Clinical trials are research studies performed in humans that evaluate new medical treatments, interventions, or devices. These studies are essential components of the medical research pipeline, serving as the bridge between laboratory discoveries and widespread patient care. They are designed to determine if new approaches are safe and effective. Without clinical trials, the development of new medications, therapies, and diagnostic tools would be severely hampered. For individuals, participation can offer early access to potentially life-saving or life-improving treatments.
Phases of Clinical Trials
Clinical trials typically progress through a series of four phases, each with distinct objectives:
Phase 1: Safety and Dosage
Phase 1 trials are the initial human studies of an experimental drug or treatment. They usually involve a small group of healthy volunteers, typically 20-100 participants. The primary goal is to assess the treatment’s safety, determine a safe dosage range, and identify potential side effects. This phase is like testing the foundation of a building; it ensures core stability before further construction.
Phase 2: Efficacy and Further Safety
Phase 2 trials involve a larger group of participants, usually several hundred, who have the disease or condition that the new treatment aims to address. The focus shifts to evaluating the treatment’s efficacy (how well it works) and continuing to monitor safety. Researchers also collect more information on dosage and administration. Here, we’re testing the building’s functionality – does it serve its purpose?
Phase 3: Confirmation and Comparison
Phase 3 trials are large-scale studies involving hundreds to thousands of participants. These trials compare the new treatment to existing standard treatments or a placebo. The aim is to confirm efficacy, monitor side effects, compare it to common treatments, and collect information that will allow the treatment to be used safely. This phase is akin to stress-testing the building in various environments, ensuring it holds up against the competition.
Phase 4: Post-Marketing Surveillance
Phase 4 trials are conducted after a drug or treatment has been approved and marketed to the general public. These studies gather additional information about the treatment’s long-term effects, optimal use, and any rare side effects that may not have appeared in earlier phases. It’s an ongoing inspection of the building, checking for wear and tear and unexpected issues over time.
Compensation in Clinical Trials
Participation in clinical trials often involves compensation for various reasons. This compensation is not a payment for medical services but rather an acknowledgment of the participant’s time, effort, and inconvenience. It can help offset costs such as travel, parking, and lost wages.
Types of Compensation
Compensation structures vary depending on the trial, its duration, complexity, and the participant’s involvement.
- Direct Payments: Monetary compensation is common, often provided as a lump sum or in installments after each study visit.
- Travel Reimbursement: Many trials offer reimbursement for travel expenses to and from the study site.
- Meals and Accommodation: For trials requiring extended stays or multiple visits, meals or accommodation may be provided.
- Study-Related Medical Care: While not direct compensation, all study-related medical care, including tests and medications, is typically provided without cost to the participant. This is a significant benefit, especially for those without adequate health insurance.
Ethical Considerations of Compensation
The amount of compensation is subject to ethical review by an Institutional Review Board (IRB) or Ethics Committee. The primary concern is that compensation should not be so high as to unduly influence an individual’s decision to participate, especially given potential risks. The compensation should be fair and reasonable, reflecting the burden, time, and inconvenience involved. Excessive compensation could be coercive, undermining the voluntary nature of participation.
Finding Lucrative Clinical Trials
Identifying clinical trials, particularly those offering compensation, requires a systematic approach. Several resources are available to the public.
Online Databases
Government and private organizations maintain comprehensive online databases of ongoing clinical trials. These databases are often searchable by location, medical condition, study phase, and compensation.
- ClinicalTrials.gov: Operated by the U.S. National Library of Medicine, ClinicalTrials.gov is a primary resource for finding federally and privately funded clinical trials around the world. It provides detailed information on study protocols, eligibility criteria, and contact information. You can filter by study type, phase, and location.
- WHO International Clinical Trials Registry Platform (ICTRP): This platform provides a single point of access to information about clinical trials from around the world. It pulls data from various national and regional registries.
- CenterWatch.com: A commercial site that lists clinical trials and provides resources for patients, professionals, and researchers. It often highlights trials that are actively recruiting and may offer compensation.
Hospital and University Research Centers
Major hospitals and university medical centers are often at the forefront of medical research. They frequently conduct a variety of clinical trials across numerous therapeutic areas.
- Direct Contact: Many institutions have dedicated research departments or patient recruitment offices. Visiting their websites or contacting them directly can yield information on current studies.
- Local Listings: These centers may post listings of trials in their facilities, on bulletin boards, or in local community newspapers.
- Specialized Clinics: If you have a specific medical condition, contacting specialist clinics or physicians can be an effective way to learn about relevant trials. They are often involved in research and can provide direct referrals.
