Clinical trials are foundational to medical progress, serving as the crucible where novel treatments, diagnostic tools, and preventive strategies are tested and validated. Without them, medical innovation would stagnate, and our understanding of human health and disease would remain rudimentary. These meticulously designed research studies are not merely an academic exercise; they represent a critical bridge between laboratory discoveries and widespread clinical application. Participating in a clinical trial is a tangible contribution to this ongoing endeavor, a direct investment in the future of healthcare. It is a decision that impacts not only the individual participant but also the broader community and future generations.
Understanding Clinical Trials
Clinical trials are systematic investigations involving human volunteers, designed to evaluate the safety and efficacy of new medical interventions. They adherence to stringent protocols and ethical guidelines to protect participant welfare and ensure the integrity of the collected data. The process is typically categorized into distinct phases, each with specific objectives.
Phases of Clinical Trials
The journey of a new medical intervention through clinical trials is a multi-stage process:
- Phase 0 Trials: These are exploratory, first-in-human trials often involving very small doses of a new drug to confirm that it behaves in humans as predicted by preclinical models. They aim to gather preliminary data on pharmacodynamics and pharmacokinetics without therapeutic intent.
- Phase I Trials: Focus on safety. A small group of healthy volunteers or patients (typically 20-100) receives the experimental treatment. The primary goals are to determine a safe dosage range, identify potential side effects, and assess how the drug is absorbed, metabolized, and excreted.
- Phase II Trials: Evaluate efficacy and further assess safety. Conducted with a larger group of patients (typically 100-300) who have the condition the treatment aims to address. Researchers look for preliminary evidence that the treatment works and continue to monitor for adverse effects.
- Phase III Trials: Confirm efficacy and safety, often in comparison to existing treatments or a placebo. These are large-scale studies involving hundreds to thousands of participants. If a treatment successfully completes Phase III, it can typically be submitted for regulatory approval.
- Phase IV Trials (Post-Marketing Surveillance): Occur after a drug or device has been approved and is on the market. These studies monitor long-term safety and effectiveness in a broader patient population, identify rare side effects, and explore new uses or populations.
Types of Interventions Studied
Clinical trials encompass a wide array of medical interventions, not solely limited to pharmaceuticals:
- Drugs: New pharmaceutical compounds, repurposed existing drugs, or novel formulations.
- Biologics: Vaccines, antibodies, gene therapies, and cell therapies derived from living organisms.
- Medical Devices: Implants, diagnostic instruments, and surgical tools.
- Procedures: Surgical techniques, radiation therapies, or other medical interventions.
- Behavioral Interventions: Lifestyle modifications, dietary changes, or psychological therapies.
- Preventive Measures: Vaccines, dietary supplements, or specific health education programs.
The Role of Participants
Participants are the linchpin of clinical research. Without their voluntary involvement, the advancement of medical science would be severely hampered. Each participant is a crucial component in the collective effort to unravel the complexities of disease and forge pathways to improved health. The decision to participate is significant and often requires careful consideration of personal circumstances, potential benefits, and risks.
Informed Consent
A cornerstone of ethical research, informed consent is a process, not merely a signature on a document. Before enrolling in a trial, prospective participants receive comprehensive information about the study’s purpose, procedures, potential risks, benefits, and alternatives. This process ensures that individuals make a voluntary, uncoerced decision based on a thorough understanding of what participation entails. It is an ongoing dialogue, with participants having the right to ask questions and withdraw at any time.
Patient Safety and Ethical Oversight
The protection of participants is paramount. Clinical trials are subject to strict ethical guidelines and regulatory oversight to minimize risks and ensure participant well-being.
- Institutional Review Boards (IRBs) / Ethics Committees (ECs): Independent committees composed of medical professionals, scientists, and community members who review and approve research protocols. They ensure that trials are ethically sound, scientifically valid, and that participant rights are protected.
- Data and Safety Monitoring Boards (DSMBs): Independent groups of experts who periodically review accumulating data from ongoing trials to ensure participant safety and trial integrity. They can recommend modifications or even early termination of a study if safety concerns arise or if a clear benefit or lack of benefit is demonstrated prematurely.
- Regulatory Agencies: Government bodies, such as the Food and Drug Administration (FDA) in the United States or the European Medicines Agency (EMA) in Europe, provide extensive regulatory frameworks for the conduct of clinical trials, ensuring compliance with established standards.
