The Modified Medical Research Council (MMRC) dyspnea scale is a widely recognized and frequently employed tool for the subjective assessment of breathlessness. Originally developed by the Medical Research Council in the United Kingdom, it has been subsequently modified to enhance its utility in various clinical and research settings. This article provides an overview of the MMRC scale, its structure, application in medical research, and inherent limitations, offering a critical perspective for researchers and clinicians considering its use.
Dyspnea, commonly referred to as shortness of breath, is a subjective sensation characterized by an uncomfortable awareness of breathing. It is a prominent symptom in numerous cardiorespiratory diseases, significantly impacting a patient’s quality of life and functional capacity. Quantifying this subjective experience presents a unique challenge for medical professionals. Unlike objective measures such as blood pressure or heart rate, dyspnea lacks a direct physiological correlate that can be precisely measured. Instead, its assessment relies heavily on patient self-report, making tools like the MMRC scale invaluable.
Subjectivity in Symptom Assessment
The subjective nature of dyspnea means that different individuals may perceive and describe similar physiological perturbations in vastly different ways. Factors such as psychological state, cultural background, and previous experiences with illness can all influence an individual’s perception of breathlessness. Consequently, a standardized and universally understood language for describing dyspnea is crucial for both clinical practice and research. The MMRC scale attempts to provide such a framework by linking the sensation of breathlessness to specific activities of daily living.
The Need for Standardized Tools
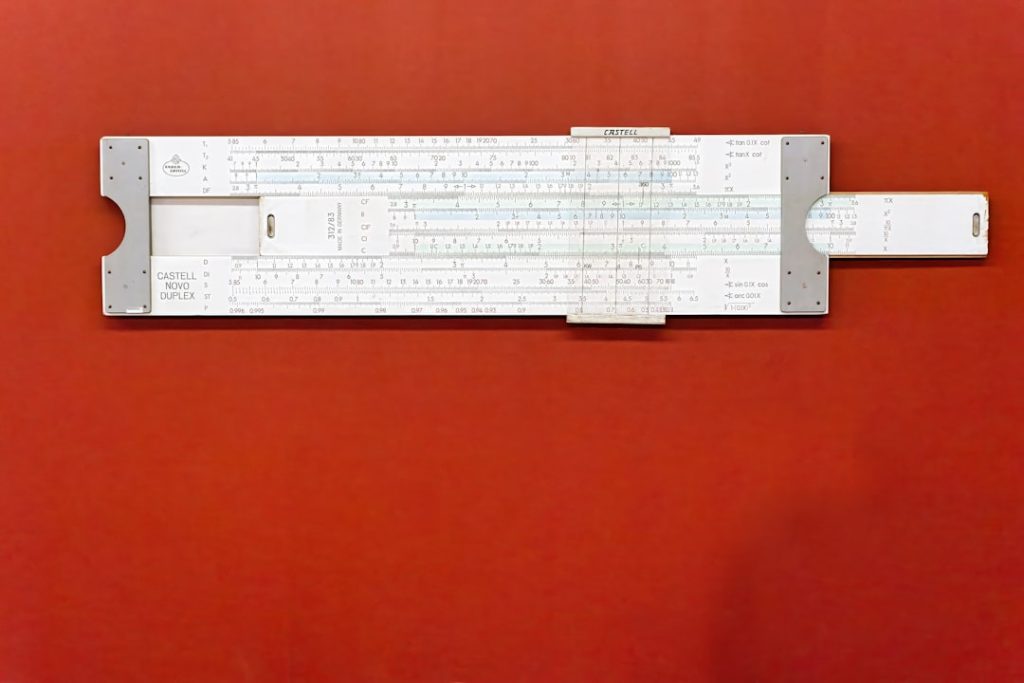
In medical research, consistency and comparability of data are paramount. Without standardized assessment tools, comparing the efficacy of different interventions or tracking disease progression across diverse patient populations becomes problematic. Imagine trying to compare the “heaviness” of various objects without a common unit of weight; the results would be chaotic and uninterpretable. The MMRC scale serves as a standardized “ruler” for dyspnea, allowing researchers to quantify and categorize the severity of breathlessness in a consistent manner.
