Certified clinical research serves as a cornerstone of modern medicine. It provides a structured framework for investigating new treatments, diagnostics, and preventative measures, moving them from theoretical concepts to practical applications. This rigorous process is essential for ensuring the safety and efficacy of medical interventions before they are widely adopted, acting as a filter for innovation. Through a systematic approach, certified clinical research aims to generate reliable evidence that informs healthcare decisions and improves patient outcomes globally.
Evidence-based medicine (EBM) is a medical practice approach that emphasizes the use of current best evidence in making decisions about the care of individual patients. At its core, EBM relies heavily on data generated through clinical research. Certified clinical research ensures that this data is not only available but also trustworthy and robust.
Defining Certified Clinical Research
Certified clinical research refers to clinical trials and studies conducted under ethical guidelines and regulatory oversight, often involving a formal certification process for either the investigators, the research sites, or the overall quality management system. This certification signifies adherence to Good Clinical Practice (GCP) guidelines, a set of international ethical and scientific quality standards for designing, conducting, recording, and reporting trials that involve human participants. The aim is to protect the rights, safety, and well-being of subjects and to ensure the credibility of study results. Think of GCP as the blueprint for building a reliable edifice of medical knowledge; without it, the structure might crumble.
The Role of Certification Bodies
Various organizations provide certification in clinical research, ranging from professional associations offering individual certifications for clinical research professionals (e.g., Certified Clinical Research Coordinator, Certified Clinical Research Associate) to regulatory bodies assessing the compliance of research sites and practices. These certifications serve multiple purposes: they validate expertise, standardize practices, and build public trust. For instance, a certified research site has demonstrated its capacity to conduct studies ethically and efficiently, providing assurance to sponsors and regulatory agencies alike.
Methodologies and Phases of Clinical Research
The journey of a new medical intervention, from conception to widespread use, is meticulously orchestrated through distinct phases of clinical research. These phases are designed to systematically gather information about safety, dosage, efficacy, and long-term effects.
Pre-Clinical Research: The Starting Point
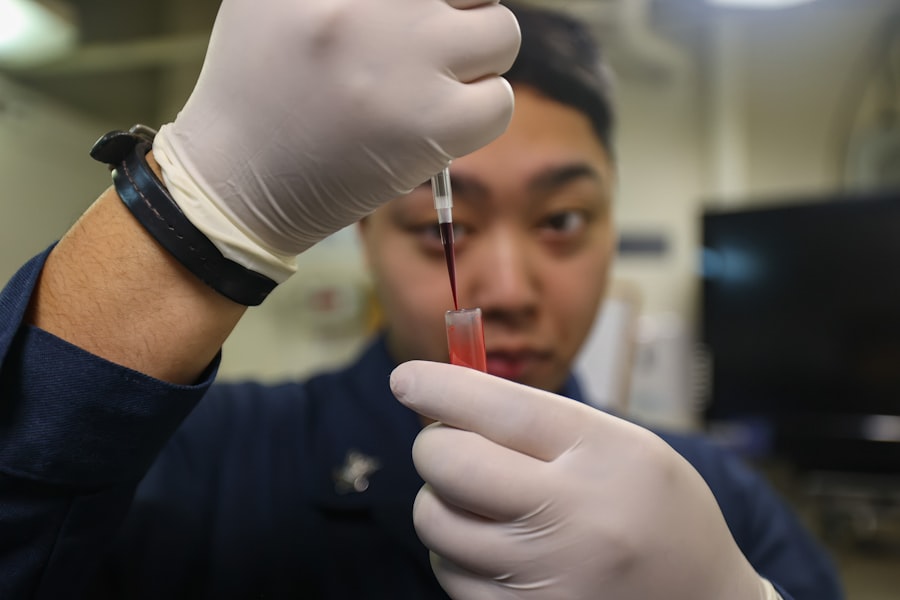
Before any intervention can be tested in humans, extensive pre-clinical research is conducted. This phase typically involves in vitro (test tube) studies and in vivo (animal model) studies. The primary goals are to assess the potential toxicity, biological activity, and preliminary efficacy of a new drug or device. This is the stage where the rough sketches are drawn and early models are built, identifying promising candidates while weeding out those with significant risks or no observable benefit. It’s a critical filter, preventing potentially harmful substances from entering human trials.
