Wikipedia, as a neutral and objective source of information, provides factual content without hyperbolic language or excessive adjectives. This article adheres to those guidelines, serving as a comprehensive resource for individuals seeking clinical trials. It aims to inform rather than persuade, presenting information in a clear, concise, and structured manner.
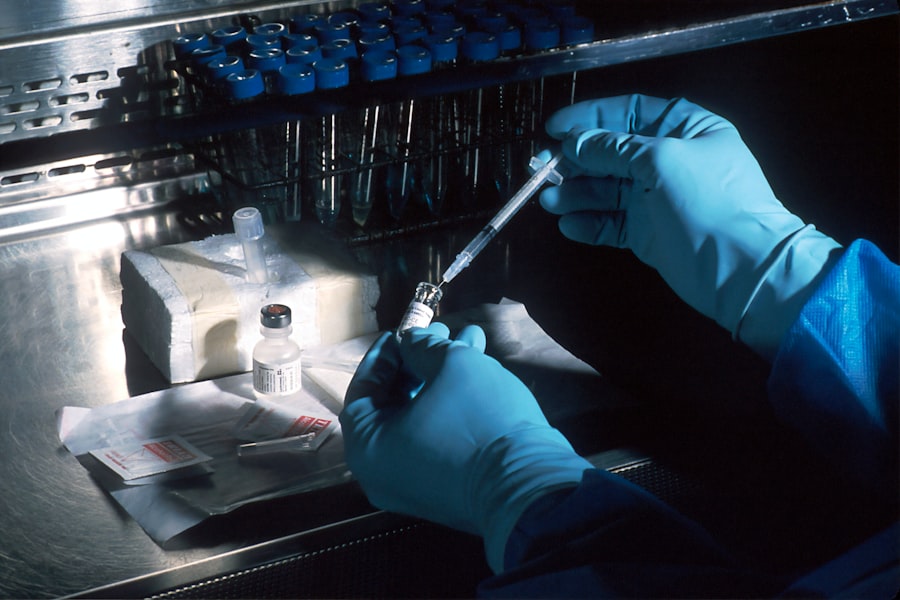
Clinical trials are research studies performed in people that evaluate a medical, surgical, or behavioral intervention. They are the primary way that researchers determine if a new treatment, such as a new drug, diet, or medical device, is safe and effective in humans. Before a new intervention can become widely available, it must undergo a rigorous testing process through various phases of clinical trials. This methodical approach ensures that potential treatments are thoroughly vetted for both efficacy and safety.
The Purpose of Clinical Trials
The overarching goal of clinical trials is to advance medical knowledge and improve healthcare for future generations. For many individuals facing challenging health conditions, participating in a clinical trial offers an opportunity to access cutting-edge treatments that are not yet widely available. For researchers, these trials are crucial for gathering data, testing hypotheses, and ultimately bringing new therapies to light. The data collected from clinical trials informs regulatory bodies, such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA), in their decisions regarding the approval of new treatments.
Phases of Clinical Trials
Clinical trials typically progress through a series of phases, each designed to answer specific questions and evaluate different aspects of the intervention.
Phase 0: Exploratory Trials
Phase 0 trials are an exploratory stage, often involving a very small number of participants and a minimal dose of the investigational drug. The primary aim is to understand how the drug is absorbed, metabolized, and excreted by the body, offering early insights into its pharmacokinetic properties. These trials do not assess efficacy.
Phase I: Safety and Dosage
Phase I trials typically involve a small group of healthy volunteers or patients with the condition. The main objective is to assess the safety of a new drug or treatment, determine a safe dosage range, and identify potential side effects. Researchers carefully monitor participants for adverse reactions.
Phase II: Efficacy and Further Safety
In Phase II, the experimental drug or treatment is administered to a larger group of patients (typically dozens to a few hundred) who have the condition. The focus shifts to evaluating the treatment’s effectiveness, while continuing to monitor safety. This phase helps determine if the intervention has a beneficial effect and at what dose.
Phase III: Confirmation and Comparison
Phase III trials involve a large number of participants (hundreds to thousands) and are designed to confirm the effectiveness of the new treatment, monitor side effects, compare it to commonly used treatments, and collect information that will allow the treatment to be used safely. Successful completion of Phase III is often required for regulatory approval.
Phase IV: Post-Marketing Surveillance
After a drug is approved and marketed, Phase IV trials continue to monitor its long-term effects and safety in a broader population. These studies can reveal rare side effects or long-term benefits that may not have been apparent in earlier phases. They are essential for understanding the full impact of a treatment over time.
Benefits and Risks of Participation
Deciding whether to participate in a clinical trial is a significant personal choice that requires careful consideration of both potential benefits and inherent risks. It is akin to navigating a new path; while it might lead to a desired destination, the journey could present unforeseen challenges.
Potential Benefits
Participants in clinical trials may gain early access to new treatments that are not yet available to the general public. This can be particularly appealing for individuals with conditions for which existing therapies are ineffective or limited. Furthermore, participants receive regular and often comprehensive medical care from a research team, including close monitoring and access to specialists. This level of attention can be a significant advantage. Contributing to medical science is another crucial benefit; by participating, individuals play a direct role in advancing scientific knowledge and potentially helping countless others in the future. Their contribution is a vital link in the chain of medical progress.
