Central laboratories, often referred to as central labs, are specialized facilities providing standardized analytical and logistical services for clinical trials. Their role is to ensure the consistent collection, processing, analysis, and reporting of laboratory data across multiple clinical study sites. This standardization is critical for the integrity and comparability of data, which directly impacts the validity and reliability of clinical trial results.
Central laboratories function as a centralized hub for all laboratory-related activities within a clinical trial. Imagine a sprawling clinical trial with numerous investigative sites spread across different countries. Each site might have its own local laboratory, but variations in equipment, methodologies, reagents, and personnel training could lead to inconsistent results. This inconsistency, if unchecked, would make it impossible to draw meaningful conclusions about the efficacy and safety of an investigational product.
Central labs mitigate this risk by acting as a single point of reference for all biological samples. They establish and adhere to stringent protocols for every stage of the sample lifecycle, from collection to analysis and archival. This consistency is paramount for regulatory compliance and ultimately for patient safety.
Standardization of Procedures
Standardization is the cornerstone of central laboratory operations. This encompasses everything from the design of sample collection kits to the analytical platforms used.
- Sample Collection Kits: Central labs design and distribute standardized sample collection kits to all participating sites. These kits include precise instructions, appropriate tubes (e.g., EDTA, serum separator), labels, and materials for temperature-controlled shipping. This ensures consistent pre-analytical conditions, which are known to impact assay results.
- Analytical Platforms and Reagents: All analyses are performed on identical, validated instruments using the same lot numbers of reagents. This eliminates variability introduced by different equipment models or reagent batches.
- Method Validation: All analytical methods used by the central lab undergo rigorous validation processes, demonstrating their accuracy, precision, linearity, limits of detection, and quantification according to regulatory guidelines (e.g., CLIA, CAP, GCLP).
Data Management and Reporting
Central labs are responsible for robust data management practices, ensuring the accuracy, integrity, and security of all laboratory data.
- Data Integration: Laboratory data are integrated into the overall clinical trial database. This often involves secure electronic data transfer with audit trails.
- Quality Control and Assurance: Extensive quality control (QC) programs are implemented, including daily instrument calibration, internal QC samples, and participation in external proficiency testing programs. Quality assurance (QA) departments regularly audit procedures and documentation.
- Reporting: Standardized reports are generated for investigators, sponsors, and regulatory authorities. These reports provide clear, concise, and accurate data summaries, often including trend analysis and graphical representations.
Key Services Offered by Central Laboratories
Central labs offer a diverse range of services, tailored to the specific needs of each clinical trial. These services span various analytical disciplines.
Clinical Chemistry and Hematology
These are fundamental tests providing information on organ function, metabolic status, and blood cell counts.
- Comprehensive Metabolic Panels (CMPs): Assess liver and kidney function, electrolyte balance, and glucose levels.
- Complete Blood Counts (CBCs): Provide information on red blood cells, white blood cells, and platelets, crucial for monitoring potential adverse effects on hematopoiesis.
- Cardiac Biomarkers: Detect myocardial injury, important in trials involving cardiovascular safety.
Urinalysis and Coagulation
Urinalysis provides insights into renal function and urinary tract health, while coagulation assays are critical for assessing bleeding risk or the effect of anticoagulant therapies.
- Routine Urinalysis: Physical, chemical, and microscopic examination of urine.
- Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT): Measure the time it takes for blood to clot, essential for monitoring anticoagulant therapy.
- D-dimer: A marker for fibrin degradation products, indicating fibrinolysis and often used in diagnosing thrombotic conditions.
Immunochemistry and Microbiology
These departments specialize in assays involving antibodies, antigens, and the detection of microorganisms.
- Immunoassays (ELISA, CLIA): Measure levels of proteins, hormones, biomarkers, and infectious disease markers.
- Viral Load and Genotyping: Critical for trials involving antiviral agents, assessing viral replication and resistance.
- Antimicrobial Susceptibility Testing: Determines the effectiveness of antibiotics against specific bacterial strains.
Molecular Diagnostics and Genetics
With advancements in molecular biology, these services are increasingly crucial for personalized medicine and targeted therapies.
- Pharmacogenomics: Analyzes genetic variations that influence an individual’s response to drugs, helping to predict efficacy and potential adverse drug reactions.
- Biomarker Discovery and Validation: Identification and verification of molecular indicators that can predict disease presence, progression, or response to treatment.
- Next-Generation Sequencing (NGS): Enables comprehensive genetic profiling, including detection of mutations, copy number variations, and gene expression changes.
