Finding Health Trials Near Me: A Guide to Clinical Research Participation
Participating in clinical trials offers individuals the opportunity to contribute to medical advancements while potentially gaining access to innovative treatments and close medical monitoring. This guide outlines methods for locating health trials, understanding their nature, and preparing for participation, all within a localized context.
Clinical trials are research studies conducted in human volunteers to evaluate new ways to prevent, detect, treat, or manage various diseases and health conditions. They are a critical step in the development of new medications, therapies, and medical devices. Each trial adheres to a meticulously designed protocol to ensure scientific rigor and participant safety.
Phases of Clinical Trials
Clinical trials typically progress through several phases, each with a distinct objective:
- Phase 0 Trials: Exploratory studies often involving very small doses of a drug in a few people to learn how the drug is absorbed and metabolized.
- Phase I Trials: Focus on safety and dosage. These trials involve a small group of healthy volunteers or patients to determine the drug’s safety, side effects, and optimal dosage.
- Phase II Trials: Evaluate effectiveness and further assess safety. A larger group of volunteers with the condition being studied receives the treatment to determine its efficacy and continue monitoring for adverse effects.
- Phase III Trials: Confirm effectiveness, monitor side effects, compare to standard treatments. These are large-scale studies involving hundreds or thousands of participants, often comparing the new treatment to existing therapies. This phase is crucial for regulatory approval.
- Phase IV Trials: Post-marketing studies. After a drug is approved and available to the public, Phase IV trials continue to monitor its long-term effects, optimal use, and safety in a broader population.
Types of Clinical Trials
Clinical trials encompass various research designs, addressing different medical needs:
- Treatment Trials: Test experimental treatments, new combinations of drugs, or new approaches to surgery or radiation therapy.
- Prevention Trials: Look for better ways to prevent disease in people who have never had the disease or to prevent the disease from returning. These approaches may include medicines, vaccines, vitamins, minerals, or lifestyle changes.
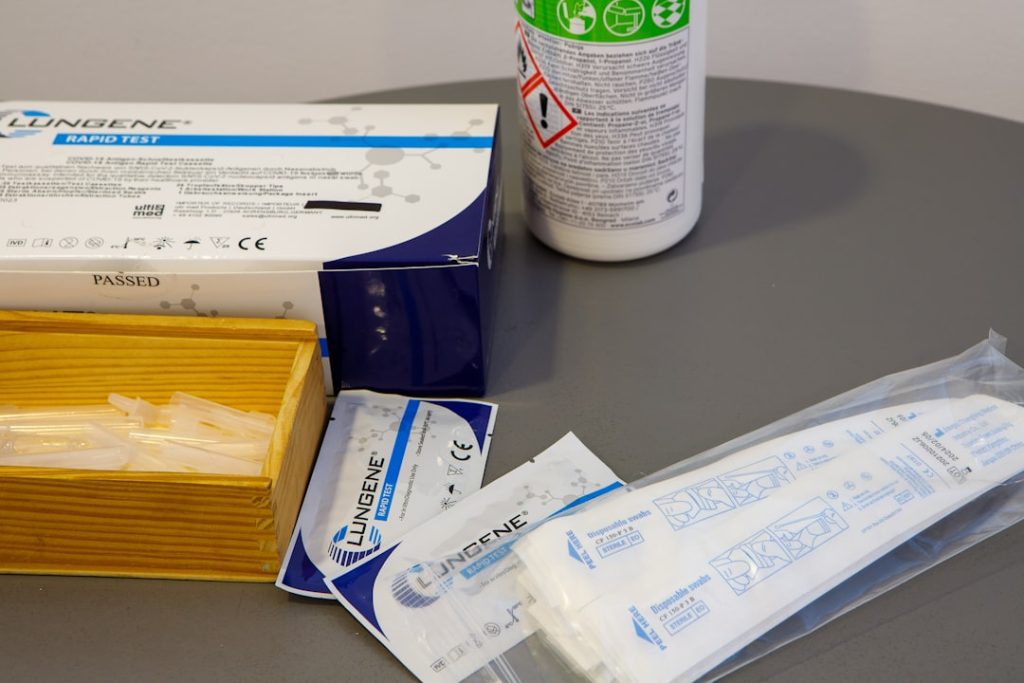
- Diagnostic Trials: Study new ways to identify diseases or health conditions.
- Screening Trials: Test the best ways to detect certain diseases or health conditions.
- Quality of Life Trials (Supportive Care Trials): Explore ways to improve comfort and the quality of life for people with chronic illnesses.
Locating Trials Online
The internet serves as a primary conduit for identifying clinical trials. Several reputable online databases function as central repositories, allowing individuals to search for studies based on various criteria.
Government Databases
Government agencies often maintain comprehensive databases of ongoing and upcoming clinical trials. These resources are typically robust and regularly updated.
- ClinicalTrials.gov: Operated by the U.S. National Library of Medicine, ClinicalTrials.gov is a widely used and authoritative resource. It contains information on trials conducted globally, allowing searches by condition, drug name, location, and sponsor. The platform provides detailed descriptions of each trial, including eligibility criteria, study design, and contact information for researchers.