Benefits and Risks of Participation
Engaging in a clinical trial carries both potential advantages and disadvantages, which prospective participants must weigh carefully.
Potential Benefits
While participation in a clinical trial does not guarantee a direct therapeutic benefit, several advantages can accrue to participants:
- Access to Novel Treatments: Participants may gain access to cutting-edge therapies that are not yet widely available, potentially before they reach the general market. This can be particularly relevant for conditions with limited existing treatment options.
- Close Medical Monitoring: Clinical trial participants often receive more frequent and thorough medical attention and monitoring than they would in routine clinical practice. This extensive oversight can contribute to better management of their underlying condition.
- Contribution to Medical Knowledge: A critical, often overlooked benefit is the satisfaction of contributing to scientific discovery and improving the health of future generations. Participants become part of the collective effort to advance medical understanding.
- Financial Compensation: Some trials offer stipends or reimbursement for travel and time, though this is not the primary motivator for participation and is always disclosed upfront.
Potential Risks and Discomforts
Clinical trials, by their nature, involve an element of uncertainty. It is crucial to understand the potential risks:
- Adverse Effects: Experimental treatments may cause unexpected side effects or adverse reactions. These can range from mild to severe, and in rare cases, they can be life-threatening.
- Ineffectiveness: The experimental treatment may not be more effective than, or even as effective as, existing treatments or a placebo. Participants may experience no improvement in their condition.
- Increased Time Commitment: Participation often requires frequent visits to the study site, additional tests, and adherence to specific protocols, which can be time-consuming.
- Placebo Effect or Standard of Care Arm: Some trials involve a placebo group or a comparison group receiving standard treatment. Participants assigned to these groups may not receive the experimental intervention.
- Unforeseen Outcomes: Despite rigorous safety measures, all medical interventions carry some inherent unpredictability.
Finding and Joining a Clinical Trial
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Enrollment Rate | Percentage of eligible participants who join the trial | 30% – 70% | Indicates trial accessibility and appeal |
| Retention Rate | Percentage of participants who complete the trial | 70% – 90% | Reflects participant satisfaction and trial feasibility |
| Average Trial Duration | Length of time participants are involved in the trial | 6 months – 3 years | Impacts participant commitment and data collection |
| Number of Active Trials | Total ongoing clinical trials available for enrollment | Thousands globally | Indicates availability of research opportunities |
| Common Eligibility Criteria | Typical requirements for joining trials (age, condition, etc.) | Age 18-65, diagnosed condition, no conflicting medications | Determines participant suitability |
| Informed Consent Rate | Percentage of participants who fully understand and agree to trial terms | 95%+ | Ensures ethical participation |
| Adverse Event Rate | Percentage of participants experiencing side effects | Varies by trial, typically 5% – 30% | Monitors safety of interventions |
The process of locating and enrolling in a clinical trial involves several steps and resources. Prospective participants should engage in thorough research and communication with their healthcare providers.
Resources for Trial Search
Multiple platforms and entities facilitate the search for relevant clinical trials:
- ClinicalTrials.gov: A comprehensive, publicly accessible database maintained by the U.S. National Library of Medicine. It lists privately and publicly funded clinical studies conducted around the world, providing detailed information about each trial, including eligibility criteria, locations, and contact information.
- Disease-Specific Organizations: Many patient advocacy groups and disease foundations maintain registries or lists of clinical trials pertinent to their specific conditions. These organizations often provide tailored guidance and support.
- Hospital and University Research Departments: Academic medical centers and large hospitals are frequently involved in conducting clinical research. Their websites often list ongoing studies.
- Healthcare Providers: Your personal physician or specialist is a critical resource. They can assess your medical history, discuss whether a trial is appropriate, and help identify suitable studies.
The Enrollment Process
Once a potential trial is identified, the enrollment process typically involves:
- Initial Contact: Reaching out to the research team to express interest.
- Pre-Screening: A preliminary assessment, often over the phone, to determine if basic eligibility criteria are met.
- Informed Consent Discussion: A detailed meeting where the research team explains the trial, and you have the opportunity to ask questions.