Structure and Interpretation of the MMRC Scale
The MMRC scale is a simple, five-grade questionnaire that assesses the degree of breathlessness experienced by an individual during various levels of physical activity. Each grade corresponds to a specific level of impairment, progressing from no breathlessness to severe breathlessness that restricts daily activities.
Grade-by-Grade Breakdown
The MMRC scale typically presents as follows:
- Grade 0: Not troubled by breathlessness except on strenuous exercise. This grade represents a baseline, indicating no significant impact of breathlessness on routine activities. For instance, a person at this grade might comfortably walk up several flights of stairs or engage in vigorous sports without feeling unduly short of breath.
- Grade 1: Short of breath when hurrying on the level or walking up a slight hill. This signifies a mild level of dyspnea, where breathlessness becomes noticeable during slightly more demanding activities than routine walking. Think of it as the first sign of a “check engine” light coming on, not yet a breakdown, but an indication of something needing attention during increased demand.
- Grade 2: Walks slower than most people on the level because of breathlessness, or has to stop for breath when walking on the level at own pace. At this stage, dyspnea begins to impact an individual’s normal walking pace and may necessitate pauses. This grade represents a more significant impairment, where the individual’s pace is dictated by their breathlessness, not their desire or ability.
- Grade 3: Stops for breath after walking about 100 meters or after a few minutes on the level. This marks a considerable increase in breathlessness severity, significantly limiting walking distance and endurance. The “fuel tank” for walking activities is starting to run critically low, requiring frequent stops for replenishment.
- Grade 4: Too breathless to leave the house, or breathless when dressing or undressing. This is the most severe grade, indicating profound dyspnea that impacts fundamental activities of daily living, often confining the individual to their home. Breathlessness becomes a constant companion, intruding even on simple self-care tasks.
Scoring and Application
The MMRC scale yields a single numerical score ranging from 0 to 4, with higher scores indicating greater severity of dyspnea. This ordinal scale allows for straightforward categorization of patients based on their self-reported breathlessness. The simplicity of its scoring is a key advantage, making it easy to administer and interpret in various clinical and research settings. No complex calculations or specialized equipment are required, making it a low-barrier tool for assessment.
Advantages in Medical Research

The MMRC dyspnea scale boasts several advantages that contribute to its widespread adoption in medical research. Its simplicity, cost-effectiveness, and established validity make it a cornerstone in the assessment of breathlessness in numerous disease states.
Simplicity and Ease of Administration
One of the most compelling advantages of the MMRC scale is its straightforward nature. It consists of only five short statements, requiring minimal time for patients to understand and respond. This brevity reduces patient burden, a crucial consideration in research studies where participants may already be contending with multiple assessments. For researchers, this translates to efficient data collection and reduced administrative overhead. The clarity of the statements also minimizes ambiguity, facilitating consistent responses across different individuals.
Cost-Effectiveness
The MMRC scale requires no specialized equipment, licensing fees, or extensive training. It can be administered verbally or as a printed questionnaire, making it an exceptionally cost-effective tool. This aspect is particularly important for large-scale epidemiological studies or research conducted in resource-limited settings where expensive diagnostic tools may not be available. Its accessibility makes it a democratic tool for dyspnea assessment.
Established Validity and Reliability
Numerous studies have validated the MMRC scale against other measures of dyspnea and functional capacity, demonstrating its utility and accuracy. It has been shown to correlate well with objective measures such as forced expiratory volume in one second (FEV1), six-minute walk distance (6MWD), and health-related quality of life questionnaires. This robust evidence base provides researchers with confidence in the scale’s ability to accurately reflect a patient’s breathlessness burden. The reliability of the MMRC scale, meaning its consistency in yielding similar results over time when the underlying condition has not changed, has also been well-demonstrated, making it suitable for tracking changes in dyspnea severity over the course of an intervention or disease progression.