Phase 1 Trials: Prioritizing Safety
Phase 1 trials are the first human trials of a new intervention. They typically involve a small group of healthy volunteers or, in some cases, patients with the condition being studied, particularly in oncology. The primary objective is to evaluate the safety of the intervention, determine a safe dosage range, and identify common side effects. Efficacy is a secondary consideration. These trials are akin to test-driving a new vehicle at low speeds in a controlled environment – the focus is on discerning fundamental operational safety.
Phase 2 Trials: Exploring Efficacy and Further Safety
Moving beyond basic safety, Phase 2 trials involve a larger group of patients who have the condition that the intervention is intended to treat. The main goals are to evaluate the efficacy of the intervention and to continue assessing its safety. Researchers also collect data on optimal dosage and administration methods. If Phase 1 is the test drive, Phase 2 is taking the vehicle on moderate roads, observing its performance and handling in more realistic conditions.
Phase 3 Trials: Confirming Efficacy and Monitoring Adverse Events
Phase 3 trials are large-scale, multi-center studies involving hundreds to thousands of patients. They compare the new intervention to existing standard treatments or a placebo to confirm its efficacy, monitor adverse events, and collect information that will allow the intervention to be used safely. Positive results from Phase 3 trials are often a prerequisite for regulatory approval (e.g., by the FDA in the United States or EMA in Europe). This phase is the ultimate road test, subjecting the intervention to diverse conditions and a large population to ensure it performs as expected for a wide range of users. It’s here that the intervention truly proves its mettle.
Phase 4 Trials: Post-Market Surveillance
Even after an intervention receives regulatory approval, the research does not cease. Phase 4 trials, also known as post-market surveillance studies, continue to monitor its safety and efficacy in the general population over extended periods. These studies identify rare or long-term side effects that may not have been apparent in earlier trials due to smaller sample sizes or shorter follow-up durations. This is the ongoing maintenance check, ensuring the vehicle continues to perform safely and efficiently long after it leaves the showroom.
Ethical Considerations in Clinical Research

The ethical framework underpinning certified clinical research is paramount. Given that studies involve human participants, robust safeguards are essential to protect their rights, well-being, and autonomy.
Informed Consent: The Cornerstone of Participation
Informed consent is a voluntary agreement to participate in research after being fully apprised of all relevant information about the study. This includes the study’s purpose, procedures, potential risks and benefits, alternatives to participation, and the right to withdraw at any time without penalty. Obtaining truly informed consent is not a mere formality; it is a dynamic process of communication and understanding, ensuring that participants are partners, not just subjects. It’s like clearly outlining the terms of a journey before embarking, ensuring everyone understands the destination, the route, and any potential bumps along the way.
Institutional Review Boards (IRBs): Guardians of Ethics
Institutional Review Boards (IRBs), or Ethics Committees, are independent administrative bodies established to protect the rights and welfare of human research subjects. They review research protocols to ensure they meet ethical standards, assess the balance of risks and benefits, and monitor the informed consent process. Their approval is mandatory for any research involving humans. IRBs act as critical gatekeepers, ensuring that compassion and caution are woven into the very fabric of research design.
Data Confidentiality and Privacy
Protecting the confidentiality and privacy of participants’ health information is a fundamental ethical obligation. Researchers must implement stringent measures to safeguard sensitive data, adhering to regulations such as HIPAA (Health Insurance Portability and Accountability Act) in the US or GDPR (General Data Protection Regulation) in Europe. The trust placed in researchers by participants is a precious commodity; its breach can have far-reaching negative consequences for individuals and for public confidence in research.
Regulatory Landscape and Compliance
The conduct of certified clinical research is heavily regulated to ensure both ethical standards and the scientific validity of the findings. Adherence to these regulations is not optional; it is a mandate.
Good Clinical Practice (GCP)
As mentioned, GCP is an international ethical and scientific quality standard. It provides a unified standard for the design, conduct, performance, monitoring, auditing, recording, analyses, and reporting of clinical trials. Compliance with GCP ensures that the data and reported results are credible and accurate, and that the rights, integrity, and confidentiality of trial subjects are protected. Think of GCP as the universal language of clinical research, enabling effective communication and consistent quality across borders.