Potential Risks
While participating in a clinical trial can offer significant advantages, it is important to acknowledge the associated risks. The investigational treatment may not be effective, or it could even prove less effective than standard care. There is also the possibility of experiencing unexpected or severe side effects, as the long-term effects of many new treatments are still being studied. The time commitment required for trial participation can be substantial, involving frequent clinic visits, tests, and procedures. Additionally, participants might incur some personal costs, such as travel expenses or missed work, although many trials offer stipends to offset these. It is crucial to remember that the placebo effect, where participants improve simply because they believe they are receiving treatment, can sometimes mask the true effectiveness of an intervention. Moreover, the trial design itself, such as randomization or blinding, can impact a participant’s experience.
Finding Clinical Trials

Locating suitable clinical trials requires a systematic approach. Several resources, both online and offline, can assist individuals in their search. Understanding these avenues can help streamline the process.
Online Databases and Registries
The internet serves as a primary repository for clinical trial information. Dedicated databases and registries collate details on active and recruiting studies globally.
ClinicalTrials.gov
ClinicalTrials.gov, maintained by the U.S. National Library of Medicine (NLM) at the National Institutes of Health (NIH), is a comprehensive database of publicly and privately funded clinical studies conducted around the world. It provides information on study purpose, participant eligibility criteria, locations, and contact information. Users can search by condition, intervention, location, or study ID. This resource is a cornerstone for anyone seeking clinical trial opportunities. Its user interface is designed for accessibility, allowing individuals to filter results based on their specific needs.
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP)
The ICTRP provides a single point of access to information about clinical trials from around the world. It aims to ensure that a complete picture of research is available for all stakeholders, enhancing transparency and public accountability. The ICTRP works by linking to various primary registries, offering a broader scope than individual national databases. This platform is a valuable tool for those seeking international trial opportunities or a comprehensive global perspective.
European Union Clinical Trials Register
For individuals within the European Union, the European Union Clinical Trials Register offers information on interventional clinical trials conducted in the EU. This registry includes details such as trial design, objectives, inclusion/exclusion criteria, and results once available. It operates under the European Medicines Agency (EMA) and provides a regulatory-compliant framework for listing clinical studies within the EU.
Disease-Specific Organizations
Many non-profit organizations dedicated to specific diseases or conditions maintain their own databases or lists of relevant clinical trials. These organizations often provide curated information, patient support, and resources tailored to their community. Examples include the American Cancer Society, the Alzheimer’s Association, and the Multiple Sclerosis Society. These resources can be particularly helpful as they often provide a more personalized approach and can connect individuals with advocacy groups.
Consulting Healthcare Professionals
Your primary care physician or a specialist can be an invaluable resource in identifying relevant clinical trials. They possess an understanding of your medical history and can offer guidance tailored to your specific situation.
Primary Care Physician (PCP)
Your PCP has a comprehensive understanding of your medical history and current health status. They can assess whether participating in a clinical trial aligns with your overall care plan and help you understand the potential implications. They can also connect you with specialists or research centers. Their knowledge acts as a first filter, ensuring that initial considerations align with your broader health management.
Specialists
If you have a particular medical condition, a specialist in that field (e.g., oncologist, neurologist, cardiologist) is more likely to be aware of ongoing clinical trials specifically relevant to your disease. Specialists are often directly involved in research or are part of networks that participate in clinical studies. They can provide expert advice on the scientific merits and potential risks of a trial. These individuals are often at the forefront of medical advancement in their respective fields.
Research Institutions and Hospitals
Academic medical centers and large research hospitals are frequently involved in conducting clinical trials. These institutions often have dedicated research departments or clinical trial offices that can provide information.
University Hospitals and Academic Medical Centers
These institutions are often at the forefront of medical research and frequently host a wide array of clinical trials across various specialties. Many have dedicated websites or departments specifically for clinical research, offering searchable databases or contact information for trial coordinators. They are centers of innovation and often have the resources to conduct complex studies.
Dedicated Clinical Research Sites
Independent clinical research sites, distinct from large university settings, also conduct numerous trials. These sites often specialize in specific therapeutic areas and can be a good option for finding trials focused on a particular condition. They may advertise their studies through local media or online platforms.
Preparing for Participation
Once you have identified a potential clinical trial, a series of steps are necessary to prepare for participation. This phase involves a detailed review of information and open communication with the research team.
Informed Consent Process
Informed consent is a fundamental ethical principle in clinical research. Before you can participate in a trial, you will be provided with a comprehensive document detailing the study’s purpose, procedures, potential risks and benefits, and your rights as a participant.
Understanding the Informed Consent Document
This document is often extensive and can be complex. Take the time to read it thoroughly. It outlines every aspect of the trial, including the experimental treatment, placebo usage (if applicable), frequency of visits, tests, and potential side effects. Do not hesitate to ask questions about anything you do not understand. The research team is obligated to provide clear explanations. This document serves as your guide, a map of the landscape you are about to explore.
