Improving Medical Room Efficiency Through Research and Administration
Medical room efficiency is a critical determinant of healthcare quality, patient satisfaction, and operational sustainability. It encompasses the streamlined execution of clinical processes within a medical facility’s examination, treatment, or procedure rooms. Inefficient room utilization can lead to extended patient wait times, increased operational costs, and reduced capacity for patient care. This article examines the multifaceted approaches to enhancing medical room efficiency, emphasizing the roles of rigorous research and robust administrative strategies.
Before implementing any improvement initiatives, a comprehensive understanding of the current state is indispensable. This involves a critical evaluation of existing workflows, resource allocation, and patient flow dynamics within the medical room environment. Without this foundational analysis, proposed solutions risk being misdirected or ineffective, akin to trying to fix a complex machine without first understanding its current operational faults.
Workflow Analysis and Mapping
Workflow analysis involves a detailed examination of each step a patient, clinician, or material takes within the medical room. This typically includes:
- Process flowcharts: Visual representations illustrating the sequence of activities, decision points, and actors involved in a specific medical room process. For example, charting the journey of a patient from check-in, through vital sign collection, physician consultation, and discharge.
- Time-motion studies: Direct observation and timing of tasks performed by healthcare staff. This quantitative data reveals bottlenecks, identifies delays, and quantifies the time spent on value-added versus non-value-added activities.
- Value stream mapping: A lean methodology visualizing the entire process from the patient’s perspective, highlighting areas of waste (e.g., waiting, unnecessary movement, over-processing).
Resource Utilization Assessment
An inefficient medical room often suffers from misaligned resource allocation. This assessment specifically examines:
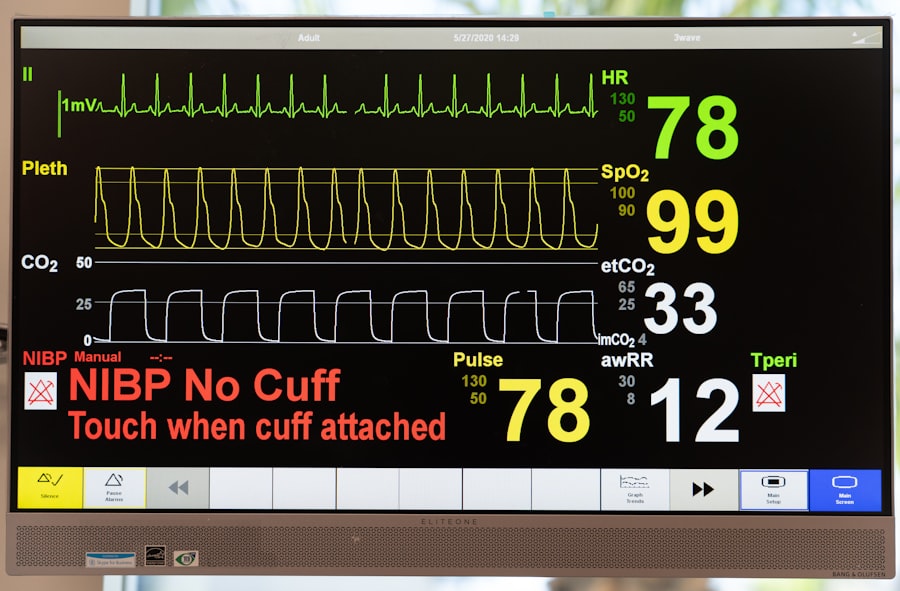
- Equipment utilization rates: Tracking how often diagnostic equipment (e.g., ultrasound machines, endoscopes) or treatment devices are in use versus idle. Equipment lying dormant represents a capital expense not generating returns.
- Staff allocation patterns: Analyzing the distribution of clinical and administrative staff across different rooms and times. Is there an optimal nurse-to-room ratio? Are support staff adequately deployed to prepare rooms or manage patient transitions?
- Supplies and inventory management: Evaluation of how medical supplies are stocked, organized, and accessed within each room. Poor inventory management can lead to time wasted searching for items or delays due to stockouts.
Patient Flow Metrics
Understanding how patients move through the system is central to efficiency. Key metrics include:
- Patient wait times: The duration from arrival to room entry, and from room entry to physician interaction.
- Room turnover time: The time elapsed from one patient’s departure to the next patient’s entry into the same room. This is a direct measure of room readiness.
- Length of stay in room: The total time a patient occupies a medical room for a specific encounter.
Research-Driven Optimization Strategies
Rigorous research provides the evidence base for effective interventions. This involves employing scientific methodologies to test hypotheses, analyze data, and derive actionable insights that can be translated into practical improvements.
Time-and-Motion Studies for Process Re-engineering
Advanced time-and-motion studies, often augmented by video analysis and statistical modeling, can pinpoint subtle inefficiencies that are not apparent through casual observation. For example, research might reveal that nurses spend an aggregate of 30 minutes per shift searching for specific medical instruments due to disorganized supply carts. This data then justifies the re-design of supply layouts or the implementation of standardized cart configurations.
Simulation Modeling and Discrete Event Simulation (DES)
Simulation software allows healthcare administrators to model various scenarios without disrupting actual operations. DES, in particular, can simulate the movement of patients, staff, and resources through a medical facility. Researchers can use DES to:
- Test staffing models: Evaluate the impact of adding or reallocating nurses, medical assistants, or physicians on wait times and room utilization.
- Optimize room allocation: Determine the ideal number of rooms required for specific specialties or procedure types given projected patient volumes.
- Assess technological interventions: Model the effect of new technologies (e.g., electronic patient tracking systems, automated dispensing cabinets) on throughput.
Ergonomics and Human Factors Research
Designing medical rooms with human factors in mind can significantly reduce physical strain on staff, minimize errors, and improve workflow. Research in this area investigates:
- Optimal equipment placement: How accessible are frequently used instruments or controls?
