Double blind randomized controlled trials (DBRCTs) are considered the gold standard in clinical research, particularly in the evaluation of new medical interventions. These trials are designed to eliminate bias and ensure that the results are as reliable and valid as possible. In a DBRCT, neither the participants nor the researchers know which individuals are receiving the treatment and which are receiving a placebo or an alternative intervention.
This method is crucial for maintaining objectivity and integrity in the data collected, as it minimizes the influence of expectations on both sides. The randomized aspect of these trials involves assigning participants to different groups in a manner that is entirely random, often using computer-generated random numbers. This process helps to ensure that the groups are comparable at the start of the trial, which is essential for attributing any observed effects to the intervention being tested rather than to pre-existing differences between groups.
The combination of double blinding and randomization creates a robust framework for assessing the efficacy and safety of new treatments, making DBRCTs a cornerstone of evidence-based medicine.
Key Takeaways
- Double blind randomized controlled trials (RCTs) are essential for minimizing bias in clinical research.
- Randomization ensures unbiased allocation of participants, enhancing the validity of trial results.
- Control groups provide a baseline to compare the effects of new treatments accurately.
- Ethical considerations are critical to protect participant rights and maintain trial integrity.
- Advances in trial methodology aim to improve efficiency and address current challenges in RCTs.
The Importance of Double Blinding in Clinical Trials
Double blinding serves a critical function in clinical trials by preventing bias from influencing the outcomes. When participants are aware of whether they are receiving the treatment or a placebo, their expectations can significantly affect their perceptions of efficacy and side effects. For instance, if a participant knows they are receiving a new drug, they may report improvements in their condition simply because they expect to feel better, a phenomenon known as the placebo effect.
Conversely, if they are aware they are receiving a placebo, they may report more negative outcomes due to their expectations of ineffectiveness. Researchers also face potential biases that can skew results. If investigators know which participants are receiving the treatment, their observations and interactions may unconsciously influence the data collection process.
For example, they might inadvertently provide more encouragement or attention to those receiving the active treatment, leading to discrepancies in reported outcomes. By implementing double blinding, both participant and investigator biases are mitigated, allowing for a more accurate assessment of the treatment’s true effects.
Understanding the Randomization Process in Clinical Trials

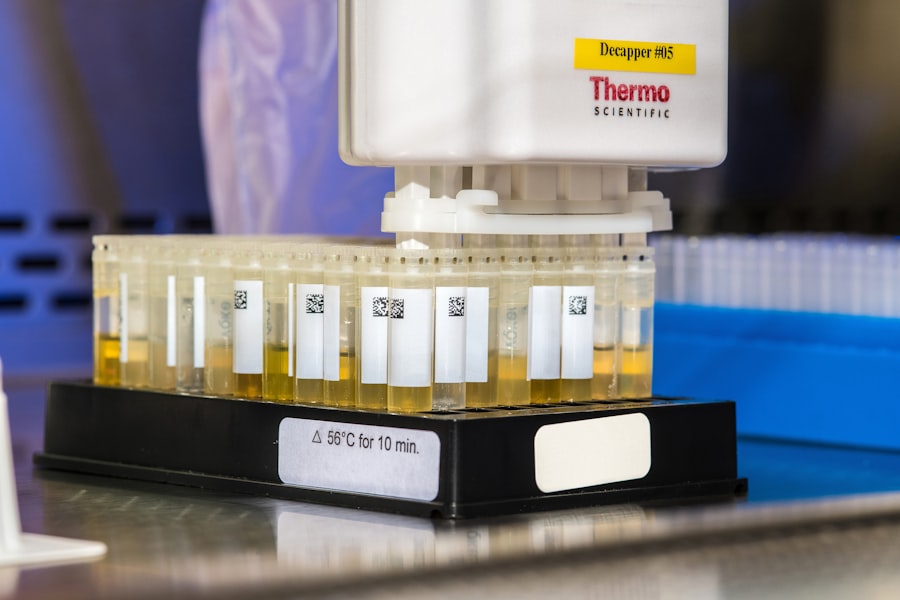
Randomization is a fundamental component of DBRCTs that ensures each participant has an equal chance of being assigned to any group within the study. This process is vital for creating comparable groups that can be analyzed for differences in outcomes. Randomization can be achieved through various methods, including simple random sampling, stratified random sampling, or block randomization.
Each method has its advantages and is chosen based on the specific needs of the trial. For instance, simple random sampling might involve assigning participants numbers and using a random number generator to select who goes into each group. Stratified random sampling, on the other hand, ensures that specific subgroups (such as age or gender) are evenly distributed across treatment groups, which can be particularly important in trials where these factors may influence outcomes.
Block randomization helps maintain balance between groups throughout the trial by ensuring that an equal number of participants are assigned to each group at regular intervals. This careful consideration of randomization methods is crucial for maintaining the integrity of the trial’s findings.
The Role of Control Groups in Clinical Trials
Control groups play an essential role in DBRCTs by providing a baseline against which the effects of the experimental treatment can be measured. Typically, control groups receive either a placebo or an existing standard treatment rather than the new intervention being tested. This comparison allows researchers to determine whether any observed effects in the treatment group can be attributed to the intervention itself rather than other external factors.
