Clinical trials are a cornerstone of medical research, providing the necessary framework to evaluate the safety and efficacy of new treatments, drugs, and medical devices. Among these, Clinical Trial Applications (CTAs) play a pivotal role in the regulatory process, particularly in the context of drug development. A CTA is a formal request submitted to regulatory authorities, such as the U.S.
Food and Drug Administration (FDA) or the European Medicines Agency (EMA), seeking permission to initiate a clinical trial involving human subjects. This application encompasses detailed information about the proposed study, including its objectives, methodology, and the potential risks and benefits to participants. The significance of CTAs cannot be overstated; they serve as a critical gatekeeping mechanism that ensures the ethical conduct of clinical research.
By requiring comprehensive data on the investigational product and the trial design, regulatory bodies aim to protect participants while also ensuring that the research is scientifically sound. The process of preparing a CTA involves meticulous planning and collaboration among various stakeholders, including researchers, sponsors, and regulatory affairs professionals. As the landscape of clinical research evolves, so too does the complexity of CTAs, necessitating ongoing advancements in technology and methodology to streamline the process and enhance patient safety.
Key Takeaways
- CTA clinical trials are essential for evaluating new treatments and improving patient outcomes.
- Technological advancements have enhanced the accuracy and efficiency of CTA clinical trials.
- Emerging trends include personalized medicine approaches and integration of AI in trial design.
- Recent trials highlight significant findings that could transform diagnostic and therapeutic strategies.
- Addressing challenges such as data management and patient recruitment is crucial for future success.
Advancements in CTA Clinical Trial Technology
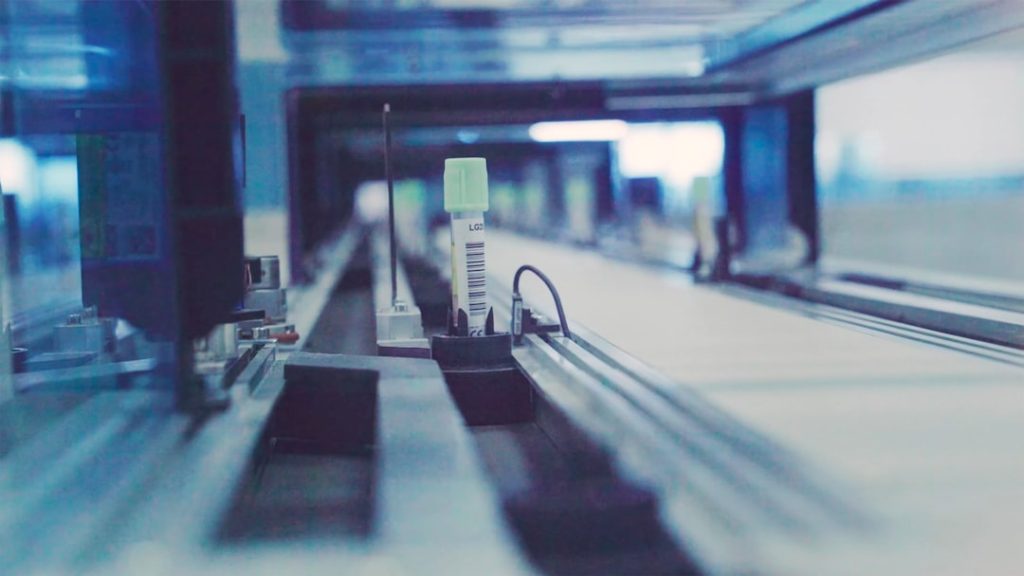
The landscape of clinical trials has been transformed by technological advancements that have significantly improved the efficiency and effectiveness of CTAs. One notable development is the integration of electronic systems for submitting and managing CTAs. Electronic Common Technical Document (eCTD) formats have become standard practice, allowing for more streamlined submissions that can be easily updated and tracked.
This shift from paper-based submissions to electronic formats not only accelerates the review process but also enhances data integrity and accessibility for regulatory authorities. Moreover, advancements in data analytics and artificial intelligence (AI) are revolutionizing how clinical trial data is collected, analyzed, and reported. AI algorithms can sift through vast amounts of data to identify patterns and predict outcomes, thereby informing trial design and patient recruitment strategies.
For instance, machine learning models can analyze historical trial data to optimize patient selection criteria, ensuring that participants are more likely to benefit from the investigational treatment. This not only improves the chances of trial success but also minimizes the risk of exposing patients to ineffective or harmful interventions.
Emerging Trends in CTA Clinical Trials

As the field of clinical research continues to evolve, several emerging trends are shaping the future of CTAs. One significant trend is the increasing emphasis on patient-centric approaches in trial design. Researchers are recognizing the importance of incorporating patient perspectives into the development process, leading to more relevant and acceptable study designs.
This shift is evident in initiatives that prioritize patient engagement through advisory boards or focus groups, allowing patients to voice their needs and preferences regarding trial participation. Another notable trend is the rise of decentralized clinical trials (DCTs), which leverage technology to conduct studies outside traditional clinical settings. DCTs utilize telemedicine, mobile health applications, and remote monitoring devices to facilitate patient participation from their homes.
This approach not only enhances accessibility for patients who may face barriers to attending in-person visits but also allows for more diverse participant populations. As regulatory agencies adapt to these changes, they are developing guidelines that support the implementation of DCTs while ensuring that safety and data integrity remain paramount.