Regulatory Compliance and Quality Assurance
Central laboratories operate under a strict regulatory framework to ensure the reliability and integrity of their data. Adherence to these regulations is not optional; it is a fundamental requirement for the acceptance of clinical trial data by regulatory bodies worldwide.
Good Clinical Laboratory Practice (GCLP)
GCLP principles provide a framework for the organization, processing, and reporting of clinical laboratory studies. While not a standalone regulation, GCLP draws upon elements of Good Clinical Practice (GCP) and Good Laboratory Practice (GLP) to specifically address the unique requirements of laboratories supporting clinical trials.
- Personnel Qualifications: Staff must be appropriately trained, qualified, and demonstrate proficiency in their assigned tasks. Continuous education and competency assessments are essential.
- Equipment Calibration and Maintenance: All instruments must be regularly calibrated, maintained, and documented according to manufacturer specifications and internal standard operating procedures (SOPs).
- Documentation: Every step of the process, from sample receipt to data reporting, must be meticulously documented. This includes SOPs, raw data, calibration records, QC results, and audit trails.
Accreditation and Certification
Accreditation by recognized bodies provides external validation of a central lab’s quality systems and technical competence.
- CAP (College of American Pathologists) Accreditation: A globally recognized program ensuring high standards of laboratory quality, proficiency testing, and personnel qualification.
- CLIA (Clinical Laboratory Improvement Amendments) Certification: In the United States, CLIA regulations establish quality standards for all laboratory testing to ensure the accuracy, reliability, and timeliness of patient test results.
- ISO 15189 Accreditation: An international standard specifying requirements for quality and competence in medical laboratories, including clinical trials.
The Logistics of Clinical Trial Samples

Managing biological samples across a global clinical trial is a complex logistical undertaking. Central labs act as the orchestrators of this intricate process. Picture a vast network of highways and air routes, all leading to a central processing plant.
Sample Collection and Kit Manufacturing
The journey begins at the investigative sites with custom-designed sample collection kits. These kits are meticulously prepared and distributed by the central lab.
- Kit Design: Kits are customized for each study, containing specific tubes, labels, instructions, and materials for safe and compliant shipping.
- Logistics and Distribution: Central labs manage the inventory, assembly, and distribution of these kits to numerous sites, often across different continents, ensuring timely delivery.
Transportation and Shipping
Maintaining sample integrity during transit is critical. This often involves temperature-controlled shipping and adherence to international regulations.
- Temperature Control: Samples may require storage and shipping at ambient, refrigerated, or frozen temperatures (e.g., -20°C, -70°C, or dry ice). Specialized packaging and temperature monitoring devices are used.
- International Regulations: Compliance with IATA (International Air Transport Association) regulations for shipping diagnostic and infectious substances is mandatory. This includes proper labeling, documentation, and packaging.
- Chain of Custody: A robust chain of custody system tracks each sample from the moment it is collected until its final disposition, providing an unbroken record of its handling.
Sample Receipt and Processing
Upon arrival at the central lab, samples undergo a series of critical steps.
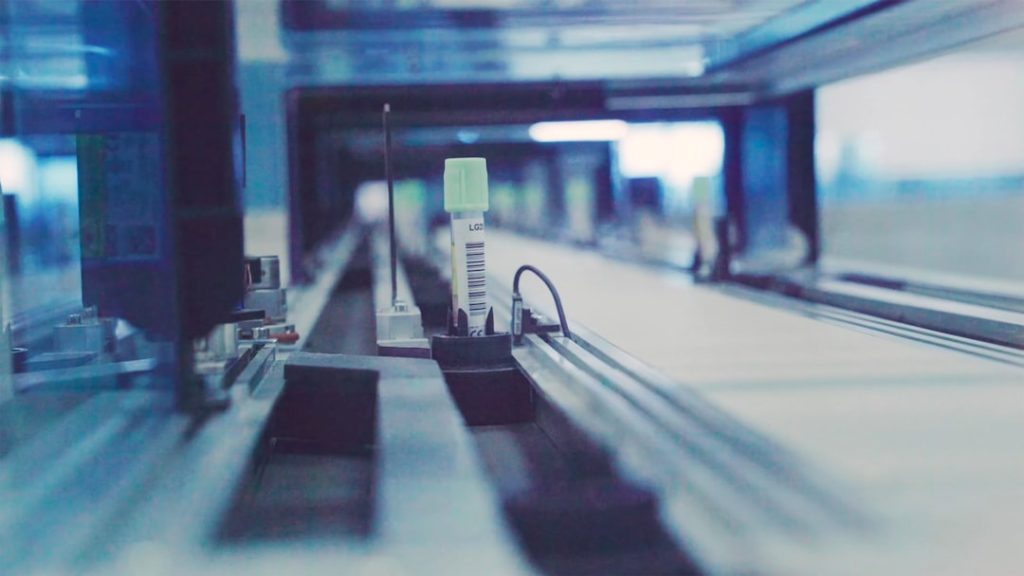
- Accessioning: Each sample is uniquely identified, logged into the laboratory information management system (LIMS), and assigned a barcode for tracking.
