Medical research studies are a cornerstone of modern healthcare, driving advancements in treatment, diagnosis, and prevention. These studies often require the participation of volunteers, and to compensate for their time, effort, and occasional inconvenience, some studies offer financial remuneration. This article explores the landscape of paid medical research studies, outlining their purpose, the participation process, potential benefits, and inherent risks.
Paid medical research studies, often interchangeably referred to as clinical trials or investigational studies, are structured scientific investigations involving human participants. Their primary objective is to evaluate the safety and efficacy of new drugs, medical devices, procedures, or diagnostic tools. These studies are essential for gathering the empirical data needed to bring new medical interventions to market or to refine existing ones. The “paid” aspect of these studies refers to the compensation offered to participants, acknowledging the time commitment and potential discomfort involved. This compensation is distinct from payment for medical services and is typically regulated to prevent undue inducement.
Phases of Clinical Trials
Clinical trials generally adhere to a phased approach, each phase serving a distinct purpose in the development pathway:
- Phase 0: Exploratory, first-in-human trials with very small doses of a drug to investigate pharmacodynamics and pharmacokinetics.
- Phase I: Focuses on safety in a small group of healthy volunteers or patients. Determines optimal dosage and identifies side effects.
- Phase II: Evaluates effectiveness and further assesses safety in a larger group of patients with the target condition.
- Phase III: Compares the new treatment to standard treatments in a large patient population, verifying effectiveness, monitoring side effects, and gathering information for regulatory approval.
- Phase IV: Post-marketing studies conducted after a drug or treatment has been approved and is on the market. Continues to monitor long-term effects and gather additional safety and efficacy data.
Types of Studies
Paid medical research studies encompass a broad spectrum of investigations:
- Drug Trials: Testing the effects of new pharmaceutical compounds.
- Device Trials: Evaluating the safety and efficacy of new medical devices, such as pacemakers or insulin pumps.
- Behavioral Studies: Investigating the impact of lifestyle interventions or psychological therapies.
- Observational Studies: Monitoring participants over time without direct intervention (though these are less likely to be paid).
- Bioavailability/Bioequivalence Studies: Comparing how different formulations of a drug are absorbed and processed by the body.
Navigating the Participant Pathway: How to Get Involved
Becoming a participant in a paid medical research study involves a structured process designed to protect both the participant and the integrity of the research. It begins with identifying suitable studies and culminates in ongoing engagement.
Finding Opportunities
Locating paid medical research studies requires proactive searching:
- ClinicalTrials.gov: A comprehensive database maintained by the U.S. National Library of Medicine. It lists studies conducted worldwide, offering detailed information on eligibility, locations, and contacts.
- Research Institutions and Universities: Many academic medical centers and university hospitals have dedicated clinical research departments or websites advertising ongoing studies.
- Pharmaceutical Companies: Larger pharmaceutical companies often host websites detailing their clinical trial programs.
- Specialized Recruitment Companies: Organizations exist specifically to recruit participants for clinical trials.
- Patient Advocacy Groups: These groups may disseminate information about relevant studies to their communities.
The Screening and Consent Process
Once a potential study is identified, a rigorous screening process ensues:
- Initial Inquiry: Contacting the research coordinator to express interest and provide basic demographic information.
- Pre-Screening: A preliminary assessment, often over the phone, to determine if basic eligibility criteria are met.
- Informed Consent: This is a critical juncture. Participants receive a detailed document outlining the study’s purpose, procedures, potential risks, benefits, alternatives, confidentiality measures, and their rights as a participant. It is not merely a formality but a comprehensive disclosure. You, as the potential participant, are encouraged to ask questions, seek clarification, and take time to consider the implications before signing. Signing indicates voluntary agreement to participate.
