Paid medical research studies, often referred to as clinical trials or medical studies, are systematic investigations involving human volunteers. The primary objective of these studies is to evaluate the safety and efficacy of new drugs, medical devices, diagnostic procedures, or other interventions. Participants are compensated for their time, inconvenience, and any travel expenses incurred during the study. This compensation acts as an incentive, acknowledging the valuable contribution individuals make to scientific advancement and public health.
The landscape of medical research is constantly evolving, with new diseases emerging and existing ones requiring more effective treatments. Clinical trials are the bedrock upon which medical innovation is built. They serve as a crucial bridge between laboratory discoveries and widespread medical application. Without human participation, the potential benefits of numerous breakthroughs would remain unrealized.
The Role of Clinical Trials
Clinical trials adhere to strict ethical guidelines and regulatory frameworks established by bodies such as the Food and Drug Administration (FDA) in the United States, the European Medicines Agency (EMA), and similar organizations globally. These regulations are designed to protect the rights, safety, and well-being of participants.
- Phases of Clinical Trials: Most clinical trials progress through several phases, each with a distinct objective:
- Phase 0: Exploratory trials in a small number of participants, often to understand drug pharmacokinetics.
- Phase I: Focus on safety and dosage in a small group of healthy volunteers or patients with a specific condition.
- Phase II: Evaluate efficacy and further assess safety in a larger group of patients.
- Phase III: Compare the new intervention to existing treatments or a placebo in a large, diverse patient population to confirm efficacy and monitor adverse effects.
- Phase IV: Post-marketing studies conducted after a drug or device has been approved, to gather additional information on risks, benefits, and optimal use.
Each phase represents a hurdle in the development process, ensuring that only interventions demonstrating a favorable risk-benefit profile proceed to the next stage.
Who Can Participate and Why?
Eligibility criteria for paid medical research studies vary significantly depending on the nature of the research. Factors such as age, gender, medical history, current medications, and the presence of specific health conditions are frequently assessed. Researchers meticulously define these criteria to ensure the study population is appropriate for the scientific inquiry and to minimize confounding variables.
- Reasons for Participation: Individuals choose to participate in medical research for various reasons:
- Financial Compensation: This is a primary motivator for many, providing an income source for their time and effort.
- Access to New Treatments: Participants, particularly those with conditions for which current treatments are ineffective, may gain early access to experimental therapies.
- Contribution to Science: Many individuals are driven by a desire to contribute to medical knowledge and help others.
- Regular Medical Monitoring: Some studies involve frequent medical check-ups and monitoring, which can be beneficial to participants.
It is important for prospective participants to understand that while there are potential benefits, participation also carries inherent risks, which are carefully explained during the informed consent process.
Locating Paid Medical Research Studies
Finding paid medical research studies requires a systematic approach. Several avenues exist for individuals seeking to participate, ranging from online databases to direct contact with research institutions.
Online Databases and Registries
The internet serves as a central hub for information regarding ongoing clinical trials. Several reputable online platforms consolidate listings from various sponsors and research sites.
- ClinicalTrials.gov: This is a comprehensive database maintained by the U.S. National Library of Medicine. It lists publicly and privately funded clinical studies conducted around the world. Users can search by condition, intervention, location, and other parameters. Each listing provides detailed information about the study, including eligibility criteria, contact information, and study locations.
- CenterWatch: This platform offers a searchable database of clinical trials, along with educational resources for participants. It caters to both healthy volunteers and individuals with specific medical conditions.
- NIH Clinical Research Trials and You: A resource provided by the National Institutes of Health, offering general information about clinical trials and links to relevant databases.
When utilizing these databases, focus on studies that are actively recruiting and match your health profile and geographical location.
Pharmaceutical Company Websites
Many pharmaceutical companies conduct their own clinical trials and often list recruitment opportunities on their official websites. These companies are the primary developers of new drugs and thus a significant source of research opportunities.
- Direct Searches: Visit the websites of major pharmaceutical companies (e.g., Pfizer, Johnson & Johnson, AstraZeneca) and navigate to their “Clinical Trials” or “Research & Development” sections. These sections often have dedicated portals for prospective participants.
- Therapeutic Area Focus: If you have a specific medical condition, you might narrow your search to companies specializing in treatments for that condition.
While direct company websites can be a source, it’s often more efficient to start with larger aggregated databases first.
Research Institutions and Medical Centers
Academic medical centers, universities with medical schools, and dedicated research institutions are hubs for clinical research. They frequently conduct studies sponsored by pharmaceutical companies, government agencies, or their own internal research initiatives.
- University Hospitals: Institutions like Harvard Medical School, Stanford University, and Johns Hopkins Medicine have extensive research programs. Their websites typically feature sections detailing ongoing clinical trials and how to volunteer.
