Multiple myeloma is a complex and multifaceted hematological malignancy characterized by the proliferation of abnormal plasma cells in the bone marrow. These malignant plasma cells produce an excess of monoclonal immunoglobulins, which can lead to various complications, including bone lesions, renal impairment, and immune dysfunction. The disease is often insidious in its onset, with many patients experiencing vague symptoms such as fatigue, bone pain, or recurrent infections that may not immediately raise suspicion for a hematological disorder.
The pathophysiology of multiple myeloma involves a combination of genetic mutations, environmental factors, and the microenvironment of the bone marrow, which collectively contribute to the survival and proliferation of these malignant cells. The incidence of multiple myeloma varies significantly across different demographics, with higher rates observed in older adults and certain ethnic groups, particularly African Americans. The median age at diagnosis is around 69 years, and while the exact cause remains largely unknown, several risk factors have been identified.
These include a family history of the disease, exposure to certain chemicals such as benzene, and prior monoclonal gammopathy of undetermined significance (MGUS), which is considered a precursor condition. Understanding these risk factors is crucial for early detection and intervention, as early-stage multiple myeloma can often be asymptomatic and may go unnoticed until it progresses to a more advanced stage.
Key Takeaways
- Multiple myeloma is a cancer of plasma cells that requires specific diagnostic tests for accurate detection.
- Treatment options include chemotherapy, stem cell transplant, and newer targeted therapies.
- Prognosis varies based on disease stage, with survival rates improving due to advances in treatment.
- Emerging therapies and clinical trials offer hope for more effective and personalized treatments.
- Supportive care and coping strategies are essential to maintain quality of life for patients.
Diagnostic Tools and Tests for Multiple Myeloma
The diagnosis of multiple myeloma typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. A thorough medical history and physical examination are essential first steps in identifying potential symptoms associated with the disease. Laboratory tests play a pivotal role in confirming the diagnosis; these include serum protein electrophoresis (SPEP) and immunofixation electrophoresis (IFE), which help identify the presence of monoclonal proteins (M-proteins) in the blood.
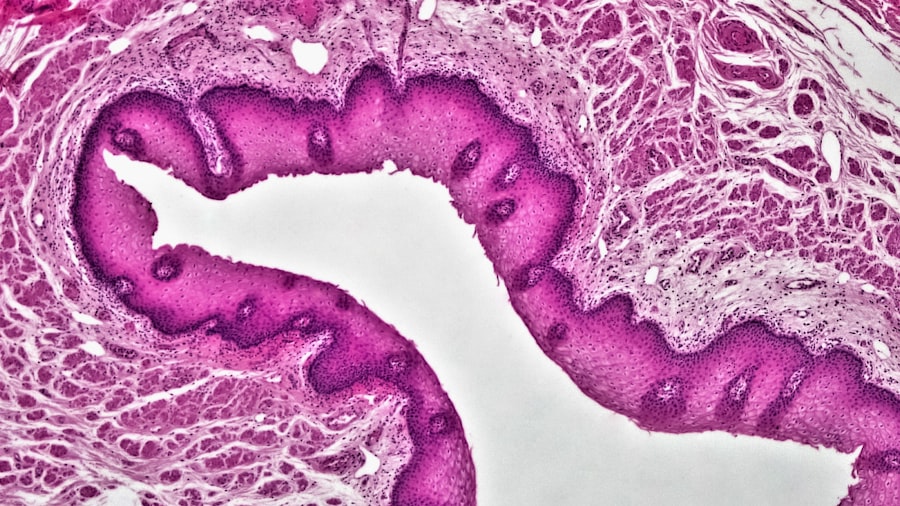
Additionally, serum free light chain assays can provide valuable information regarding the light chain production by plasma cells, aiding in the diagnosis and monitoring of the disease. Bone marrow biopsy remains the gold standard for diagnosing multiple myeloma. This procedure involves extracting a small sample of bone marrow, typically from the hip bone, to assess for the presence of abnormal plasma cells.
A diagnosis is generally confirmed when at least 10% of the bone marrow consists of these malignant cells, along with evidence of related organ damage or specific biomarkers. Imaging studies such as X-rays, magnetic resonance imaging (MRI), or positron emission tomography (PET) scans are also utilized to evaluate bone involvement and detect lytic lesions that are characteristic of multiple myeloma. These diagnostic tools collectively provide a comprehensive understanding of the disease’s extent and severity.
Treatment Options for Multiple Myeloma
The treatment landscape for multiple myeloma has evolved significantly over the past few decades, with advancements in both pharmacological therapies and stem cell transplantation techniques. The choice of treatment is influenced by various factors, including the patient’s age, overall health, disease stage, and specific genetic abnormalities present in the myeloma cells. Standard treatment regimens often include a combination of chemotherapy agents such as melphalan or cyclophosphamide, along with corticosteroids like dexamethasone.