Key Findings from Recent CTA Clinical Trials
Recent CTA clinical trials have yielded significant findings that underscore the importance of rigorous research methodologies and innovative approaches. For example, a recent trial investigating a novel immunotherapy for melanoma demonstrated promising results in terms of overall survival rates compared to standard treatments. The study’s design incorporated adaptive trial methodologies, allowing researchers to modify treatment protocols based on interim results.
This flexibility not only accelerated the identification of effective treatment regimens but also minimized patient exposure to less effective therapies. Additionally, findings from trials focused on rare diseases have highlighted the potential for targeted therapies to make substantial impacts on patient outcomes. In one such study, a gene therapy trial for a rare genetic disorder showed remarkable improvements in patients’ quality of life and functional abilities.
These results emphasize the critical role that CTAs play in advancing treatment options for underserved populations, showcasing how innovative research can lead to breakthroughs that were previously thought unattainable.
Challenges and Opportunities in CTA Clinical Trials
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of CTA Clinical Trials | Total clinical trials registered under the Clinical Trials Act (CTA) | 1,250 | Trials |
| Average Enrollment | Average number of participants per CTA clinical trial | 150 | Participants |
| Trial Phases Distribution | Percentage distribution of trials by phase | Phase 1: 20%, Phase 2: 35%, Phase 3: 30%, Phase 4: 15% | Percentage |
| Average Trial Duration | Mean duration from trial start to completion | 24 | Months |
| Primary Therapeutic Areas | Most common disease areas studied in CTA trials | Oncology, Cardiovascular, Neurology | Categories |
| Trial Completion Rate | Percentage of trials completed as planned | 78 | Percentage |
| Number of Sponsors | Total unique sponsors conducting CTA clinical trials | 320 | Sponsors |
Despite the advancements in technology and methodology, CTA clinical trials face several challenges that can hinder their progress. One major obstacle is the complexity of regulatory requirements across different jurisdictions. Each regulatory body has its own set of guidelines and expectations for CTAs, which can create confusion and delays for sponsors seeking to conduct multinational trials.
Navigating these regulatory landscapes requires expertise and resources that may not be readily available to all research organizations. However, these challenges also present opportunities for improvement within the field. The growing trend toward harmonization of regulatory standards offers a pathway for streamlining CTA processes across borders.
Initiatives such as the International Council for Harmonisation (ICH) aim to create unified guidelines that can facilitate smoother submissions and approvals. Furthermore, collaboration among stakeholders—including regulatory agencies, industry representatives, and patient advocacy groups—can foster a more efficient environment for conducting clinical trials while ensuring that patient safety remains a top priority.
The Impact of CTA Clinical Trials on Patient Care

The implications of CTA clinical trials extend far beyond the confines of research laboratories; they have a profound impact on patient care and treatment options available in clinical practice. Successful trials often lead to the approval of new therapies that can significantly improve patient outcomes, particularly in areas where existing treatments are limited or ineffective. For instance, recent advancements in CAR-T cell therapy have transformed the landscape of hematologic malignancies, offering hope to patients with previously untreatable conditions.
Moreover, CTA clinical trials contribute to the broader understanding of disease mechanisms and treatment responses, ultimately informing clinical guidelines and best practices. By generating robust evidence through well-designed studies, researchers can provide healthcare professionals with valuable insights into how to optimize treatment regimens for diverse patient populations. This evidence-based approach not only enhances individual patient care but also contributes to public health by improving overall treatment strategies within healthcare systems.
Future Directions for CTA Clinical Trials
Looking ahead, several key directions are poised to shape the future of CTA clinical trials. One promising avenue is the continued integration of digital health technologies into trial designs. Wearable devices and mobile applications can facilitate real-time data collection and monitoring, enabling researchers to gather more comprehensive insights into patient experiences and treatment effects.
This shift toward real-world evidence will enhance the relevance of trial findings and support more personalized approaches to patient care. Additionally, as precision medicine gains traction, future CTAs will likely focus on tailoring treatments based on individual genetic profiles or biomarkers. This approach not only holds promise for improving treatment efficacy but also minimizes adverse effects by ensuring that patients receive therapies most suited to their unique characteristics.
As researchers continue to explore innovative methodologies and technologies, it is essential that regulatory frameworks evolve in tandem to support these advancements while maintaining rigorous safety standards.
Conclusion and Recommendations for CTA Clinical Trials
In conclusion, CTA clinical trials represent a vital component of medical research that drives innovation and improves patient care. As advancements in technology continue to reshape the landscape of clinical trials, it is crucial for stakeholders to remain adaptable and proactive in addressing emerging challenges. Regulatory agencies should prioritize harmonization efforts to streamline processes across jurisdictions while fostering collaboration among industry partners.
Furthermore, embracing patient-centric approaches will enhance trial designs and ensure that research aligns with patient needs and preferences. By leveraging digital health technologies and focusing on precision medicine, future CTAs can pave the way for groundbreaking therapies that transform healthcare outcomes. Ultimately, a commitment to rigorous scientific inquiry combined with a focus on patient welfare will ensure that CTA clinical trials continue to play a pivotal role in advancing medical knowledge and improving lives worldwide.