Utility Across Diverse Disease States
While initially developed for chronic obstructive pulmonary disease (COPD), the MMRC scale has proven valuable in assessing dyspnea across a wide spectrum of cardiorespiratory and other conditions. These include:
- Asthma: To gauge the impact of airway inflammation and bronchoconstriction on daily activities.
- Interstitial Lung Disease: To track the progression of pulmonary fibrosis and its effect on exercise tolerance.
- Heart Failure: To quantify the severity of cardiac dyspnea and its response to treatment.
- Pulmonary Hypertension: To assess the functional limitations imposed by elevated pulmonary artery pressures.
- Obesity: To understand the contribution of excess weight to breathlessness.
- Post-COVID-19 Condition: To evaluate persistent dyspnea in individuals recovering from COVID-19.
This versatility makes the MMRC scale a valuable tool for researchers studying various patient populations, enabling comparisons and insights across different disease categories. It serves as a common language, bridging the gaps between specialties.
Limitations and Considerations for Research

Despite its strengths, the MMRC scale is not without limitations. Researchers must be cognizant of these inherent drawbacks to avoid misinterpretation of data and to ensure appropriate application of the scale.
Subjectivity and Inter-individual Variability
As a self-reported measure, the MMRC scale is inherently subjective. An individual’s interpretation of terms like “hurrying” or “slight hill” can vary significantly based on their physical condition, age, and previous experiences. For instance, what constitutes “strenuous exercise” for a sedentary individual might be considered mild activity for an athlete. This variability, much like trying to measure temperature with thermometers calibrated to different scales, can introduce noise into research data and potentially obscure subtle but clinically relevant changes. Researchers should acknowledge this subjectivity in their study design and interpretation.
Ceiling Effect
The MMRC scale has a limited range (0-4), which can lead to a “ceiling effect” in patients with severe dyspnea. Individuals who consistently score a 4, indicating severe breathlessness that confines them to the house or makes dressing difficult, may not be able to demonstrate further deterioration in their symptoms using this scale, even if their condition worsens. Imagine a measuring stick that only goes up to four feet; you can’t accurately measure anything taller. This limitation means the MMRC scale may not be sensitive enough to detect improvements or deteriorations at the most extreme end of the dyspnea spectrum.
Lack of Responsiveness to Subtle Changes
While effective in categorizing overall dyspnea severity, the MMRC scale may not be sufficiently responsive to detect subtle, clinically meaningful changes in breathlessness over short periods or in response to interventions that elicit small improvements. For example, a small but real improvement in lung function might not translate to a change in MMRC grade if the patient is still within the same activity category. This lack of granularity can be a drawback in intervention trials aiming to demonstrate fine-tuned effects. More sensitive, continuous scales, such as visual analogue scales (VAS) or Borg scales, may be more appropriate for detecting such nuanced changes in specific research contexts.
Cultural and Linguistic Considerations
The MMRC scale was developed in an English-speaking, Western context. The descriptions of activities may not translate equivalently across different cultures and languages. For example, “walking up a slight hill” might be a common activity in some regions but less so in others, affecting a patient’s ability to relate to the description. Careful translation and cultural adaptation are necessary when using the MMRC scale in diverse populations to ensure its validity and avoid misinterpretation. Just as a plant needs the right soil to flourish, a questionnaire needs the right cultural context to yield accurate data.
Focus on Physical Activity Limitation
The MMRC scale primarily quantifies dyspnea in relation to physical activity. It does not explicitly capture other dimensions of breathlessness, such as its emotional impact, the fear of breathlessness, or the sensation quality (e.g., “tightness,” “air hunger”). While closely related to physical limitation, these other facets contribute significantly to a patient’s overall burden of dyspnea. For a comprehensive understanding of dyspnea, researchers may need to supplement the MMRC scale with other instruments that explore these additional dimensions. The MMRC acts as a snapshot of physical limitation, but a complete album requires more pictures.
