In the realm of clinical research, the integration of Interactive Response Technology (IRT) systems has revolutionized the way clinical trials are conducted. IRT systems facilitate the management of patient enrollment, randomization, and drug supply logistics, thereby streamlining the entire trial process. These systems are designed to enhance the efficiency and accuracy of clinical trials, which are essential for bringing new therapies to market.
The evolution of IRT systems has been driven by the need for real-time data management and the increasing complexity of clinical trial designs. As trials become more intricate, the role of IRT systems becomes increasingly critical in ensuring that they are executed smoothly and effectively. The significance of IRT systems extends beyond mere operational efficiency; they play a pivotal role in safeguarding patient safety and ensuring compliance with regulatory standards.
By automating various processes, IRT systems minimize human error and enhance data integrity, which is crucial for the credibility of trial outcomes. As clinical trials continue to evolve in response to emerging medical needs and technological advancements, understanding the intricacies of IRT systems becomes essential for stakeholders involved in the research process.
Key Takeaways
- IRT systems play a crucial role in managing and optimizing clinical trial processes.
- Patient outcomes are a key focus in evaluating the success of clinical trials.
- IRT systems help address challenges in patient data management and trial logistics.
- Successful case studies demonstrate the effectiveness of IRT systems in improving outcomes.
- Best practices and future advancements in IRT systems promise enhanced patient care in trials.
The Importance of Patient Outcomes in Clinical Trials
Patient outcomes are at the heart of clinical trials, serving as the primary measure of a treatment’s efficacy and safety. These outcomes encompass a wide range of metrics, including survival rates, quality of life, and symptom relief, all of which are critical for evaluating the success of a new intervention. The focus on patient outcomes has shifted from merely assessing clinical endpoints to incorporating patient-reported outcomes (PROs), which provide valuable insights into how patients perceive their health status and treatment experiences.
This shift underscores the importance of patient-centered approaches in clinical research, emphasizing that the ultimate goal is to improve patients’ lives. Moreover, regulatory agencies such as the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have increasingly recognized the importance of patient outcomes in their approval processes. They advocate for the inclusion of PROs in clinical trial designs to ensure that new therapies not only meet statistical significance but also translate into meaningful benefits for patients.
This growing emphasis on patient outcomes necessitates robust methodologies for capturing and analyzing data, making it imperative for clinical trial sponsors to adopt innovative solutions like IRT systems that can effectively manage this complexity.
Understanding the Role of IRT Systems in Clinical Trials

IRT systems serve as a backbone for managing various aspects of clinical trials, including patient randomization, drug inventory management, and data collection. These systems enable real-time tracking of patient enrollment and treatment allocation, ensuring that trials adhere to their protocols while maintaining compliance with regulatory requirements. By automating these processes, IRT systems reduce administrative burdens on clinical trial staff, allowing them to focus on more strategic tasks that directly impact patient care.
One of the key functionalities of IRT systems is their ability to facilitate adaptive trial designs. In an adaptive trial, modifications can be made based on interim results without compromising the integrity of the study. This flexibility is crucial in responding to emerging data trends and optimizing treatment pathways for patients.
For instance, if early results indicate that a particular treatment is more effective in a specific demographic group, an IRT system can quickly adjust randomization strategies to ensure that more patients receive that treatment. This capability not only enhances the scientific rigor of trials but also aligns with the overarching goal of improving patient outcomes.
Challenges in Patient Outcomes and How IRT Systems Can Help
Despite advancements in clinical trial methodologies, challenges persist in accurately capturing and analyzing patient outcomes. One significant hurdle is ensuring consistent data collection across diverse sites and populations. Variability in how outcomes are measured can lead to discrepancies that undermine the validity of trial results.
Additionally, patient dropout rates can skew data, making it difficult to assess long-term efficacy and safety. These challenges highlight the need for robust systems that can standardize data collection processes and maintain engagement with participants throughout the trial. IRT systems address these challenges by providing a centralized platform for data management that ensures consistency across all trial sites.
By standardizing outcome measures and utilizing electronic data capture methods, IRT systems facilitate accurate and reliable data collection. Furthermore, these systems can implement automated reminders and follow-up protocols to enhance patient retention, thereby minimizing dropout rates. For example, an IRT system can send automated messages to participants reminding them of upcoming visits or assessments, which not only keeps patients engaged but also ensures that critical data points are collected in a timely manner.