- Primary Processing: This includes centrifugation, aliquoting, and preparation for storage or immediate analysis. Strict adherence to SOPs minimizes pre-analytical errors.
- Archiving: Remaining sample aliquots are often archived for potential future analysis or regulatory requirements, typically stored at ultra-low temperatures in secure facilities with continuous temperature monitoring.
Advancements and Future Trends in Central Laboratory Services
| Metric | Description | Typical Range/Value | Importance in Clinical Trials |
|---|---|---|---|
| Turnaround Time (TAT) | Time taken from sample receipt to result delivery | 24-72 hours | Critical for timely decision-making and patient safety |
| Sample Volume Capacity | Number of samples processed per day | 500-10,000 samples/day | Ensures scalability for large multi-center trials |
| Test Menu | Range of assays and tests offered (e.g., hematology, biochemistry, immunology) | 50-200+ tests | Supports diverse clinical trial protocols and endpoints |
| Regulatory Compliance | Certifications and standards met (e.g., CLIA, CAP, GCP) | Mandatory for clinical trial labs | Ensures data integrity and regulatory acceptance |
| Data Management Systems | Use of LIMS and electronic data capture systems | Integrated, validated systems | Facilitates accurate data tracking and reporting |
| Geographic Coverage | Number of countries or regions served | Global or regional (5-50+ countries) | Supports multi-national clinical trials |
| Quality Control Measures | Internal and external QC programs participation | Continuous monitoring and proficiency testing | Maintains accuracy and reliability of lab results |
| Sample Storage Capability | Ability to store samples at required conditions (e.g., -80°C) | Short and long-term storage options | Enables retesting and biomarker discovery |
The central laboratory landscape is continuously evolving, driven by technological innovations, regulatory shifts, and the increasing complexity of clinical trials.
Automation and Robotics
Automation is transforming central lab operations, improving efficiency, reducing human error, and increasing throughput.
- Automated Sample Handling Systems: Robots perform tasks such as uncapping, aliquoting, and barcoding, minimizing manual intervention.
- High-Throughput Analyzers: Modern analytical platforms can process hundreds or thousands of samples per hour, accelerating turnaround times.
- Laboratory Information Management Systems (LIMS): Sophisticated LIMS platforms integrate all lab operations, from sample tracking to data reporting, enhancing data integrity and accessibility.
Biomarker Development and Precision Medicine
The focus on specific biomarkers is central to the development of precision medicine, which aims to tailor treatments to individual patients based on their genetic and molecular profiles.
- Companion Diagnostics: Central labs often play a critical role in developing and validating companion diagnostics, which are tests that identify patients who are most likely to benefit from a particular therapy.
- Liquid Biopsies: Analysis of circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and other biomarkers from blood samples offers a less invasive alternative to tissue biopsies, enabling real-time monitoring of disease progression and treatment response.
- Multi-Omics Integration: The integration of data from genomics, proteomics, metabolomics, and other “omics” technologies provides a holistic view of biological systems, driving deeper insights into disease mechanisms and therapeutic interventions.
Global Harmonization and Regulatory Challenges
Operating globally presents challenges in harmonizing diverse regulatory requirements and ensuring consistent quality across different regions.
- International Standards: Adherence to international standards like ISO 15189 and GCLP is becoming increasingly important for global clinical trials.
- Data Privacy (e.g., GDPR, HIPAA): Central labs must navigate complex data privacy regulations, ensuring the protection of patient information across borders.
- Emerging Technologies Regulation: As new analytical technologies emerge, regulatory bodies adapt their guidelines, requiring central labs to stay abreast of these changes and demonstrate compliance.
Central laboratories are indispensable partners in drug development. They are the silent engines ensuring the robust, reliable, and reproducible generation of laboratory data, which is foundational for demonstrating the safety and efficacy of new medical therapies. Without their rigorous standardization and quality control, the clinical trial landscape would be fragmented, and the journey of bringing crucial treatments to patients would be significantly impeded. You, as a stakeholder in this process, benefit directly from their unwavering commitment to scientific integrity.