- Dedicated Research Centers: Some organizations specialize solely in clinical research, contracting with various sponsors. These sites often maintain their own participant databases and recruitment lists.
- Local Healthcare Providers: Your primary care physician or specialist may be aware of local research opportunities or be affiliated with a research institution. They can serve as a valuable conduit for information.
Engaging with these institutions directly can provide access to studies that may not be extensively advertised elsewhere.
The Informed Consent Process

Informed consent is a cornerstone of ethical medical research. Before participating in any study, individuals must undergo a comprehensive informed consent process, which ensures they fully understand the nature of the research, its potential risks and benefits, and their rights as a participant. It’s not merely a signature on a form; it’s a dialogue.
What Informed Consent Entails
The informed consent document (ICD) is a detailed written explanation of the study. Researchers or their designees will review this document with you, providing ample opportunity for questions and clarification.
- Study Purpose: A clear explanation of what the study aims to achieve.
- Procedures: A description of all tests, interventions, and appointments involved.
- Risks and Discomforts: A comprehensive list of potential side effects, discomforts, or risks associated with the experimental intervention and study procedures. This is often the most critical section for participants to understand.
- Benefits: A discussion of potential direct or indirect benefits you might experience, though it’s crucial to understand that direct personal benefit is not guaranteed.
- Alternatives: Information about alternative treatments or care options available outside the study.
- Confidentiality: Assurance regarding the protection of your personal and medical information.
- Voluntary Participation: Emphasizing that participation is voluntary and you can withdraw at any time without penalty or loss of benefits.
- Compensation: Details regarding the financial compensation, including payment schedule and total amount.
The informed consent process is designed to empower participants, allowing them to make an autonomous decision based on complete information. Viewing yourself as a co-pilot, not a passenger, in the research journey is essential during this stage.
Your Rights as a Participant
Beyond the information provided in the ICD, participants have specific rights that are protected by ethical guidelines and regulations.
- Right to Ask Questions: You have the right to ask as many questions as needed until you fully understand all aspects of the study.
- Right to Withdraw: You can withdraw from the study at any time, for any reason, without fear of reprisal or impact on your routine medical care.
- Right to Privacy: Your personal health information will be kept confidential, typically through anonymization or pseudonymization.
- Right to Information: You have the right to be informed of any new information that arises during the study that might affect your willingness to continue participating.
- Right to Independent Review: All studies are reviewed and approved by an Institutional Review Board (IRB) or Ethics Committee, an independent body that safeguards the rights and welfare of human subjects.
Understanding these rights is paramount to ensuring a safe and ethical research experience.
Compensation and Financial Considerations
Participation in paid medical research studies typically involves financial compensation. This payment is designed to reimburse participants for their time, inconvenience, travel expenses, and sometimes for meals. It is not considered a wage for labor but rather a token of appreciation for their contribution to medical science.
How Compensation is Determined
The amount of compensation varies significantly between studies and is influenced by several factors.
- Study Duration: Longer studies with more visits or extended periods of residence at a facility generally offer higher compensation.
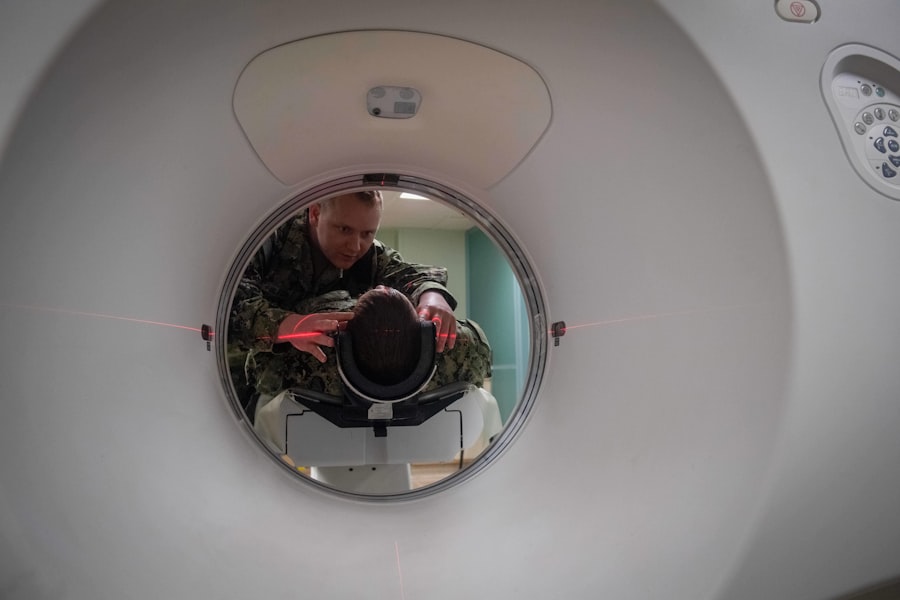
- Complexity of Procedures: Studies involving more invasive procedures (e.g., biopsies, frequent blood draws, specialized imaging) or requiring strict adherence to protocols may offer higher payments.