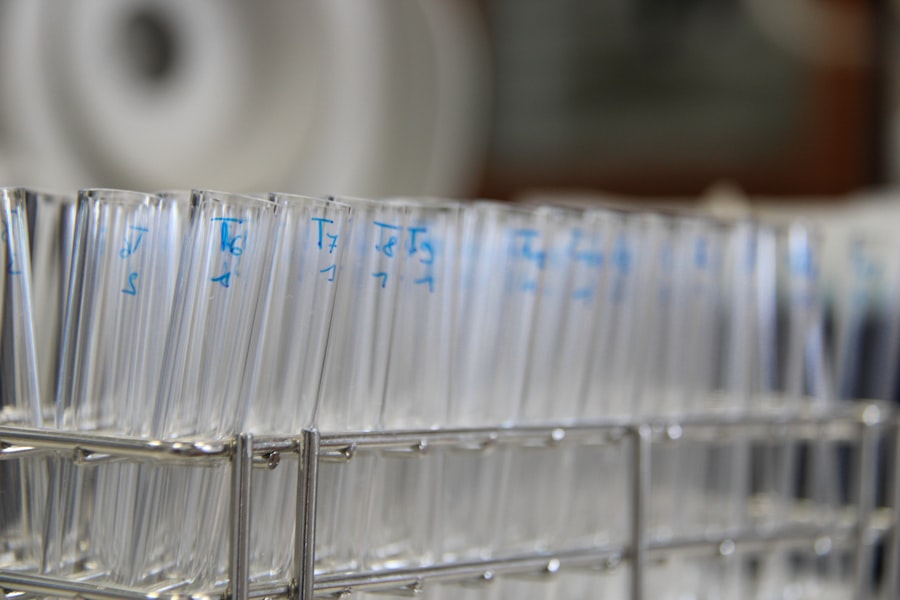
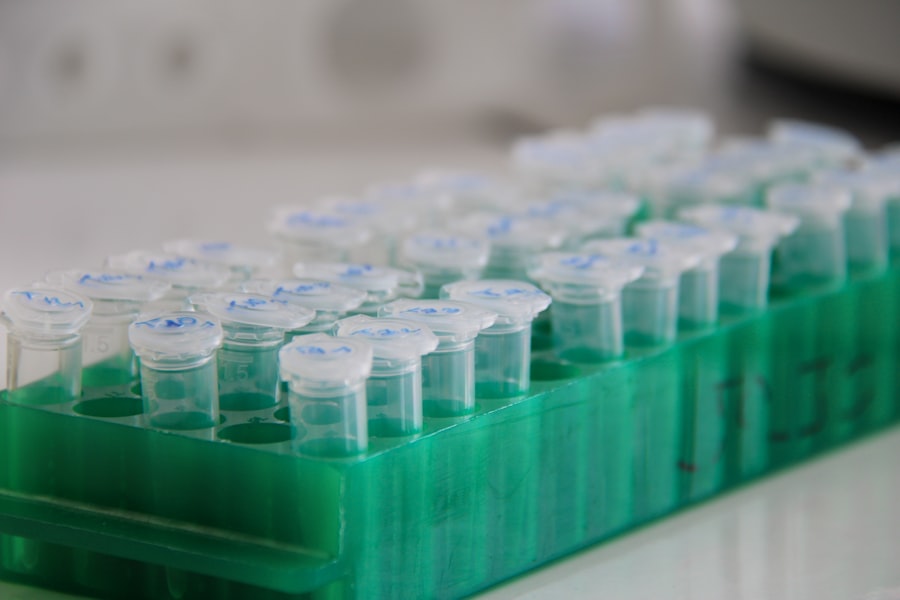
- Screening Visit: A comprehensive medical evaluation to confirm eligibility, which may include physical exams, blood tests, imaging, and other diagnostic procedures.
- Enrollment: If all eligibility criteria are met and informed consent is provided, you are officially enrolled in the study.
The Future of Medical Advancement
Clinical trials are more than just experiments; they are the engines of progress in medicine. Each trial, whether successful or not, contributes to the collective knowledge base that informs future research and clinical practice. By understanding the intricate mechanisms of disease and meticulously evaluating interventions, we collectively push the boundaries of what is medically possible. Your consideration of participation in a clinical trial is a recognition of this scientific imperative and positions you as an active contributor to the ongoing quest for improved health outcomes for all. The cumulative impact of individual choices to participate in these studies reverberates throughout the global healthcare landscape, shaping the trajectory of medical innovation.