Patient Advocacy Groups
Advocacy groups for specific diseases or conditions often maintain lists of clinical trials pertinent to their members. These organizations are deeply connected to the research community and can be valuable conduits of information.
- Support Networks: Joining online forums or local support groups related to your health condition can provide peer-to-peer information sharing about trials.
- Newsletters and Websites: Many advocacy groups publish newsletters or maintain websites with dedicated sections on clinical trial opportunities.
Eligibility and Screening
Before participating in any clinical trial, potential participants undergo a rigorous screening process. This is not arbitrary; it’s a critical step to ensure participant safety and the scientific integrity of the study.
Inclusion and Exclusion Criteria
Every clinical trial has a specific set of inclusion and exclusion criteria. These are predetermined factors that define who can and cannot participate.
- Inclusion Criteria: These are characteristics that a person must possess to be eligible for a study. Examples include age range, diagnosis of a specific condition, gender, or certain medical history parameters.
- Exclusion Criteria: These are characteristics that would prevent a person from participating, even if they meet some inclusion criteria. Examples include pregnancy, other co-existing medical conditions, use of certain medications, or previous participation in a similar trial.
These criteria are akin to a finely tuned filter, designed to select a homogeneous study population that will respond predictably to the intervention and minimize confounding variables. Failure to meet one or more criteria will lead to disqualification, regardless of individual interest.
Medical Screening Process
The screening process involves a series of medical evaluations and assessments to determine if a potential participant meets the eligibility criteria.
- Medical History Review: Detailed review of past and present medical conditions, medications, and treatments.
- Physical Examination: A comprehensive physical check-up to assess overall health.
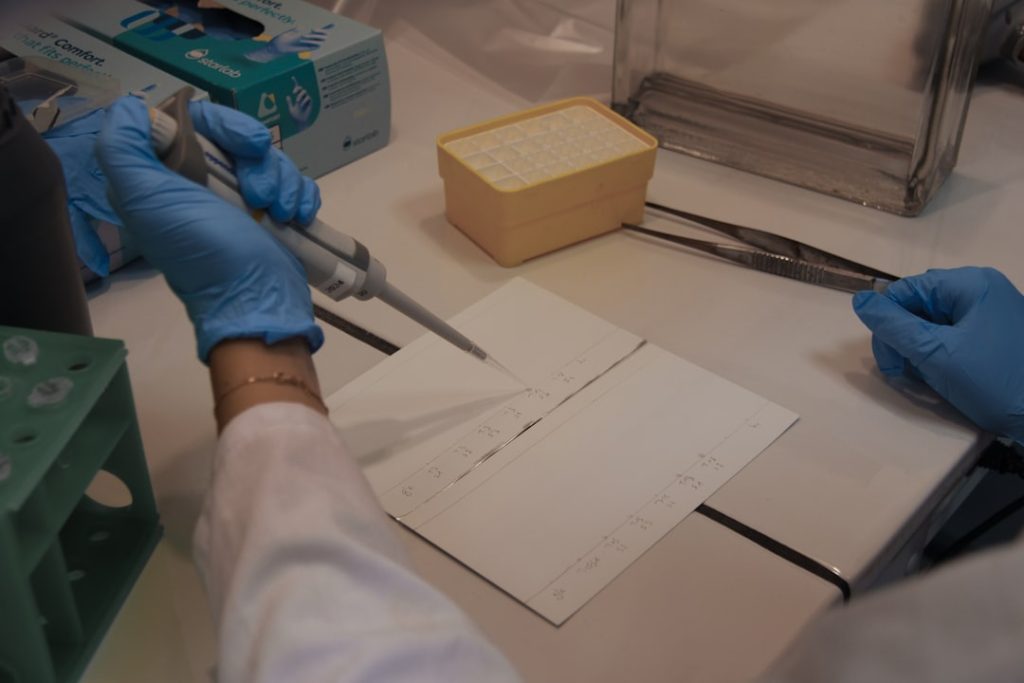
- Laboratory Tests: Blood work, urine tests, and other diagnostic tests to check organ function and detect underlying conditions.
- Diagnostic Imaging: X-rays, MRIs, or CT scans may be performed depending on the study’s focus.
- Questionnaires and Interviews: Assessments of lifestyle, mental health, and adherence to study requirements.
This process can be time-consuming, and there is no guarantee of acceptance. It is designed to protect participants from undue risk and to ensure that the study’s results are valid and reliable. Imagine building a precision instrument; each component must be exact for the whole to function correctly.
Risks and Benefits of Participation
Deciding whether to participate in a clinical trial is a significant personal choice that involves weighing potential risks against potential benefits. It’s a decision that must be made with eyes wide open, fully informed.
Potential Benefits
While participation offers no guarantees, there are several general benefits.
