Applied clinical trials serve as a cornerstone in the advancement of medical science, directly influencing patient outcomes by rigorously testing new treatments, therapies, and interventions. These trials are designed to evaluate the efficacy and safety of medical products in real-world settings, providing critical data that informs clinical practice. By bridging the gap between laboratory research and patient care, applied clinical trials ensure that innovations are not only theoretically sound but also practically beneficial for patients.
For instance, the development of new cancer therapies often relies on extensive clinical trials to determine their effectiveness in diverse populations, ultimately leading to improved survival rates and quality of life for patients. Moreover, applied clinical trials contribute to the continuous evolution of treatment protocols. As new data emerges from these studies, healthcare providers can refine their approaches to patient care, tailoring interventions to meet the specific needs of different patient populations.
This iterative process is vital in fields such as cardiology, where clinical trials have led to the development of personalized treatment plans based on genetic markers and other individual characteristics. The impact of these trials extends beyond immediate patient outcomes; they also shape healthcare policies and guidelines, ensuring that evidence-based practices are at the forefront of medical care.
Key Takeaways
- Applied clinical trials are crucial for improving patient outcomes by testing real-world treatments.
- Designing trials with patient needs in mind ensures relevance and effectiveness.
- Patient-centric approaches enhance engagement and trial success.
- Technology and data analysis optimize trial processes and result accuracy.
- Collaboration with healthcare providers and adherence to ethics boost trial integrity and impact.
Designing Effective Clinical Trials to Address Patient Needs
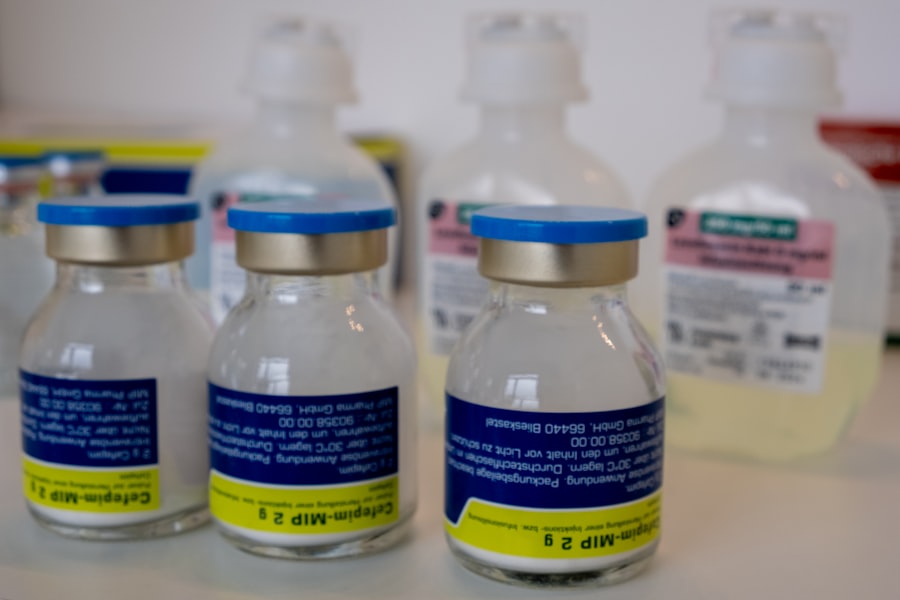
The design of clinical trials is a critical factor that determines their success in addressing patient needs. A well-structured trial must consider various elements, including the target population, endpoints, and methodologies. For example, when designing a trial for a new diabetes medication, researchers must carefully select participants who reflect the diversity of the patient population affected by the disease.
This includes considering factors such as age, gender, ethnicity, and comorbidities. By ensuring that the trial cohort is representative, researchers can generate findings that are more applicable to the broader population. Additionally, the choice of endpoints is paramount in trial design.
Endpoints should not only measure clinical efficacy but also consider patient-reported outcomes, such as quality of life and symptom relief. For instance, in trials for chronic pain medications, incorporating patient feedback on pain management and daily functioning can provide a more comprehensive understanding of the treatment’s impact. This focus on relevant outcomes helps ensure that the results are meaningful to both patients and healthcare providers, ultimately guiding better clinical decisions.
Utilizing Patient-Centric Approaches in Clinical Trial Design
In recent years, there has been a significant shift towards patient-centric approaches in clinical trial design. This paradigm emphasizes the importance of involving patients in the planning and execution of trials to ensure that their perspectives and preferences are considered. Engaging patients early in the process can lead to more relevant research questions and outcomes that truly reflect their needs.
For example, focus groups or surveys can be conducted to gather insights from potential participants about what they value most in treatment options. Furthermore, patient-centric trial designs often incorporate flexible protocols that accommodate individual patient circumstances. This might include allowing for remote monitoring or telehealth consultations, which can enhance accessibility for patients who may have difficulty attending in-person visits due to mobility issues or geographical barriers.
By prioritizing the patient experience throughout the trial process, researchers can foster greater trust and collaboration between participants and study teams, ultimately leading to higher retention rates and more robust data collection.