Asking Questions
It is imperative to ask questions. Consider preparing a list of questions in advance. Examples include: What are the potential side effects? How will this trial affect my daily life? What are my alternatives to participating in this trial? Who will pay for the treatment and associated medical care? What happens if I decide to withdraw from the study? Open dialogue is crucial for ensuring you are fully informed.
Eligibility Criteria
Each clinical trial has specific eligibility criteria that participants must meet to ensure the study is appropriate for them and to maintain the scientific integrity of the research. These criteria often include age, gender, type and stage of disease, previous treatments, and other medical conditions.
Inclusion Criteria
These are the characteristics that an individual must possess to be eligible for a particular trial. For example, a trial might require participants to be within a certain age range, have a specific diagnosis, or have responded in a certain way to previous treatments. These are the gates that must be open for you to enter.
Exclusion Criteria
Conversely, exclusion criteria are characteristics that would prevent an individual from participating. Examples include pre-existing medical conditions that could interfere with the study, certain medications, or pregnancy. These are the gates that must remain closed. Meeting both sets of criteria is essential for safe and effective trial participation.
Communication with the Research Team
Maintaining open and honest communication with the research team is paramount throughout your participation in a clinical trial. This relationship is a partnership in which both parties have responsibilities.
Role of the Principal Investigator (PI)
The Principal Investigator is the lead researcher responsible for the overall conduct of the trial. They oversee the design, execution, and reporting of the study, and are the ultimate authority on medical decisions within the trial. You should feel comfortable addressing any medical concerns or questions to them or their delegated medical staff. The PI is the conductor of this scientific orchestra.
Study Coordinators and Nurses
Study coordinators and nurses are often your primary points of contact for day-to-day questions, scheduling, and logistical concerns. They are instrumental in explaining study procedures, collecting data, and ensuring your comfort and safety. They are the navigators, guiding you through the process. Do not hesitate to communicate any changes in your health or well-being to them promptly. This ongoing dialogue ensures that any issues are addressed in a timely manner and that your participation is as safe and beneficial as possible.
Ethical Considerations and Patient Rights
| Metric | Description | Example Data |
|---|---|---|
| Number of Active Trials | Total clinical trials currently recruiting or ongoing in your area | 45 |
| Trial Phases | Distribution of clinical trials by phase (I, II, III, IV) | Phase I: 10, Phase II: 15, Phase III: 12, Phase IV: 8 |
| Therapeutic Areas | Common medical conditions targeted by trials near you | Cancer, Diabetes, Cardiovascular, Neurology |
| Average Enrollment Size | Average number of participants per trial | 120 participants |
| Average Trial Duration | Typical length of clinical trials in months | 18 months |
| Top Research Institutions | Leading hospitals or centers conducting trials near you | City Medical Center, Regional Research Institute |
| Participant Eligibility | Common inclusion criteria for trials | Age 18-65, Specific diagnosis, No prior treatment |
Clinical trials are governed by strict ethical guidelines and regulations to protect the rights, safety, and well-being of participants. These safeguards are the bedrock of responsible medical research.
Institutional Review Boards (IRBs) / Ethics Committees (ECs)
Before a clinical trial can begin, its protocol must be reviewed and approved by an Institutional Review Board (IRB) in the United States or an Ethics Committee (EC) elsewhere. These independent committees are composed of scientists, medical professionals, and community members.
Role in Participant Protection
The primary role of IRBs/ECs is to protect the rights and welfare of human research participants. They meticulously review all aspects of the proposed study, including its scientific merit, ethical considerations, and the informed consent process. They ensure that the potential benefits outweigh the risks and that participants are not coerced into joining a study. Their approval is a vital step, acting as a quality control mechanism for ethical research.
Continuous Oversight
IRBs/ECs do not merely approve a study at its outset; they provide ongoing oversight throughout the trial. They review any amendments to the protocol, adverse events, and interim results to ensure that participant safety remains paramount. This continuous scrutiny ensures that the ethical compass of the trial remains correctly oriented.
Patient Rights
Participants in clinical trials have specific rights that are legally and ethically protected. Understanding these rights empowers individuals to make informed decisions and advocate for themselves.
Right to Withdraw
You have the unqualified right to withdraw from a clinical trial at any time, for any reason, without penalty or loss of benefits. This right is fundamental to ethical research, acknowledging your autonomy over your medical care. Your decision to withdraw will not affect your relationship with your doctor or access to standard medical care.
Confidentiality and Privacy
Your personal and medical information collected during a clinical trial is treated with strict confidentiality. Researchers are bound by privacy laws and ethical standards to protect your identity and data. While results may be published, your individual identity will not be revealed. This commitment to privacy is essential, safeguarding your personal boundaries and trust.
Access to Information
You have the right to be fully informed about all aspects of the trial, including its purpose, procedures, potential risks and benefits, and any new information that arises during the study. This includes the right to ask questions and receive clear, understandable answers. Transparent communication is a cornerstone of your participation.