Regulatory Bodies (e.g., FDA, EMA)
National and international regulatory bodies play a crucial role in overseeing clinical research and approving new medical interventions. For example, the U.S. Food and Drug Administration (FDA) is responsible for protecting public health by ensuring the safety, efficacy, and security of human and veterinary drugs, biological products, and medical devices. Similarly, the European Medicines Agency (EMA) is responsible for the scientific evaluation, supervision, and safety monitoring of medicines in the E.U. These bodies act as stringent auditors, meticulously scrutinizing every facet of research before giving their seal of approval. Their primary role is to serve as a critical check on the claims made about new treatments.
Audits and Inspections
Regulatory agencies and institutional bodies periodically conduct audits and inspections of research sites, sponsor organizations, and contract research organizations (CROs) to verify compliance with regulations and GCP guidelines. These evaluations are designed to ensure data integrity, protocol adherence, and ethical conduct. They represent a kind of quality control check on the entire research process, identifying deviations and pushing for corrective actions.
The Impact and Future of Certified Clinical Research
| Metric | Description | Typical Value/Range | Source/Notes |
|---|---|---|---|
| Number of Certified Clinical Research Professionals (CCRP) | Total individuals holding CCRP certification | Over 10,000 worldwide | Society of Clinical Research Associates (SoCRA) |
| Average Study Enrollment Time | Time taken to enroll participants in clinical trials | 3 to 6 months | Industry benchmarks |
| Certification Exam Pass Rate | Percentage of candidates passing the CCRP exam on first attempt | 65% – 75% | SoCRA annual reports |
| Continuing Education Units (CEUs) Required | CEUs needed to maintain certification every 3 years | 45 CEUs | SoCRA certification maintenance policy |
| Average Salary for Certified Clinical Research Professionals | Annual salary range for CCRP holders | 70,000 – 110,000 | Industry salary surveys |
| Clinical Trial Success Rate | Percentage of trials completed successfully with certified staff | Approximately 80% | Industry data |
| Years of Experience Required for Certification | Minimum clinical research experience before eligibility | 2 years | SoCRA eligibility criteria |
Certified clinical research has been a powerful engine for medical progress, transforming health outcomes globally. Its future promises further innovation, driven by new technologies and evolving methodologies.
Advancing Medical Treatments and Diagnostics
The direct impact of certified clinical research is evident in the vast array of effective treatments and sophisticated diagnostics currently available. From vaccines eradicating diseases to therapies prolonging lives and imaging techniques precisely identifying conditions, these advancements are direct descendants of meticulous clinical trials. It’s the river that feeds the fertile soil of medical innovation, allowing new crops of therapies to flourish.
Personalized Medicine and Precision Trials
The future of medical research is increasingly leaning towards personalized medicine, tailoring treatments to an individual’s unique genetic makeup, environment, and lifestyle. This shift necessitates precision clinical trials, often leveraging biomarkers and genomic data to identify specific patient populations most likely to benefit from a particular intervention. This is akin to moving from a general recipe to a bespoke meal, precisely calibrated for an individual’s unique needs. Expect to see smaller, more targeted trials with higher success rates in the coming decades.
Technology Integration (AI, Big Data, Wearables)
Emerging technologies are set to revolutionize how clinical research is conducted. Artificial intelligence (AI) can analyze vast datasets to identify potential drug candidates or predict patient responses. Big data analytics allows for more efficient recruitment and identification of patterns. Wearable devices offer continuous, real-world data collection, moving beyond episodic clinic visits. These tools are poised to streamline processes, enhance data collection, and provide deeper insights, ultimately accelerating the pace of discovery. Imagine these technologies as powerful telescopes and microscopes, allowing researchers to see further and with greater detail than ever before.
In conclusion, certified clinical research is not merely a collection of procedures; it is a rigorous, ethical, and indispensable process that transforms scientific curiosity into tangible health benefits. It is the unseen scaffolding that supports the towering edifice of modern medicine, ensuring its stability, integrity, and continuous growth. As you rely on medical care, remember that every treatment, every diagnostic test, and every preventative measure you encounter has likely passed through the discerning filter of certified clinical research, a testament to its enduring value.