The use of control groups also helps to account for natural variations in health outcomes that may occur over time. For example, in a trial assessing a new antidepressant, both groups may show improvements over time due to factors such as therapy or lifestyle changes unrelated to the medication. By comparing outcomes between the treatment and control groups, researchers can isolate the specific impact of the new drug on participants’ mental health.
This rigorous comparison is vital for establishing causality and ensuring that new treatments are both effective and safe before they are approved for widespread use.
Assessing the Effectiveness of New Drugs through Double Blind Randomized Controlled Trials
| Metric | Description | Typical Value/Range | Importance |
|---|---|---|---|
| Sample Size | Number of participants enrolled in the trial | 50 – 1000+ | Determines statistical power and reliability of results |
| Randomization Method | Process used to assign participants to groups | Simple, Block, Stratified, or Computer-generated | Reduces selection bias and balances confounding variables |
| Blinding | Both participants and researchers unaware of group assignments | Double-blind | Prevents performance and detection bias |
| Control Group | Group receiving placebo or standard treatment | Placebo or active comparator | Provides baseline for comparison |
| Primary Outcome Measure | Main variable measured to assess treatment effect | Depends on study (e.g., symptom reduction, survival rate) | Determines efficacy of intervention |
| Duration | Length of time participants are followed | Weeks to years | Ensures adequate time to observe outcomes |
| Dropout Rate | Percentage of participants who do not complete the trial | Typically 5% – 20% | Affects validity and generalizability of results |
| Statistical Significance | Probability that results are not due to chance | p-value < 0.05 | Indicates reliability of findings |
DBRCTs are instrumental in assessing the effectiveness of new drugs because they provide a structured environment for evaluating both efficacy and safety. The design allows researchers to collect data on various outcomes, such as symptom relief, side effects, and overall quality of life. For instance, in a trial evaluating a novel cancer therapy, researchers might measure tumor size reduction as a primary outcome while also assessing secondary outcomes like patient-reported quality of life and adverse events.
The statistical analysis performed on data from DBRCTs is rigorous and often involves complex methodologies to ensure that results are valid and reliable. Researchers typically use intention-to-treat analysis, which includes all participants as originally assigned regardless of whether they completed the study or adhered to treatment protocols. This approach helps prevent bias introduced by dropouts or noncompliance and provides a more accurate reflection of how the drug would perform in real-world settings.
Challenges and Limitations of Double Blind Randomized Controlled Trials
Despite their strengths, DBRCTs face several challenges and limitations that can impact their execution and findings. One significant challenge is recruitment; finding enough eligible participants who meet specific inclusion criteria can be difficult, particularly for rare diseases or conditions. Additionally, participants may drop out during the trial for various reasons, including adverse effects or lack of perceived benefit from the treatment.
High dropout rates can lead to incomplete data and affect the overall validity of the trial results. Another limitation is that DBRCTs can be resource-intensive and time-consuming. They often require substantial funding, extensive planning, and coordination among multiple sites or institutions.
Furthermore, ethical considerations may arise when withholding potentially beneficial treatments from control group participants, particularly in cases where effective therapies already exist. These challenges necessitate careful planning and consideration when designing DBRCTs to ensure that they yield meaningful and applicable results.
Ethical Considerations in Double Blind Randomized Controlled Trials
Ethical considerations are paramount in conducting DBRCTs, as they involve human subjects who may be vulnerable or facing serious health conditions. Informed consent is a critical component; participants must be fully aware of what participation entails, including potential risks and benefits. Researchers have an ethical obligation to ensure that participants understand their rights and can withdraw from the study at any time without penalty.
Moreover, ethical review boards play an essential role in overseeing clinical trials to ensure that they adhere to established ethical standards. These boards evaluate study protocols to assess whether risks are minimized and whether potential benefits justify those risks. In cases where there is already an established effective treatment available, researchers must carefully consider whether it is ethical to assign participants to a placebo group instead of providing them with proven care.
Future Implications and Advancements in Clinical Trial Methodology
As medical research continues to evolve, so too do methodologies for conducting clinical trials. Innovations such as adaptive trial designs allow researchers to modify aspects of a trial based on interim results without compromising its integrity. This flexibility can lead to more efficient trials that adapt to emerging data regarding efficacy or safety.
Additionally, advancements in technology have facilitated remote monitoring and data collection through digital health tools and mobile applications. These technologies enable researchers to gather real-time data from participants outside traditional clinical settings, potentially increasing participant engagement and retention while also broadening access to diverse populations. Furthermore, there is growing interest in incorporating real-world evidence into clinical trial designs.
By integrating data from electronic health records or patient registries, researchers can enhance their understanding of how new treatments perform across varied populations and settings beyond controlled environments. This approach not only enriches clinical research but also aligns with regulatory agencies’ increasing emphasis on real-world evidence when evaluating new therapies. In summary, double blind randomized controlled trials remain a cornerstone of clinical research methodology due to their ability to minimize bias and provide robust evidence regarding treatment efficacy and safety.
As methodologies continue to advance and adapt to modern challenges, DBRCTs will likely evolve further, enhancing their relevance and applicability in an ever-changing healthcare landscape.