Case Studies: Successful Implementation of IRT Systems in Clinical Trials
| Metric | Description | Value | Unit |
|---|---|---|---|
| Number of Participants | Total enrolled subjects in the IRT system clinical trial | 250 | Participants |
| Randomization Rate | Percentage of participants successfully randomized using the IRT system | 98 | % |
| Drug Dispensation Accuracy | Accuracy rate of drug dispensation managed by the IRT system | 99.5 | % |
| Enrollment Duration | Time taken to complete participant enrollment | 6 | Months |
| System Downtime | Total downtime experienced by the IRT system during the trial | 2 | Hours |
| Data Query Rate | Percentage of data queries related to IRT system data | 1.2 | % |
| Randomization Error Rate | Incidence of errors during randomization process | 0.3 | % |
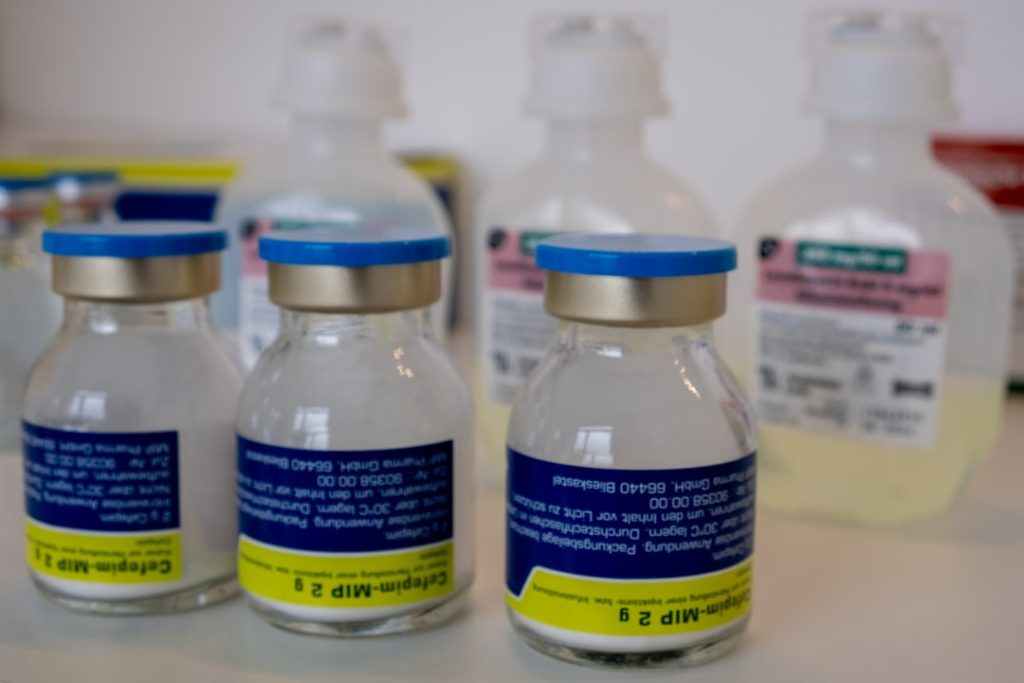
Numerous case studies illustrate the successful implementation of IRT systems in enhancing clinical trial efficiency and improving patient outcomes. One notable example is a Phase III oncology trial that utilized an IRT system to manage patient randomization and drug supply logistics across multiple sites worldwide. The system enabled real-time tracking of patient enrollment and treatment allocation, which was crucial given the trial’s complex design involving multiple treatment arms.
As a result, the trial was completed ahead of schedule, with a significant reduction in administrative errors related to randomization. Another compelling case involved a cardiovascular study where an IRT system was employed to monitor patient-reported outcomes throughout the trial duration. By integrating PRO measures into the IRT platform, researchers were able to capture real-time feedback from participants regarding their symptoms and quality of life.
This data not only enriched the overall understanding of treatment effects but also allowed for timely interventions when patients reported adverse events or deteriorating health status. The successful integration of PROs into the trial design ultimately contributed to a more comprehensive assessment of treatment efficacy and safety.
Best Practices for Utilizing IRT Systems to Improve Patient Outcomes
To maximize the benefits of IRT systems in clinical trials, several best practices should be adopted by research teams. First and foremost is the importance of thorough planning during the trial design phase. Engaging stakeholders—including clinicians, data managers, and regulatory experts—early in the process ensures that the IRT system is tailored to meet specific trial needs.
This collaborative approach fosters a shared understanding of objectives and facilitates seamless integration into existing workflows. Another best practice involves continuous training and support for clinical trial staff who will be using the IRT system. Providing comprehensive training sessions ensures that all team members are proficient in utilizing the technology effectively.
Additionally, establishing a dedicated support team can help address any technical issues that arise during the trial, minimizing disruptions that could impact patient outcomes. Regular feedback loops should also be established to assess system performance and identify areas for improvement throughout the trial lifecycle.
The Future of IRT Systems in Clinical Trials
As technology continues to advance at an unprecedented pace, the future of IRT systems in clinical trials looks promising. Innovations such as artificial intelligence (AI) and machine learning are poised to enhance data analytics capabilities within IRT platforms. These technologies can analyze vast amounts of data in real time, identifying trends and patterns that may not be immediately apparent to human researchers.
This capability could lead to more informed decision-making regarding treatment adjustments and patient management strategies. Moreover, as patient engagement becomes increasingly central to clinical research, future IRT systems may incorporate more interactive features that empower patients to take an active role in their care. For instance, mobile applications linked to IRT platforms could allow patients to report outcomes directly from their devices, providing researchers with immediate access to valuable data while enhancing participant engagement.
Such advancements will not only improve data quality but also foster a sense of ownership among patients regarding their treatment journeys.
The Impact of IRT Systems on Patient Outcomes
The integration of Interactive Response Technology systems into clinical trials has fundamentally transformed how research is conducted, particularly concerning patient outcomes. By streamlining processes such as randomization and data collection while enhancing patient engagement through real-time feedback mechanisms, IRT systems have proven instrumental in improving both operational efficiency and data integrity. As clinical trials continue to evolve in complexity and scope, leveraging these advanced technologies will be essential for ensuring that new therapies are not only effective but also aligned with patients’ needs and experiences.
The ongoing development and refinement of IRT systems will undoubtedly play a crucial role in shaping the future landscape of clinical research. By prioritizing patient outcomes through innovative solutions, researchers can ensure that their efforts translate into meaningful advancements in healthcare—ultimately leading to improved quality of life for patients around the world.