Enhancing Patient Recruitment and Retention in Clinical Trials
Recruitment and retention are two of the most significant challenges faced by clinical trials. A successful trial requires not only a sufficient number of participants but also their continued engagement throughout the study duration. To enhance recruitment efforts, researchers must employ diverse strategies that reach potential participants where they are.
This may involve leveraging social media platforms, community outreach programs, or partnerships with local healthcare providers to raise awareness about ongoing trials. Retention strategies are equally important and can significantly impact the integrity of trial results. Providing clear communication about the trial’s purpose, procedures, and potential benefits can help alleviate participant concerns and foster a sense of ownership in the research process.
Additionally, offering incentives such as travel reimbursements or access to new treatments can motivate participants to remain engaged. For instance, a trial investigating a novel treatment for rheumatoid arthritis might include regular follow-up appointments with healthcare professionals who can provide ongoing support and address any concerns that arise during the study.
Leveraging Technology and Data Analysis for Better Patient Outcomes
| Metric | Description | Typical Value/Range | Importance |
|---|---|---|---|
| Enrollment Rate | Number of patients enrolled per month | 5-50 patients/month | Measures recruitment efficiency |
| Retention Rate | Percentage of patients completing the trial | 70%-95% | Indicates participant adherence and trial quality |
| Protocol Deviation Rate | Percentage of visits or data points not following protocol | 1%-10% | Reflects trial compliance and data integrity |
| Adverse Event Rate | Number of adverse events reported per 100 patients | Varies by trial phase and drug | Assesses safety profile |
| Data Query Rate | Number of data queries per 100 case report forms (CRFs) | 5-20 queries/100 CRFs | Indicates data quality and monitoring effectiveness |
| Time to Database Lock | Duration from last patient last visit to database lock | 1-3 months | Measures data cleaning and readiness for analysis |
| Cost per Patient | Average cost to enroll and complete one patient | Varies widely by indication and phase | Important for budgeting and financial planning |
The integration of technology into clinical trials has revolutionized data collection and analysis, leading to improved patient outcomes. Electronic health records (EHRs), mobile health applications, and wearable devices enable researchers to gather real-time data on patient health metrics and treatment responses. This wealth of information allows for more nuanced analyses and can help identify trends that may not be apparent through traditional data collection methods.
Moreover, advanced data analytics techniques such as machine learning and artificial intelligence are increasingly being utilized to enhance trial design and execution. These technologies can help identify suitable candidates for trials based on complex criteria or predict potential adverse events by analyzing large datasets from previous studies. For example, AI algorithms can analyze genetic data to identify patients who are most likely to benefit from a specific therapy, thereby optimizing recruitment efforts and improving overall trial efficiency.
Collaborating with Healthcare Providers for Successful Clinical Trials
Collaboration with healthcare providers is essential for the success of clinical trials. Physicians play a crucial role in identifying potential participants and facilitating their involvement in research studies. By fostering strong relationships with healthcare professionals, researchers can create a network of advocates who understand the importance of clinical trials and can effectively communicate this to their patients.
Additionally, involving healthcare providers in the trial design process can lead to more relevant research questions and methodologies. Their insights into patient care practices and challenges can help shape studies that address real-world issues faced by patients. For instance, a trial focused on a new hypertension medication might benefit from input from cardiologists who understand the complexities of managing blood pressure in patients with multiple comorbidities.
This collaborative approach not only enhances the quality of research but also ensures that findings are readily applicable in clinical settings.
Ensuring Ethical and Regulatory Compliance in Clinical Trials
Ethical considerations are paramount in clinical trials, as they directly impact participant safety and trust in the research process. Ensuring ethical compliance involves adhering to established guidelines and regulations designed to protect human subjects. Institutional Review Boards (IRBs) play a critical role in reviewing study protocols to ensure that they meet ethical standards before approval.
In addition to regulatory compliance, transparency is essential in maintaining public trust in clinical research. Researchers must provide clear information about trial objectives, risks, benefits, and participant rights. Informed consent processes should be thorough and understandable, allowing participants to make educated decisions about their involvement.
For example, when conducting trials involving vulnerable populations such as children or individuals with cognitive impairments, additional safeguards must be implemented to ensure their protection.
The Future of Applied Clinical Trials in Advancing Patient Care
The future of applied clinical trials holds great promise for advancing patient care through innovative methodologies and technologies. As personalized medicine continues to gain traction, clinical trials will increasingly focus on tailoring treatments to individual patient profiles based on genetic, environmental, and lifestyle factors. This shift will require adaptive trial designs that allow for modifications based on interim results, enabling researchers to respond dynamically to emerging data.
Furthermore, as healthcare systems become more integrated with technology, remote monitoring and telemedicine will likely play a larger role in clinical trials. This evolution will enhance accessibility for participants while also providing researchers with continuous data streams that can inform treatment efficacy in real time. The integration of artificial intelligence into trial design will further streamline processes such as patient recruitment and data analysis, ultimately leading to faster and more efficient studies.
In conclusion, applied clinical trials are essential for improving patient outcomes through rigorous testing of new treatments while addressing real-world needs through thoughtful design and execution. As we move forward into an era characterized by technological advancements and a greater emphasis on patient-centered care, the landscape of clinical research will continue to evolve, paving the way for innovative solutions that enhance health outcomes for all patients.




