provide compelling evidence that their intervention has the potential to benefit patients without posing undue risks.
This data often comes from a series of well-designed laboratory experiments and animal studies that assess pharmacodynamics, pharmacokinetics, and toxicology. The strength of this preclinical evidence can significantly influence regulatory approval and investor confidence. Another vital factor is the development of a comprehensive clinical trial protocol.
This document serves as a blueprint for the entire study, detailing objectives, methodologies, participant selection criteria, endpoints, and statistical analyses. A well-structured protocol not only guides researchers through the complexities of clinical trials but also ensures compliance with regulatory standards. Engaging with experienced clinical trial designers and biostatisticians during this phase can enhance the quality of the protocol, ultimately leading to more reliable results and smoother regulatory interactions.
Overcoming Challenges in Advancing to the Next Stage

The journey from preclinical research to clinical trials is fraught with challenges that can impede progress if not addressed proactively. One significant hurdle is securing funding for clinical studies, which often require substantial financial resources. Investors and funding agencies typically seek assurance that a project has a high likelihood of success before committing their resources.
Therefore, researchers must be adept at presenting their preclinical findings convincingly and demonstrating a clear path forward. This often involves crafting compelling narratives around the potential impact of their research while also addressing any perceived risks. Additionally, navigating regulatory requirements can pose another challenge.
Each country has its own set of regulations governing clinical trials, which can vary significantly in terms of complexity and stringency. Researchers must be well-versed in these regulations to avoid delays or rejections that could derail their projects. Engaging regulatory consultants or legal experts early in the process can help streamline this aspect, ensuring that all necessary documentation is prepared accurately and submitted on time.
By anticipating these challenges and developing strategies to mitigate them, researchers can enhance their chances of successfully advancing to clinical research.
The Role of Data Analysis in Advancing to Clinical Research
Data analysis plays a crucial role in advancing to clinical research, serving as both a tool for decision-making and a means of ensuring scientific rigor. In preclinical studies, data analysis helps researchers interpret complex biological information, identify trends, and draw meaningful conclusions about the safety and efficacy of their interventions. Advanced statistical methods can be employed to analyze data from experiments, allowing researchers to ascertain whether observed effects are statistically significant or merely due to chance.
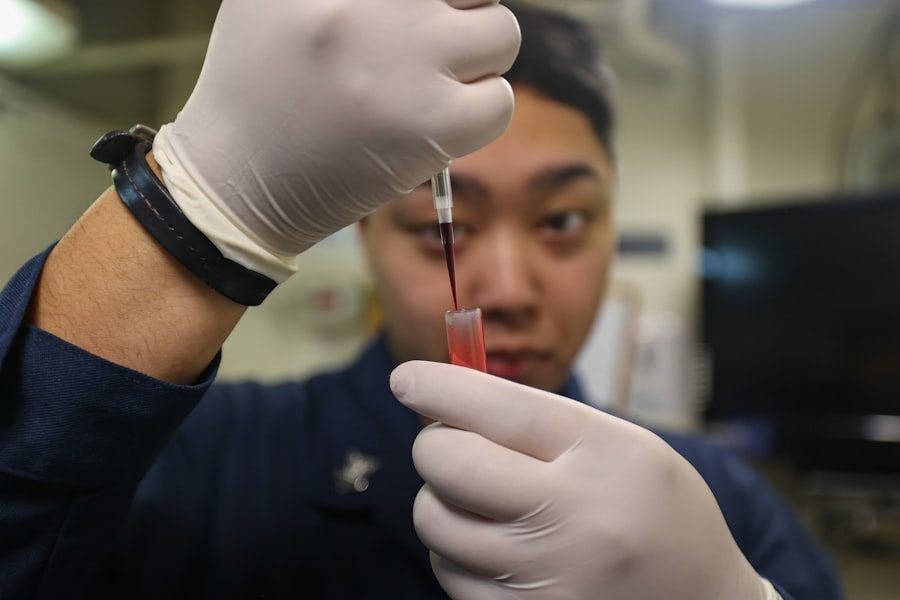
As researchers transition into clinical trials, data analysis becomes even more critical. Clinical trials generate vast amounts of data from diverse sources, including patient demographics, treatment responses, and adverse events. Effective data management systems are essential for organizing this information and facilitating real-time analysis.
Utilizing sophisticated statistical software can aid in monitoring trial progress and making informed decisions about modifications to study protocols or patient recruitment strategies. Furthermore, transparent reporting of data analysis results is vital for maintaining scientific integrity and fostering trust among stakeholders.