- European Clinical Trials Register (EU CTR): For individuals in Europe, the EU CTR (previously the EudraCT database for trials covered by the Clinical Trials Directive) provides access to information on clinical trials conducted within the European Union and the European Economic Area. It focuses on trials involving medicinal products.
Non-Profit and Advocacy Organization Websites
Many non-profit organizations and disease-specific advocacy groups dedicate resources to assisting their communities in finding clinical trials. These organizations often have a deep understanding of specific conditions and can provide targeted information.
- Disease-Specific Foundations: Foundations focused on conditions such as cancer, Alzheimer’s disease, diabetes, or rare diseases frequently list relevant trials on their websites. These listings are often curated and may include trials not immediately visible on broader government databases. For example, the Alzheimer’s Association maintains a trial matching service.
- Patient Advocacy Groups: These groups offer support and information for patients and their families. Many provide educational resources on clinical trials and directories of ongoing studies relevant to their specific patient population.
Pharmaceutical Company Websites
Pharmaceutical and biotechnology companies conducting trials often list them on their corporate websites. While these listings typically focus on trials sponsored by that particular company, they can be a relevant source for specific drug development.
- Direct Company Search: If a particular pharmaceutical company is known to be developing treatments for a specific condition, visiting their corporate research and development section may reveal ongoing trials.
Local Search Strategies
While online databases offer a broad overview, local search strategies can refine the results, bringing the search closer to home. The “near me” aspect of finding trials often involves connecting with local medical institutions and healthcare providers.
University Medical Centers and Hospitals
Academic medical centers and large hospitals are often at the forefront of clinical research. They conduct a significant number of trials across various specialties.
- Research Departments: Most university medical centers have dedicated research departments or clinical trial offices. These offices can provide information on studies being conducted within their institution. Websites of these institutions often feature a “clinical trials” or “research” section.
- Doctor Referrals: Primary care physicians and specialists often have knowledge of ongoing trials within their professional networks or at affiliate institutions. A doctor can act as a crucial link, bridging the gap between national databases and local opportunities. Discussing trial participation with a healthcare provider is an essential step.
Specialized Clinics and Research Networks
Certain clinics or research networks specialize in particular diseases or medical disciplines. These entities are frequent participants in clinical trials.
- Condition-Specific Clinics: Clinics focusing on areas like cardiology, oncology, neurology, or infectious diseases are more likely to be involved in relevant clinical research. Direct contact with these clinics can yield information on local opportunities.
- Research Site Networks: Some organizations exist solely to manage and recruit for clinical trials across multiple locations. While these are often contract research organizations (CROs) working on behalf of pharmaceutical companies, they may have public-facing portals or offices that individuals can contact.
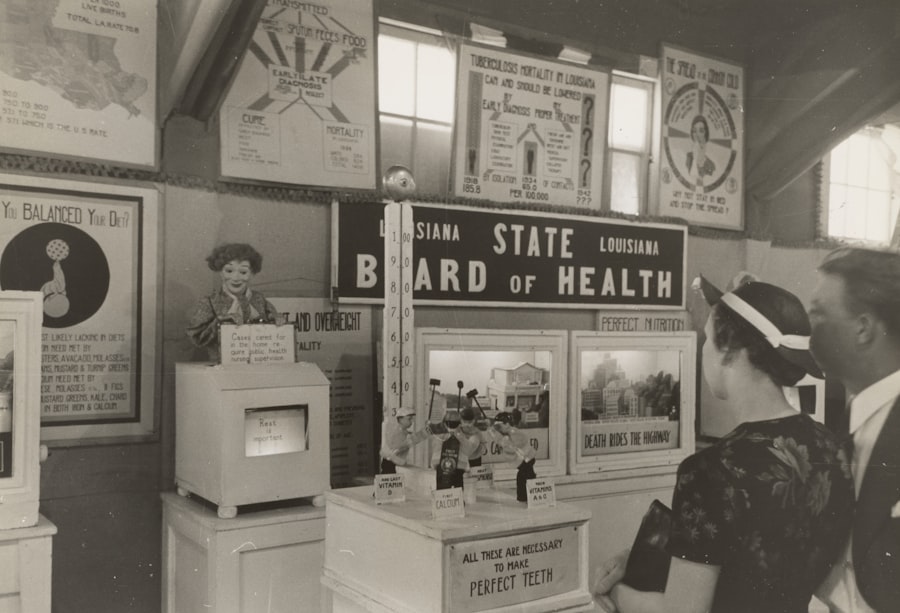
Community Outreach and Advertising
Clinical trial recruitment campaigns often extend beyond traditional medical settings into community spaces and local media.
- Local Advertisements: Trials may be advertised in local newspapers, community centers, radio, or even targeted online ads based on geographic location. These advertisements typically provide a clear call to action and contact information.
- Health Fairs and Events: Participating in local health fairs or community health events can provide opportunities to speak directly with research coordinators or representatives from trial sites.
