Clinical project management is a critical discipline within the healthcare and pharmaceutical industries, serving as the backbone for the successful execution of clinical trials and research initiatives. The complexity of clinical projects, which often involve multiple stakeholders, regulatory requirements, and intricate timelines, necessitates a structured approach to ensure that objectives are met efficiently and effectively. The role of a clinical project manager is multifaceted, encompassing planning, execution, monitoring, and closure of projects while ensuring compliance with ethical standards and regulatory guidelines.
This level of oversight is essential not only for the integrity of the research but also for the safety and well-being of participants involved in clinical trials. Moreover, the importance of clinical project management extends beyond mere compliance and operational efficiency. It plays a pivotal role in fostering innovation within the healthcare sector.
By streamlining processes and enhancing collaboration among cross-functional teams, clinical project management facilitates the rapid development of new therapies and medical devices. This is particularly crucial in an era where the demand for novel treatments is ever-increasing, driven by factors such as aging populations and the rise of chronic diseases. Effective project management can significantly reduce time-to-market for new drugs and therapies, ultimately benefiting patients and healthcare systems alike.
Key Takeaways
- Clinical project management is crucial for ensuring successful trial outcomes and regulatory compliance.
- Clear goals and objectives provide direction and measurable milestones for clinical projects.
- Effective communication and collaboration enhance team coordination and stakeholder engagement.
- Utilizing specialized project management tools improves efficiency and tracking of clinical activities.
- Proactive risk management and continuous monitoring help mitigate issues and optimize project performance.
Setting Clear Goals and Objectives for Clinical Projects
Establishing clear goals and objectives is foundational to the success of any clinical project. These goals serve as a roadmap, guiding the project team through various phases of the trial while ensuring alignment with broader organizational objectives. In clinical research, goals may range from specific endpoints related to patient outcomes to broader objectives such as market approval for a new drug.
The SMART criteria—Specific, Measurable, Achievable, Relevant, and Time-bound—are often employed to formulate these objectives, ensuring that they are not only clear but also attainable within the project’s constraints. In addition to setting initial goals, it is crucial to engage stakeholders in this process. Stakeholders may include clinical researchers, regulatory bodies, funding organizations, and patient advocacy groups.
By involving these parties in goal-setting discussions, project managers can gain valuable insights that enhance the relevance and feasibility of the objectives. For instance, input from patient advocacy groups can help ensure that trial endpoints reflect what is meaningful to patients, thereby increasing the likelihood of participant recruitment and retention. This collaborative approach not only strengthens the project’s foundation but also fosters a sense of ownership among stakeholders, which can be instrumental in navigating challenges that arise during the project lifecycle.
Implementing Effective Communication and Collaboration Strategies

Effective communication is a cornerstone of successful clinical project management. Given the diverse array of stakeholders involved in clinical trials—from researchers and sponsors to regulatory agencies and patients—establishing clear lines of communication is essential for ensuring that everyone is on the same page. Regular updates, status reports, and meetings can help maintain transparency and facilitate information sharing among team members.
Utilizing various communication channels—such as emails, video conferences, and collaborative platforms—can cater to different preferences and enhance engagement. Collaboration strategies also play a vital role in fostering teamwork among cross-functional groups. In clinical projects, team members often come from diverse backgrounds, including clinical research, biostatistics, regulatory affairs, and data management.
Encouraging an environment where team members feel comfortable sharing ideas and feedback can lead to innovative solutions to complex problems. For example, implementing regular brainstorming sessions or workshops can stimulate creative thinking and allow team members to contribute their unique perspectives. Additionally, leveraging collaborative tools such as shared document repositories or project management software can streamline workflows and enhance coordination among team members.
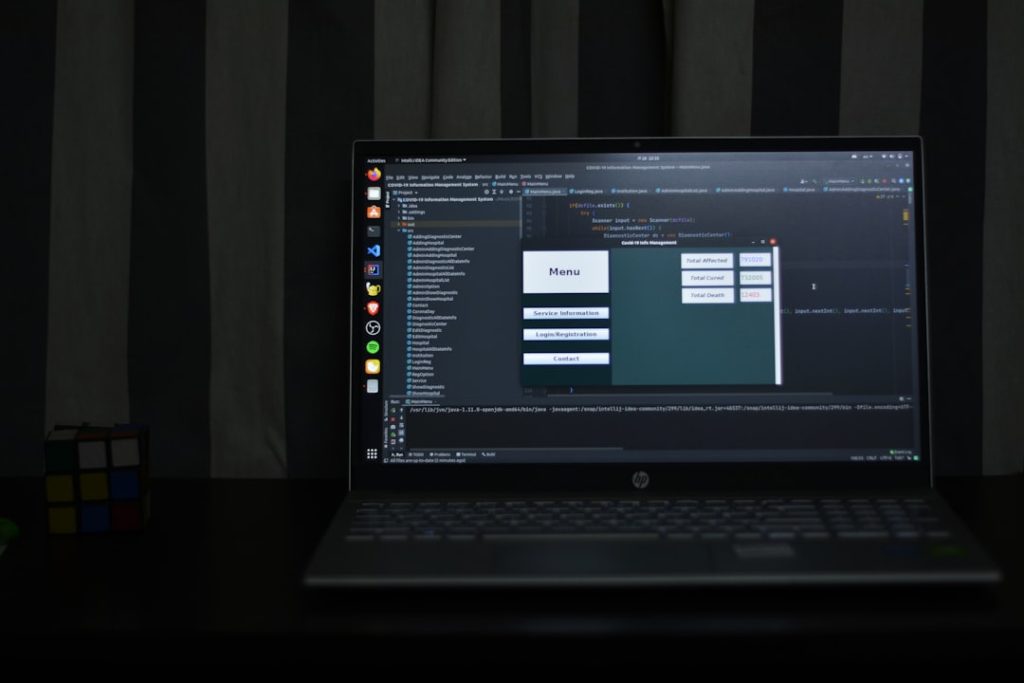
Utilizing Project Management Tools and Software
The advent of technology has revolutionized project management across various industries, including clinical research. A plethora of project management tools and software solutions are available that cater specifically to the needs of clinical project managers. These tools can assist in planning, tracking progress, managing resources, and ensuring compliance with regulatory requirements.