- Lighting and acoustics: Do these environmental factors contribute to staff fatigue or patient discomfort?
- Room layout for specific procedures: Is the layout conducive to sterile technique, patient privacy, or team collaboration during complex procedures? Studies might involve tracking eye movements or physical movements of staff during simulated procedures to identify design flaws.
Administrative Excellence: Implementing and Sustaining Improvements

Research provides the “what” and “why,” but administrative excellence provides the “how.” Effective administration translates research findings into practical changes, ensures their successful implementation, and fosters a culture of continuous improvement.
Standardized Workflows and Protocols
Standardization reduces variability, diminishes errors, and improves predictability. This involves:
- Developing clear protocols for room setup and turnover: Checklists ensure all necessary equipment is present and rooms are cleaned efficiently between patients.
- Implementing standardized patient intake and discharge procedures: This ensures a consistent approach, minimizes administrative burden, and prevents delays.
- Creating “playbooks” for common procedures: These documents outline optimal steps, equipment, and staff roles for frequent medical encounters, promoting consistency and reducing reliance on individual memory.
Technology Integration and Digital Solutions
Leveraging technology can automate tasks, improve communication, and provide real-time data for decision-making.
- Electronic Health Records (EHRs): While EHR implementation itself can be complex, optimized EHR usage can streamline documentation, order entry, and access to patient information within the room.
- Real-time locating systems (RTLS): Using RFID tags or similar technologies, RTLS can track the location of equipment, staff, and even patients, providing insights into bottlenecks and resource availability.
- Patient portal integration: Allowing patients to complete pre-visit paperwork online reduces administrative time spent in the room and improves data accuracy.
- Digital signage and communication boards: Displaying wait times, room assignments, and patient flow updates can reduce patient anxiety and streamline transitions.
Staff Training and Empowerment
Front-line staff are often the best sources of insights into operational inefficiencies. Empowering them and providing adequate training is crucial.
- Cross-training staff: Enabling nurses or medical assistants to perform a wider range of tasks (e.g., basic equipment troubleshooting, room preparation for multiple specialties) improves flexibility.
- Regular training on new protocols and technologies: Ensuring staff are proficient in using new systems or adhering to updated workflows.
- Establishing feedback mechanisms: Creating avenues for staff to report issues, suggest improvements, and participate in process re-design. This could involve regular meetings, suggestion boxes, or dedicated improvement committees.
Data-Driven Performance Monitoring
The journey to sustained efficiency requires constant vigilance and adaptation. This necessitates a robust system for monitoring key performance indicators (KPIs) and using that data to inform ongoing improvements.
Key Performance Indicators (KPIs) for Room Efficiency
Monitoring relevant KPIs provides objective insights into the effectiveness of implemented strategies. These may include:
- Average room turnover time: A direct measure of the speed at which rooms are prepared for the next patient.
- Patient throughput per room (per day/hour): The number of patients seen in a given room over a defined period.
- Patient wait times (various stages): Tracking delays at different points in the patient journey.
- Staff overtime hours directly attributable to inefficiencies: An indicator of workload imbalance or process breakdowns.
- Patient satisfaction scores related to wait times and overall experience: A qualitative measure that reflects the impact of efficiency on the patient.
Regular Audits and Benchmarking
Periodic audits assess adherence to new protocols and identify deviations. Benchmarking involves comparing performance metrics against internal historical data, industry best practices, or other similar facilities. This external perspective can highlight areas where further improvement is possible. For example, if a facility’s room turnover time is consistently higher than national averages for similar specialties, it signals a need for further investigation and corrective action.
Continuous Quality Improvement (CQI) Cycles
Medical room efficiency is not a static state but an ongoing process. Implementing CQI methodologies such as Plan-Do-Study-Act (PDSA) cycles allows for iterative improvement.
- Plan: Identify a problem, propose a solution, and define success metrics.
- Do: Implement the solution on a small scale.
- Study: Analyze the results against the success metrics.
- Act: Standardize the successful change, or refine the solution and repeat the cycle if unsuccessful.
This cyclical approach ensures that improvements are not one-off events but are systematically integrated and continually refined based on observed outcomes.
Conclusion
| Metric | Description | Value | Unit | Notes |
|---|---|---|---|---|
| Number of Research Studies | Total ongoing research projects in the medical room | 12 | Studies | Includes clinical trials and observational studies |
| Patient Visits per Month | Average number of patients visiting the medical room monthly | 150 | Visits | Includes both research participants and general patients |
| Staff Members | Number of administrative and medical staff assigned | 8 | People | Includes researchers, nurses, and admin personnel |
| Equipment Utilization Rate | Percentage of time medical equipment is in use | 75 | % | Measured monthly |
| Average Response Time | Time taken to respond to patient inquiries or emergencies | 5 | Minutes | Target is under 10 minutes |
| Research Funding Allocated | Budget allocated for research activities in the medical room | 120000 | Units | Annual budget |
| Compliance Rate | Adherence to medical and research regulations | 98 | % | Based on recent audits |
Improving medical room efficiency is a complex undertaking that requires a multifaceted approach, drawing equally from rigorous research and astute administration. By systematically analyzing current operations, leveraging research methodologies like time-motion studies and simulation, and implementing administrative strategies such as standardized workflows and technology integration, healthcare organizations can create more efficient, patient-centric environments. The continuous monitoring of performance through data-driven KPIs and the adoption of continuous quality improvement principles are not mere optional additions but fundamental components for sustaining improvements and ensuring that medical rooms, the heart of clinical care, operate as effectively as possible. The ultimate goal is not just to see more patients, but to provide better, safer, and more timely care for every individual who enters these critical spaces.