- Risk Level: Studies perceived as carrying a higher degree of risk or discomfort may offer more attractive compensation, though this is carefully balanced against ethical considerations.
- Scarcity of Participants: Studies seeking individuals with rare conditions or very specific demographics might offer more competitive compensation to attract suitable volunteers.
- Number of Visits: Compensation is often structured per visit or per procedure.
The compensation structure, including the payment schedule (e.g., partial payments after certain milestones, full payment at study completion), will be clearly outlined in the informed consent document.
Tax Implications
In many jurisdictions, compensation received from medical research studies is considered taxable income. This is a crucial point that participants should be aware of.
- IRS Reporting (U.S.): In the United States, if you receive more than a certain threshold (e.g., $600 from a single entity in a calendar year), the research institution or sponsor is typically required to report this income to the Internal Revenue Service (IRS) using Form 1099-MISC or 1099-NEC.
- Record Keeping: It is advisable to keep accurate records of all payments received from research studies throughout the year.
- Consult a Tax Professional: If you anticipate receiving substantial compensation from multiple studies, it is prudent to consult with a tax advisor to understand your obligations and potential deductions.
Failure to report this income can lead to penalties. Transparency regarding tax implications is usually part of the informed consent process.
Ethical Considerations and Risks
| Study Title | Location | Compensation | Duration | Eligibility Criteria | Contact Information |
|---|---|---|---|---|---|
| Diabetes Medication Trial | New York, NY | Up to 1500 | 3 months | Age 18-65, diagnosed with Type 2 Diabetes | researchny@example.com |
| Sleep Disorder Study | Chicago, IL | Up to 800 | 6 weeks | Adults 21-50, diagnosed with insomnia | sleepstudychi@example.com |
| Hypertension Drug Trial | Los Angeles, CA | Up to 1200 | 2 months | Age 30-70, diagnosed with high blood pressure | hypertensionla@example.com |
| Allergy Treatment Research | Houston, TX | Up to 600 | 4 weeks | Adults 18-55, seasonal allergies | allergyhou@example.com |
| Cholesterol Management Study | Miami, FL | Up to 1000 | 3 months | Age 25-65, elevated cholesterol levels | cholesterolmiami@example.com |
While paid medical research studies offer potential benefits, it is imperative to approach them with a clear understanding of the ethical framework and inherent risks. The foundation of all ethical research is the principle of “do no harm” (non-maleficence).
Potential Risks of Participation
Every medical intervention, even a placebo, carries some degree of risk. In clinical trials, these risks can be more pronounced due to the experimental nature of the intervention.
- Adverse Side Effects: The most common risk is experiencing side effects from the investigational drug or device. These can range from mild (e.g., headache, nausea) to severe (e.g., allergic reactions, organ damage).
- Unknown Risks: Because the intervention is new, not all potential risks may be known prior to the study.
- Placebo Effect/No Effect: If you are in a placebo group or the experimental treatment is ineffective, your condition may not improve or could even worsen.
- Inconvenience and Discomfort: Study procedures, such as frequent blood draws, prolonged hospital stays, or diagnostic tests, can be inconvenient or cause physical discomfort.
- Privacy Concerns: Despite safeguards, there is always a theoretical risk of a breach of privacy, though sophisticated measures are in place to prevent this.
The informed consent document meticulously details known risks, and researchers are obligated to inform participants of any new risks that emerge during the study.
Ethical Safeguards for Participants
To mitigate risks and protect participants, a robust system of ethical safeguards is in place.
- Institutional Review Boards (IRBs) / Ethics Committees: These independent, multidisciplinary bodies review and approve all research protocols involving human subjects. Their primary role is to ensure the study is ethically sound, scientifically valid, and that participant rights and welfare are protected.
- Informed Consent: As previously discussed, this process ensures participants make a voluntary, informed decision.
- Data Monitoring Committees (DMCs): For some studies, particularly those with higher risks, independent DMCs monitor data throughout the trial to identify any safety concerns or significant efficacy differences that warrant early termination of the study.
- Confidentiality and Data Security: Strict protocols are implemented to protect participant data, often involving de-identification or anonymization.
- Adherence to GCP (Good Clinical Practice) Guidelines: GCP is an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve the participation of human subjects.
These safeguards act as a safety net, endeavoring to catch potential issues before they cause significant harm.
Making an Informed Decision
Deciding whether to participate in a paid medical research study is a personal one, akin to navigating a winding river where the current is sometimes unknown. It requires careful consideration of the information presented, internal reflection on your motivations, and a clear understanding of the potential implications. Do not hesitate to seek a second opinion from your own healthcare provider before making a commitment. Your health and well-being should remain the paramount concern throughout this decision-making process.