- Access to New Treatments: Participants may gain early access to experimental treatments not yet available to the general public. For individuals with life-threatening or debilitating conditions, this can be a lifeline.
- Close Medical Monitoring: Clinical trial participants typically receive careful medical attention and frequent monitoring from a team of healthcare professionals. This can be more intensive than standard care.
- Contribution to Medical Science: By participating, individuals play a direct role in advancing scientific knowledge and helping others in the future. This sense of altruism is a significant motivator for many.
- No-Cost Medical Care (Study-Related): As mentioned, all study-related medical procedures, drugs, and tests are usually provided free of charge, which can be advantageous for those without comprehensive health coverage.
Potential Risks
Participation also carries inherent risks, as new treatments are, by definition, unproven.
- Unknown Side Effects: The experimental treatment may have adverse side effects that are unexpected, severe, or even life-threatening. The full safety profile of a new intervention is often not completely understood until later phases.
- Ineffectiveness: The treatment may not be more effective than standard treatment, or it may not work at all for the individual participant. There is no guarantee of therapeutic benefit.
- Placebo Effect: Some trials involve a placebo group, meaning participants may receive an inactive substance instead of the experimental treatment. They would then not receive the active intervention being studied.
- Time Commitment and Inconvenience: Clinical trials often require numerous visits to the study site, extensive tests, and strict adherence to protocol, which can be demanding on personal time.
- Confidentiality Concerns: While strong safeguards are in place, there is always a minimal inherent risk of privacy breaches, though regulations like HIPAA (in the US) aim to protect participant data.
Informed Consent Process
Before anyone can participate in a clinical trial, they must go through a comprehensive informed consent process. This is a conversation, not just a signature.
- Detailed Explanation: Researchers provide a detailed explanation of the trial’s purpose, procedures, potential risks, benefits, and alternatives.
- Questions and Answers: Participants are given ample opportunity to ask questions and have them answered to their satisfaction.
- Voluntary Participation: Emphasized as voluntary, with the right to withdraw at any time without penalty or loss of benefits.
- Consent Form: Participants sign an informed consent form, indicating they understand the study and agree to participate. This document is a legal and ethical cornerstone of human research.
The informed consent form acts as a detailed map, guiding the participant through the journey ahead, highlighting both the scenic routes and potential pitfalls. It is not just a formality; it is a critical instrument for ethical research and participant autonomy.
Understanding the “Lucrative” Aspect
When people refer to “lucrative” clinical trials, they are typically referring to those that offer significant financial compensation. While direct compensation for participation can be substantial in some cases, it’s crucial to understand the context and purpose. It is not a means to generate regular employment income.
Factors Influencing Compensation Levels
Several factors influence the level of compensation offered in a clinical trial.
- Phase of Study: Phase 1 trials, particularly those involving healthy volunteers and potentially higher risks or intensive procedures, often offer the highest compensation due to the absence of direct therapeutic benefit for participants. As studies progress to later phases (2 and 3), participants may already have the condition being treated, and the primary benefit can be access to the experimental treatment itself, potentially reducing the emphasis on financial compensation.
- Intensity and Duration: Trials that require lengthy stays at a clinic, frequent visits, numerous invasive procedures (e.g., biopsies, spinal taps), or a long overall duration tend to offer higher compensation to account for the increased burden and disruption to the participant’s daily life.
- Risk Level: Studies involving treatments with potentially higher or unknown risks may offer greater compensation to reflect the increased burden and sacrifice. This compensation acts as an acknowledgement of the additional burden.
- Participant Population: Some trials seek specific, hard-to-find participant populations, such as individuals with rare diseases or very specific genetic profiles. The difficulty in recruitment can sometimes lead to higher compensation offers.
- Market Forces and Competition: The research landscape is competitive. If multiple trials are seeking similar participants, compensation levels may fluctuate based on supply and demand.
Perspective on Financial Gain
While financial compensation can be a significant draw, it is rarely the sole motivator for participation, particularly in therapeutic trials. For many individuals facing challenging health conditions, the primary “lucrative” aspect is the potential for improved health outcomes or access to innovative treatments not otherwise available. The financial compensation, in this context, serves more as an alleviation of the burden associated with participation, rather than a primary incentive for enrolling. It’s a payment for time and inconvenience, not a salary.
Treating clinical trials as a quick path to “lucrative” income risks overlooking the serious medical research context. These are medical procedures, not employment opportunities. The primary purpose is to advance medical science, and while compensation is often provided, it should always be considered secondary to the research objectives and personal health considerations. Potential participants should approach these opportunities with a clear understanding of the commitment required, the potential personal risks, and the overarching goal of contributing to medical knowledge.