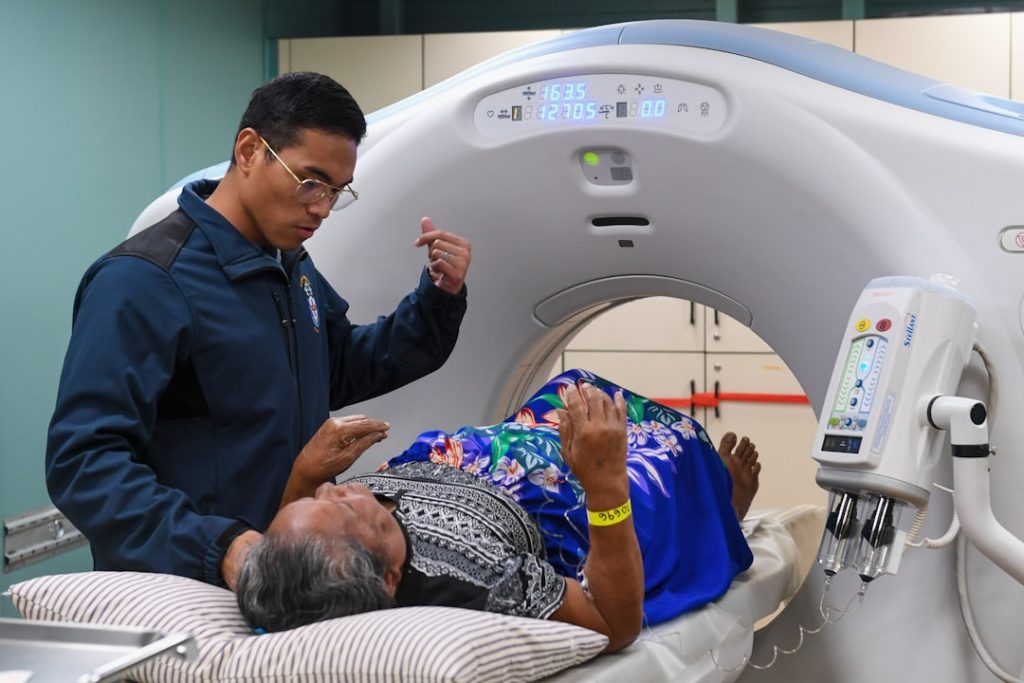
- Medical Screening: A thorough medical evaluation, including physical examinations, blood tests, imaging, and review of medical history, to confirm eligibility and ensure safety for the study procedures. This acts as a gatekeeper, vital for participant protection and data validity.
What to Expect During Participation
Participating in a study demands adherence to the research protocol:
- Scheduled Visits: Regular visits to the research site for check-ups, administration of investigational treatments, data collection, and monitoring of side effects. The frequency and duration of these visits vary widely depending on the study design.
- Adherence to Protocol: Following instructions meticulously, including medication schedules, dietary restrictions, or activity limitations. This ensures the integrity and reliability of the study’s findings. Deviation from the protocol can compromise the data.
- Side Effect Reporting: Promptly reporting any adverse events or unexpected symptoms to the research team. This is paramount for participant safety and allows the research team to intervene if necessary.
- Data Collection: Providing samples (e.g., blood, urine), completing questionnaires, and undergoing various assessments as required by the study protocol.
The Payoff and the Perils: Benefits and Risks of Participation

Participation in paid medical research studies is a two-sided coin, offering potential benefits alongside inherent risks. A clear understanding of both is essential for informed decision-making.
Potential Benefits
While financial compensation is a primary motivator for many, other benefits contribute to the overall value of participation:
- Financial Compensation: This is often the most tangible benefit, compensating for time, travel, and potential inconveniences. The amount varies significantly based on study duration, invasiveness, and required commitment. It is not intended as payment for injury or undue inducement.
- Access to New Treatments: Participants may gain early access to cutting-edge treatments that are not yet available to the general public. For individuals with conditions where standard therapies have failed, this can be a significant draw.
- Close Medical Monitoring: Clinical trial participants often receive more frequent and thorough medical evaluations than they would in routine clinical care. This rigorous oversight can lead to early detection of health issues.
- Contribution to Medical Science: Every participant becomes a vital cog in the machinery of medical discovery. Their data helps to advance understanding, potentially leading to new cures or improved treatments for future generations. This is a profound, altruistic benefit.
- Expert Medical Care: Studies are conducted by highly qualified medical professionals and scientists who specialize in the area of research.
Inherent Risks and Considerations
No medical intervention, even a placebo, is without risk. Participation in a research study carries its own set of potential downsides:
- Adverse Side Effects: Investigational treatments may cause unexpected or severe side effects. While studies are designed to minimize risk, the full spectrum of a new drug’s effects is often unknown. This is the “wild card” of research.
- Ineffectiveness of Treatment: The investigational treatment may not be effective for your condition, or it might even exacerbate it. There is no guarantee of therapeutic benefit. You are, in essence, becoming a data point, not necessarily a recipient of guaranteed improvement.
- Inconvenience and Time Commitment: Studies can be demanding, requiring numerous visits, uncomfortable procedures, and strict adherence to schedules, which can disrupt daily life.
- Placebo Effect: Some studies involve a placebo group, meaning participants may receive an inactive substance instead of the actual treatment. This is crucial for scientific rigor but means there is no therapeutic benefit for those in the placebo arm.
- Loss of Confidentiality (Rare): While robust measures are in place to protect participant privacy, there is always a theoretical, albeit rare, risk of a data breach.
- Opportunity Cost: Engaging in one study may preclude participation in others for a certain period, especially those involving similar interventions.
Ethical Oversights and Participant Rights: Your Shield in the Research Arena
The ethical conduct of medical research is paramount. A comprehensive framework of regulations and oversight bodies exists to protect participants’ rights and welfare. These safeguards act as a bulwark against exploitation and ensure that research is conducted responsibly.