For instance, electronic data capture (EDC) systems enable real-time data collection and monitoring during clinical trials, significantly improving data accuracy and reducing the time spent on data entry. Moreover, project management software can facilitate task assignment and progress tracking through visual dashboards that provide an overview of project milestones and timelines. Tools like Gantt charts or Kanban boards allow project managers to visualize workflows and identify bottlenecks early in the process.
This level of visibility is crucial for maintaining momentum in clinical projects where delays can have significant implications for timelines and budgets. By utilizing these technological solutions effectively, clinical project managers can enhance their ability to deliver projects on time and within scope.
Managing Resources and Budgets Effectively
| Metric | Description | Typical Value/Range | Importance |
|---|---|---|---|
| Study Start-Up Time | Time from protocol approval to first patient enrolled | 3-6 months | High – impacts overall project timeline |
| Patient Recruitment Rate | Number of patients enrolled per site per month | 2-5 patients/site/month | High – critical for meeting enrollment targets |
| Protocol Deviation Rate | Percentage of enrolled patients with protocol deviations | 1-5% | Medium – affects data quality and regulatory compliance |
| Data Query Rate | Number of data queries per 100 case report forms (CRFs) | 5-15 queries/100 CRFs | Medium – indicates data quality and monitoring effectiveness |
| Site Activation Time | Time from site selection to site initiation visit | 1-3 months | High – affects recruitment start |
| Patient Retention Rate | Percentage of patients completing the study | 80-95% | High – impacts study validity and data completeness |
| Budget Variance | Difference between planned and actual project costs | ±10% | High – critical for financial management |
| Adverse Event Reporting Time | Time from adverse event occurrence to reporting | 24-72 hours | High – regulatory compliance and patient safety |
| Monitoring Visit Frequency | Number of monitoring visits per site per month | 1-2 visits | Medium – ensures data integrity and compliance |
| Regulatory Submission Time | Time taken to prepare and submit regulatory documents | 1-2 months | High – impacts study start and compliance |
Resource management is a critical aspect of clinical project management that directly impacts a project’s success. Clinical trials often require substantial financial investment, human resources, and material assets. Therefore, effective budgeting is essential to ensure that resources are allocated appropriately throughout the project’s lifecycle.
A well-structured budget should account for all potential costs associated with the trial, including personnel salaries, site fees, patient recruitment expenses, and regulatory compliance costs. In addition to financial resources, managing human resources effectively is equally important. This involves not only recruiting qualified personnel but also ensuring that team members are adequately trained and supported throughout the project.
For example, providing ongoing training on regulatory requirements or new technologies can enhance team performance and reduce errors during trial execution. Furthermore, fostering a positive work environment that encourages collaboration and professional development can lead to higher job satisfaction among team members, ultimately contributing to better project outcomes.
Identifying and Mitigating Risks in Clinical Projects

Risk management is an integral component of clinical project management that requires proactive identification and mitigation strategies. Clinical trials are inherently fraught with uncertainties—ranging from patient recruitment challenges to unforeseen regulatory hurdles—that can jeopardize project timelines and outcomes. Conducting a thorough risk assessment at the outset of a project allows managers to identify potential risks early on and develop contingency plans to address them.
For instance, if a trial faces challenges in recruiting participants due to stringent eligibility criteria or competition from other studies, project managers may need to adjust their recruitment strategies or broaden eligibility criteria to enhance enrollment rates. Additionally, establishing a risk management framework that includes regular monitoring of identified risks throughout the project lifecycle can help ensure that emerging issues are addressed promptly. By fostering a culture of risk awareness within the project team, managers can empower team members to report potential concerns without hesitation.
Monitoring and Evaluating Project Progress and Outcomes
Continuous monitoring and evaluation are essential for assessing the progress of clinical projects against established goals and objectives. This process involves collecting data on key performance indicators (KPIs) throughout the trial to gauge whether it is on track to meet its targets. Regularly scheduled progress meetings can provide opportunities for team members to discuss challenges encountered during execution and share insights on potential improvements.
Moreover, evaluating outcomes at various stages of the project allows for informed decision-making regarding necessary adjustments or course corrections. For example, if interim analysis reveals that certain endpoints are not being met as anticipated, project managers may need to reassess their strategies or allocate additional resources to address specific challenges. This iterative approach not only enhances accountability but also fosters a culture of continuous improvement within the project team.
Adapting and Improving Project Management Strategies for Future Projects
The landscape of clinical research is constantly evolving due to advancements in technology, regulatory changes, and shifting patient demographics. As such, it is imperative for clinical project managers to remain adaptable and open to refining their strategies based on lessons learned from previous projects. Conducting post-project evaluations can provide valuable insights into what worked well and what could be improved in future endeavors.
For instance, if a particular recruitment strategy proved effective in one trial but fell short in another due to differing patient populations or site capabilities, managers should analyze these discrepancies to inform future planning efforts. Additionally, staying abreast of industry trends—such as the increasing use of decentralized trials or patient-centric approaches—can help managers incorporate innovative practices into their project management frameworks. By fostering a culture of learning within their teams and embracing change as an opportunity for growth, clinical project managers can enhance their effectiveness in delivering successful outcomes in an ever-evolving landscape.