These agents work synergistically to reduce the number of malignant plasma cells and alleviate symptoms. In recent years, novel therapies have emerged that target specific pathways involved in myeloma cell survival and proliferation. Proteasome inhibitors such as bortezomib and carfilzomib disrupt the proteasome’s function, leading to the accumulation of pro-apoptotic factors within malignant cells.
Immunomodulatory drugs like thalidomide, lenalidomide, and pomalidomide enhance the immune response against myeloma cells while also exhibiting direct anti-myeloma effects. Monoclonal antibodies such as daratumumab and elotuzumab have also gained prominence in treatment protocols, targeting specific antigens on myeloma cells to facilitate their destruction by the immune system. For eligible patients, autologous stem cell transplantation (ASCT) remains a cornerstone of treatment for multiple myeloma.
This procedure involves harvesting a patient’s own stem cells before administering high-dose chemotherapy to eradicate malignant cells. Once the chemotherapy is completed, the harvested stem cells are reinfused into the patient to restore normal hematopoiesis. ASCT has been shown to improve overall survival rates significantly; however, it is not suitable for all patients due to age or comorbidities.
Prognosis and Survival Rates for Multiple Myeloma
The prognosis for patients diagnosed with multiple myeloma has improved markedly over recent years due to advancements in treatment options and a better understanding of the disease’s biology. Survival rates can vary widely based on several factors, including age at diagnosis, stage of disease, response to initial therapy, and specific genetic abnormalities present in the myeloma cells. The International Staging System (ISS) is commonly used to stratify patients based on their disease stage, which is determined by serum beta-2 microglobulin and albumin levels.
Patients classified as stage I generally have a better prognosis compared to those in stages II or
| Metric | Value | Unit | Notes |
|---|---|---|---|
| Number of Patients Enrolled | 500 | patients | Across multiple centers |
| Median Progression-Free Survival (PFS) | 18 | months | Estimated from interim analysis |
| Overall Response Rate (ORR) | 75 | % | Includes partial and complete responses |
| Complete Response Rate (CR) | 40 | % | Patients with no detectable disease |
| Median Overall Survival (OS) | Not reached | – | Follow-up ongoing |
| Adverse Event Rate (Grade 3 or higher) | 30 | % | Serious treatment-related events |
| Median Age of Participants | 65 | years | Range 45-80 years |
| Duration of Treatment | 12 | months | Median duration on protocol |
Recent data indicate that the median overall survival for patients with multiple myeloma has increased significantly over the past two decades, with many patients now living well beyond five years post-diagnosis. For instance, studies have shown that patients who achieve a complete response to initial therapy may experience even longer survival times. However, despite these improvements, multiple myeloma remains an incurable disease for most patients; thus, ongoing monitoring and management are essential components of care.
The emergence of minimal residual disease (MRD) testing has provided additional insights into prognosis by detecting low levels of residual myeloma cells post-treatment, allowing for more tailored therapeutic approaches.
Emerging Therapies and Clinical Trials for Multiple Myeloma
The field of multiple myeloma research is rapidly evolving, with numerous emerging therapies currently under investigation in clinical trials. One promising area involves CAR T-cell therapy, which involves genetically modifying a patient’s T-cells to express chimeric antigen receptors that specifically target myeloma cells. Early clinical trials have demonstrated encouraging results with CAR T-cell therapies such as idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel), showing high response rates in heavily pre-treated patients.
Another exciting avenue of research focuses on bispecific T-cell engagers (BiTEs), which are designed to simultaneously bind to both T-cells and myeloma cells, effectively redirecting T-cell activity against malignant plasma cells. Agents like teclistamab have shown promise in early-phase trials, providing new hope for patients who have exhausted conventional treatment options. Additionally, small molecule inhibitors targeting specific signaling pathways involved in myeloma cell survival are being explored; these include inhibitors of B-cell lymphoma 2 (BCL-2) proteins and other novel agents that disrupt critical cellular processes.
Clinical trials play a vital role in advancing our understanding of multiple myeloma and improving treatment outcomes. Patients are encouraged to consider participation in clinical trials as they may provide access to cutting-edge therapies that are not yet widely available. Furthermore, ongoing research into biomarkers that predict response to therapy will likely enhance personalized treatment approaches in the future.
Supportive Care for Patients with Multiple Myeloma
Supportive care is an integral component of managing multiple myeloma, addressing not only the physical aspects of the disease but also its psychological and social implications. Patients often experience a range of symptoms that can significantly impact their quality of life, including pain from bone lesions, fatigue from anemia or treatment side effects, and emotional distress stemming from their diagnosis. A multidisciplinary approach involving oncologists, nurses, social workers, nutritionists, and palliative care specialists is essential to provide comprehensive support tailored to each patient’s needs.