Ensuring Ethical Considerations in Advancing to the Next Stage
| Metric | Description | Typical Range/Value | Importance |
|---|---|---|---|
| Phase | Stage of clinical trial (Phase I, II, III, IV) | Phase II or III | Determines trial objectives and scale |
| Number of Participants | Number of subjects enrolled in the trial | 100 – 3,000 | Impacts statistical power and validity |
| Primary Endpoint | Main outcome measured to assess efficacy | e.g., Progression-Free Survival, Response Rate | Defines success criteria for the trial |
| Secondary Endpoints | Additional outcomes measured for safety or efficacy | e.g., Overall Survival, Quality of Life | Provides supplementary data on treatment impact |
| Duration | Length of the clinical trial | 6 months – 5 years | Affects time to market and resource allocation |
| Randomization | Method of assigning participants to treatment groups | Randomized Controlled Trial (RCT) | Reduces bias and improves reliability |
| Blinding | Whether participants and/or researchers are unaware of treatment assignments | Single-blind, Double-blind | Minimizes placebo effect and observer bias |
| Adverse Event Rate | Frequency of negative side effects reported | Varies by drug and phase; typically 5-30% | Critical for safety assessment |
| Dropout Rate | Percentage of participants who leave the trial early | 5-20% | Impacts data completeness and trial validity |
| Data Monitoring | Frequency and type of interim data reviews | Periodic (e.g., quarterly) by Data Monitoring Committee | Ensures participant safety and trial integrity |
Ethical considerations are paramount when advancing to clinical research, as they directly impact participant safety and the integrity of the research process. The principle of informed consent is foundational in this context; potential participants must be fully informed about the nature of the study, its risks and benefits, and their rights before agreeing to participate. Researchers have an ethical obligation to ensure that consent forms are clear and comprehensible, allowing individuals to make informed decisions about their involvement.
Additionally, ethical oversight is typically provided by Institutional Review Boards (IRBs) or Ethics Committees (ECs), which review study protocols to ensure that they meet ethical standards. These bodies assess factors such as risk-benefit ratios, participant recruitment strategies, and data privacy measures. Engaging with these committees early in the planning process can help identify potential ethical concerns and facilitate smoother approval processes.
By prioritizing ethical considerations throughout the research lifecycle, investigators can uphold the dignity and rights of participants while contributing valuable knowledge to the scientific community.
Collaborating with Regulatory Authorities in Advancing to Clinical Research
Collaboration with regulatory authorities is essential for successfully advancing to clinical research. These agencies play a critical role in ensuring that clinical trials are conducted safely and ethically while also protecting public health. Establishing open lines of communication with regulatory bodies can facilitate a smoother approval process and help researchers navigate complex regulatory landscapes.
Early engagement with agencies such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA) allows researchers to gain insights into regulatory expectations and requirements. Moreover, submitting Investigational New Drug (IND) applications or Clinical Trial Applications (CTAs) requires meticulous attention to detail and adherence to specific guidelines set forth by regulatory authorities.
Researchers must provide comprehensive documentation that includes preclinical data, proposed study designs, manufacturing processes, and plans for monitoring safety and efficacy during trials. By fostering collaborative relationships with regulators, researchers can receive valuable feedback that may enhance their study designs and increase the likelihood of successful approvals.
Leveraging Technology in Advancing to the Next Stage
The integration of technology into clinical research has revolutionized how studies are designed, conducted, and analyzed. From electronic health records (EHRs) to mobile health applications, technology enables researchers to collect real-time data from diverse sources efficiently. This capability not only enhances data accuracy but also allows for more dynamic patient engagement throughout the trial process.
For instance, wearable devices can monitor patient vitals continuously, providing invaluable insights into treatment responses outside traditional clinical settings. Furthermore, advancements in artificial intelligence (AI) and machine learning are transforming data analysis in clinical research. These technologies can identify patterns within large datasets that may not be apparent through conventional statistical methods.
By harnessing AI algorithms, researchers can optimize patient recruitment strategies by identifying suitable candidates based on historical data or even predict potential adverse events before they occur. The application of technology not only streamlines processes but also enhances the overall quality of clinical research outcomes.
Future Perspectives on Advancing to Clinical Research
Looking ahead, the landscape of clinical research is poised for significant transformation driven by ongoing advancements in science and technology. As personalized medicine continues to gain traction, future clinical trials may increasingly focus on tailoring interventions based on individual genetic profiles or biomarkers. This shift towards precision medicine will necessitate innovative trial designs that accommodate smaller patient populations while still yielding robust data on efficacy and safety.
Additionally, the rise of decentralized clinical trials (DCTs) presents new opportunities for advancing research beyond traditional settings. DCTs leverage digital tools to facilitate remote patient monitoring and data collection, allowing participants to engage in trials from their homes. This approach not only enhances patient convenience but also broadens access to diverse populations who may have previously faced barriers to participation due to geographical constraints or mobility issues.
In conclusion, as we navigate these evolving dynamics within clinical research, it is imperative for researchers to remain adaptable and forward-thinking. Embracing new methodologies while upholding ethical standards will be crucial in advancing innovative therapies that address pressing healthcare challenges in an increasingly complex world.