Institutional Review Boards (IRBs)
In the United States, Institutional Review Boards (IRBs) are committees established to review, approve, and monitor biomedical and behavioral research involving human subjects. Their primary mission is to protect the rights and welfare of research participants. An IRB acts as a vigilant guardian, ensuring that:
- Risks are Minimized: The study design minimizes potential harm to participants.
- Risks are Justified: The potential benefits outweigh the risks.
- Informed Consent is Valid: Participants understand the study and voluntarily agree to participate.
- Privacy and Confidentiality are Protected: Measures are in place to safeguard participant data.
- Vulnerable Populations are Protected: Special considerations are given to groups such as children, pregnant women, prisoners, and individuals with impaired decision-making capacity.
Similar ethical review committees exist in other countries under different names (e.g., Research Ethics Committees in the UK).
Participant Rights
Beyond IRB oversight, participants possess fundamental rights within a research study:
- Right to Informed Consent: The right to understand all aspects of the study before agreeing to participate, and to ask questions. This is the cornerstone of ethical research participation.
- Right to Withdraw: The absolute right to withdraw from a study at any time, for any reason, without penalty or loss of benefits to which they would otherwise be entitled. This right underscores the voluntary nature of participation.
- Right to Privacy and Confidentiality: The right to have personal data and medical information protected and kept confidential.
- Right to Safety: The presumption that researchers will take all reasonable steps to ensure participant safety and respond promptly to any adverse events.
- Right to Information: The right to be informed of new findings that might affect their willingness to continue participation.
- Right to Compensation for Injury: In some jurisdictions or specific study types, participants may have a right to compensation if an injury directly results from their participation in the study. This is less common but an important consideration.
Beyond the Individual: The Broader Impact of Paid Research
| Study Type | Average Compensation | Duration | Participant Requirements | Common Conditions Studied |
|---|---|---|---|---|
| Phase 1 Clinical Trials | 1500 – 3000 | 1 – 4 weeks | Healthy adults, 18-45 years | New drug safety and dosage |
| Phase 2 Clinical Trials | 2000 – 5000 | 1 – 6 months | Patients with target condition | Effectiveness and side effects |
| Phase 3 Clinical Trials | 3000 – 7000 | 6 months – 2 years | Large patient groups | Confirm effectiveness, monitor adverse reactions |
| Observational Studies | 500 – 1500 | Varies | Specific demographics or conditions | Long-term health outcomes |
| Behavioral Studies | 100 – 1000 | Hours to weeks | Varies by study | Mental health, lifestyle impacts |
While individual motivations for participating in paid medical studies often center on personal benefit or financial gain, the collective impact of these endeavors extends far beyond the individual participant. Each study, successful or not, contributes to a vast mosaic of scientific knowledge.
Advancing Medical Knowledge
Every clinical trial, regardless of its outcome, adds to humanity’s understanding of disease, physiology, and pharmacology. Even studies that fail to demonstrate efficacy or reveal unexpected side effects provide invaluable data, guiding future research away from unproductive paths and informing the development of superior interventions. This iterative process is the engine of medical progress. Participants are, in a sense, scouts charting unknown territories for the benefit of future generations.
Developing New Therapies
The most direct and celebrated impact of successful clinical trials is the development of new drugs, vaccines, and medical devices. These innovations translate into tangible improvements in patient care, offering new treatment options for previously untreatable conditions, extending life expectancy, and enhancing quality of life. From antibiotics to cancer therapies, from pacemakers to diagnostic imaging, every medical breakthrough has its roots in human research participation.
Informing Public Health Policy
Research findings from clinical trials frequently inform public health policies and guidelines. For example, studies on vaccine efficacy directly influence immunization schedules, while research on lifestyle interventions can shape recommendations for diet and exercise. Participants in these studies contribute directly to healthier populations and more informed public health strategies. Their data, like bricks in a wall, build up robust recommendations for society.
Economic and Societal Benefits
The medical research industry is a significant economic driver, creating jobs for scientists, clinicians, support staff, and a wide array of associated professionals. Furthermore, the global health improvements stemming from research lead to a more productive workforce, reduced healthcare costs in the long run (through prevention and more effective treatments), and overall societal well-being. The financial compensation received by participants can also provide a short-term economic benefit to individuals.
In conclusion, participation in paid medical research studies is a layered decision. It offers financial compensation and potential access to emerging treatments, but it also carries inherent risks and demands a significant commitment. Understanding the rigorous ethical safeguards, the informed consent process, and one’s rights as a participant is crucial. For those who choose to participate, they become vital contributors to the ongoing advancement of medical science, their individual involvement serving as a thread in the intricate tapestry of human health and discovery.