Preparing for Participation

Once potential trials have been identified, preparing for participation involves understanding the commitment, assessing personal suitability, and engaging in informed decision-making.
Eligibility Criteria
Every clinical trial has specific inclusion and exclusion criteria that determine who can participate. These criteria are designed to ensure the safety of participants and the scientific integrity of the study.
- Inclusion Criteria: Factors that allow someone to participate in a trial, such as age, gender, type and stage of disease, previous treatment history, or other medical conditions.
- Exclusion Criteria: Factors that prevent someone from participating, such as certain medical conditions, medications, or pregnancy.
- Initial Screening: A preliminary assessment, often over the phone or through an online questionnaire, determines if an individual meets the basic criteria.
Informed Consent
Informed consent is a cornerstone of ethical clinical research. It is a process that ensures potential participants understand the full scope of the trial before committing.
- Information Provision: Researchers provide a detailed document explaining the trial’s purpose, procedures, potential risks and benefits, alternatives to participation, and the right to withdraw at any time.
- Discussion and Questions: Participants have the opportunity to ask questions and discuss the trial with the research team. This dialogue is crucial for clarifying any uncertainties.
- Voluntary Agreement: Participation is entirely voluntary. Signing the informed consent document signifies understanding and agreement, but does not waive any legal rights or obligate continued participation.
Questions to Ask the Research Team
Engaging actively with the research team is paramount. Asking pertinent questions can clarify aspects of the trial and ensure a well-informed decision.
- Trial Specifics: “What is the purpose of this study?” “What are the specific procedures I will undergo?” “How long will the trial last, and how many visits are required?”
- Potential Risks and Benefits: “What are the potential risks and side effects of the treatment?” “What are the potential benefits of participating in this trial?” “Are there alternative treatments available?”
- Logistics and Costs: “Will I be reimbursed for travel or other expenses?” “Will my insurance cover any costs associated with the trial?” “Who will be responsible for my medical care during the trial?”
- Ethical Considerations: “How will my privacy be protected?” “Who do I contact if I have questions or concerns during the trial?”
The Experience of Participation
| Trial Name | Location | Condition | Phase | Enrollment Status | Contact |
|---|---|---|---|---|---|
| Diabetes Management Study | New York, NY | Type 2 Diabetes | Phase 3 | Recruiting | info@diabetesstudy.org |
| Hypertension Medication Trial | Chicago, IL | High Blood Pressure | Phase 2 | Recruiting | contact@htntrial.com |
| Asthma Treatment Research | Los Angeles, CA | Asthma | Phase 1 | Not Recruiting | asthma@researchcenter.org |
| COVID-19 Vaccine Study | Houston, TX | COVID-19 | Phase 4 | Recruiting | covidstudy@healthcenter.net |
| Alzheimer’s Disease Trial | Boston, MA | Alzheimer’s Disease | Phase 3 | Recruiting | alzheimers@clinicaltrials.org |
Participating in a clinical trial is a journey. It often involves regular visits to the research site, adherence to a study protocol, and meticulous data collection.
Commitment and Responsibilities
Participants in clinical trials undertake specific responsibilities, which are vital for the trial’s success.
- Adherence to Protocol: Following the instructions for medication, appointments, and procedures as outlined in the study protocol.
- Open Communication: Reporting any new symptoms, side effects, or changes in health status to the research team promptly.
- Record Keeping: Maintaining accurate records of medication intake or symptom diaries as requested by the study.
Medical Oversight and Safety
While trials focus on new treatments, participant safety is a paramount concern and is monitored by multiple layers of oversight.
- Institutional Review Boards (IRBs) / Ethics Committees (ECs): Independent committees that review and approve research protocols to protect the rights and welfare of human participants. They continue to monitor trials throughout their duration.
- Data and Safety Monitoring Boards (DSMBs): Independent groups of experts who periodically review accumulating data from ongoing trials to ensure participant safety and scientific validity. They can recommend stopping a trial if safety concerns arise or if a treatment shows overwhelming efficacy or futility.
- Regular Monitoring: Study staff closely monitor participants for any adverse events and provide necessary medical care during the trial.
Potential Outcomes
The outcome of a clinical trial is not always guaranteed. Participants enter with the understanding that the new treatment may or may not be effective.
- Effective Treatment: The investigational treatment may prove beneficial, potentially leading to an improved condition or quality of life.
- No Benefit or Negative Effects: The treatment may not be effective or could produce side effects. In such cases, participants receive appropriate medical management and may be guided to alternative care.
- Contribution to Science: Regardless of individual outcome, participation always contributes to a broader understanding of diseases and potential treatments, acting as a crucial step in the advancement of medical knowledge. Even a trial that shows no benefit or negative effects provides valuable information.
Participating in a clinical trial is a deliberate decision, providing an opportunity to contribute directly to the tapestry of medical progress. It is a conduit to potentially new therapies and an important avenue for individuals seeking advanced or alternative treatment options, particularly when standard approaches have been exhausted.