Pain management is particularly crucial for patients with multiple myeloma due to the prevalence of skeletal-related events such as fractures or spinal compression. Effective pain control may involve a combination of pharmacological interventions—such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, or bisphosphonates—and non-pharmacological strategies like physical therapy or acupuncture. Additionally, addressing nutritional needs is vital since many patients may experience weight loss or gastrointestinal side effects from treatments; dietary modifications or supplements can help maintain strength and overall well-being.
Psychosocial support is equally important in managing multiple myeloma. Patients may face anxiety or depression related to their diagnosis and treatment journey. Support groups or counseling services can provide valuable emotional support and coping strategies for both patients and their families.
Furthermore, education about the disease process and treatment options empowers patients to take an active role in their care decisions.
Living with Multiple Myeloma: Coping Strategies and Quality of Life
Living with multiple myeloma presents unique challenges that require effective coping strategies to maintain quality of life. Patients often report feelings of uncertainty regarding their prognosis and treatment outcomes; thus, fostering resilience through education about their condition can be empowering. Understanding the nature of multiple myeloma—its chronicity rather than its curability—can help patients adjust their expectations and focus on managing their health proactively.
Establishing a strong support network is crucial for emotional well-being. Engaging with family members, friends, or support groups can provide a sense of community and shared experience that alleviates feelings of isolation. Many patients find solace in connecting with others who are navigating similar challenges; online forums or local support groups can serve as valuable resources for sharing experiences and coping strategies.
Incorporating lifestyle modifications can also enhance quality of life for individuals living with multiple myeloma. Regular physical activity tailored to individual capabilities can help combat fatigue and improve overall physical health. Mindfulness practices such as yoga or meditation may assist in managing stress levels while promoting emotional resilience.
Additionally, maintaining open communication with healthcare providers about any emerging symptoms or concerns ensures timely interventions that can further improve quality of life.
Future Directions in Multiple Myeloma Research
The future landscape of multiple myeloma research holds great promise as scientists continue to unravel the complexities underlying this malignancy. One area garnering significant attention is the exploration of genetic profiling to identify specific mutations or chromosomal abnormalities that may influence treatment responses. By understanding these genetic factors better, researchers aim to develop targeted therapies that can more effectively address individual patient needs.
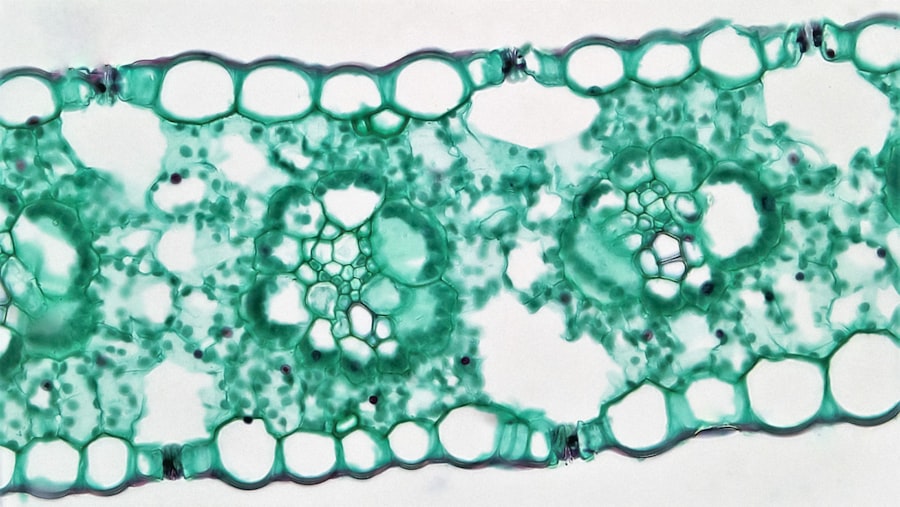
Moreover, ongoing investigations into the role of the bone marrow microenvironment are shedding light on how interactions between malignant plasma cells and surrounding stromal cells contribute to disease progression and treatment resistance. Targeting these interactions may lead to novel therapeutic strategies that enhance treatment efficacy while minimizing toxicity. As clinical trials continue to explore innovative therapies such as CAR T-cell therapy and bispecific antibodies, there is hope for improved outcomes for patients with multiple myeloma who have limited options today.
The integration of precision medicine approaches—tailoring treatments based on individual genetic profiles—will likely become increasingly important in optimizing care for this patient population. In summary, while multiple myeloma remains a challenging disease with significant implications for patients’ lives, ongoing research efforts hold promise for advancing our understanding and management of this complex malignancy. As new therapies emerge and supportive care strategies evolve, there is hope for improved outcomes and enhanced quality of life for those affected by multiple myeloma.