Integrating MMRC into Research Design
| MMRC Grade | Description | Dyspnea Severity | Impact on Daily Activities |
|---|---|---|---|
| 0 | Not troubled by breathlessness except with strenuous exercise | None | Normal activity without breathlessness |
| 1 | Short of breath when hurrying on level ground or walking up a slight hill | Mild | Minimal limitation in daily activities |
| 2 | Walks slower than people of the same age on level ground because of breathlessness or has to stop for breath when walking at own pace | Moderate | Some limitation in walking and daily tasks |
| 3 | Stops for breath after walking about 100 meters or after a few minutes on level ground | Severe | Significant limitation in mobility and daily activities |
| 4 | Too breathless to leave the house or breathless when dressing or undressing | Very Severe | Unable to perform most daily activities independently |
When designing research studies involving dyspnea assessment, careful consideration of the MMRC scale’s strengths and limitations is crucial for valid and meaningful results. Researchers should strive to integrate the scale effectively within a broader methodological framework.
Pre-screening and Baseline Assessment
The MMRC scale is highly effective as a pre-screening tool to identify patients with significant dyspnea who may be eligible for specific research studies. It can also serve as a robust baseline measure to characterize the initial severity of breathlessness in a study cohort. For instance, a study investigating a new treatment for COPD might define eligibility criteria based on an MMRC score of 2 or higher, ensuring that enrolled patients experience a clinically relevant level of dyspnea. This initial categorization helps to standardize the study population.
Outcome Measure in Intervention Studies
The MMRC scale can be used as a primary or secondary outcome measure in clinical trials assessing the efficacy of interventions. A statistically significant reduction in MMRC score following an intervention would indicate an improvement in dyspnea severity. However, researchers should consider the scale’s responsiveness, particularly for interventions expected to yield small or incremental changes. It might be more suitable for interventions targeting substantial improvements in functional capacity. When using the MMRC as an outcome measure, specifying a minimum clinically important difference (MCID) – the smallest change in score that patients perceive as beneficial – is essential for interpreting the clinical significance of observed changes.
Stratification and Subgroup Analysis
Due to its ability to broadly categorize dyspnea severity, the MMRC scale can be used to stratify patient cohorts for subgroup analysis. For example, researchers might analyze the response to an intervention separately for patients with mild (MMRC 0-1) versus moderate-to-severe (MMRC 2-4) dyspnea. This segmentation can reveal differential treatment effects or identify patient characteristics that influence treatment response. It allows for a more nuanced understanding of the disease and intervention effects.
Complementary Measures
To overcome the MMRC scale’s limitations, particularly its subjectivity and limited scope, researchers are encouraged to use it in conjunction with complementary measures. These might include:
- Objective Physiological Measures: Such as FEV1, forced vital capacity (FVC), oxygen saturation, and resting/exercise heart rate. These provide physiological context to the subjective report.
- Exercise Capacity Tests: Like the 6MWD or cardiopulmonary exercise testing (CPET), which offer objective measures of functional limitation.
- Other Dyspnea Scales: Such as the Borg scale, visual analogue scales (VAS), or the UCSD Shortness of Breath Questionnaire, which may capture different dimensions of breathlessness or offer greater sensitivity to change.
- Health-Related Quality of Life Questionnaires: Such as the St. George’s Respiratory Questionnaire (SGRQ) or the COPD Assessment Test (CAT), which provide a broader perspective on the impact of dyspnea on a patient’s life.
By triangulating data from multiple sources, researchers can build a more comprehensive and robust understanding of dyspnea in their study population, mitigating the individual weaknesses of any single assessment tool. The MMRC scale, when integrated thoughtfully into a comprehensive research battery, serves as a valuable and efficient instrument for assessing the impact of breathlessness on daily living.