Mastering clinical research is a multi-faceted endeavor, demanding a systematic approach and an understanding of its intricate components. This guide aims to demystify the process, offering a foundational roadmap for navigating the complexities inherent in clinical investigations. It is not merely a collection of protocols, but a framework for cultivating the critical thinking and precision required for ethical and effective research.
Embarking on a clinical research journey requires a firm grasp of its underlying principles. Before a single data point is collected, a robust conceptual framework must be established. This section delves into the foundational elements upon which all sound clinical research is built.
Understanding Research Ethics
Ethical considerations are the bedrock of clinical research. Without a steadfast commitment to protecting participant welfare, any scientific endeavor loses its legitimacy. Informed consent, for instance, is not a mere formality but a dialogue ensuring participants comprehend the nature, risks, and benefits of their involvement.
- Autonomy and Informed Consent: Participants must be given sufficient information to make a voluntary and uncoerced decision about their involvement. This includes details about the study’s purpose, procedures, potential risks, and benefits. The process is continuous, not a one-time event, and participants retain the right to withdraw at any point.
- Beneficence and Non-maleficence: Research should maximize potential benefits to participants and society while minimizing harm. This ethical tightrope walk requires careful evaluation of risks versus potential rewards, ensuring that the burden placed on participants is justified by the scientific value of the research.
- Justice and Equity: The selection of research participants should be equitable, and the benefits and burdens of research should be distributed fairly across different populations. Vulnerable populations, such as children, prisoners, or individuals with cognitive impairments, require special protections.
Regulatory Landscape
Clinical research operates within a dense web of regulations designed to safeguard participants and ensure data integrity. Navigating this landscape is paramount to avoiding scientific and legal pitfalls.
- International Guidelines: Organizations like the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) provide globally accepted standards for the design, conduct, monitoring, auditing, recording, analyses, and reporting of clinical trials. The ICH-GCP (Good Clinical Practice) guideline is a cornerstone document within this framework.
- National Regulations: Each country typically has its own regulatory bodies, such as the Food and Drug Administration (FDA) in the United States or the European Medicines Agency (EMA) in the European Union. These bodies translate international guidelines into specific national requirements for drug and device development.
- Institutional Review Boards (IRBs)/Ethics Committees (ECs): These independent bodies review research protocols to protect the rights and welfare of human participants. Their approval is mandatory before any research involving human subjects can commence. They act as a critical gatekeeper, ensuring ethical principles are upheld.
Research Design and Methodology
The blueprint of any successful research project is its design. A well-conceived methodology determines the validity and reliability of the findings. This section explores the architectural elements of clinical research.
Formulating the Research Question
A clear and focused research question is the compass guiding the entire investigation. Without it, the research ship drifts aimlessly. It must be specific, measurable, achievable, relevant, and time-bound (SMART).
- PICO Framework: For clinical questions, the PICO framework (Patient/Population, Intervention, Comparison, Outcome) is a powerful tool for structuring research questions. It helps to define the core elements of the inquiry systematically.
- Hypothesis Generation: A research question often leads to the formulation of a testable hypothesis, a proposed explanation for an observed phenomenon. This hypothesis serves as the tentative answer to the research question and is what the study aims to prove or disprove.
Study Designs
Different research questions necessitate different study designs, each with its unique strengths and limitations. Selecting the appropriate design is crucial for generating credible evidence.
- Observational Studies: These studies observe participants without intervention. They are valuable for understanding disease patterns, risk factors, and natural histories.
- Cohort Studies: Groups of individuals are followed over time to see if exposure to certain factors leads to specific outcomes.
- Case-Control Studies: Individuals with a disease (cases) are compared to individuals without the disease (controls) to identify past exposures that may have contributed to the disease.
- Cross-Sectional Studies: Data are collected at a single point in time to assess the prevalence of a disease or exposure.
- Interventional Studies (Clinical Trials): These studies actively intervene to evaluate the effect of a treatment or intervention. They are considered the gold standard for establishing causality.
- Randomized Controlled Trials (RCTs): Participants are randomly assigned to an intervention group or a control group. Randomization minimizes bias and ensures comparability between groups.
- Non-Randomized Trials: Intervention is given to a group, but without randomization. These are often used when randomization is not ethical or feasible.
Data Management and Analysis
Data is the currency of clinical research. Its meticulous collection, rigorous management, and appropriate analysis are indispensable for extracting meaningful insights and generating valid conclusions.
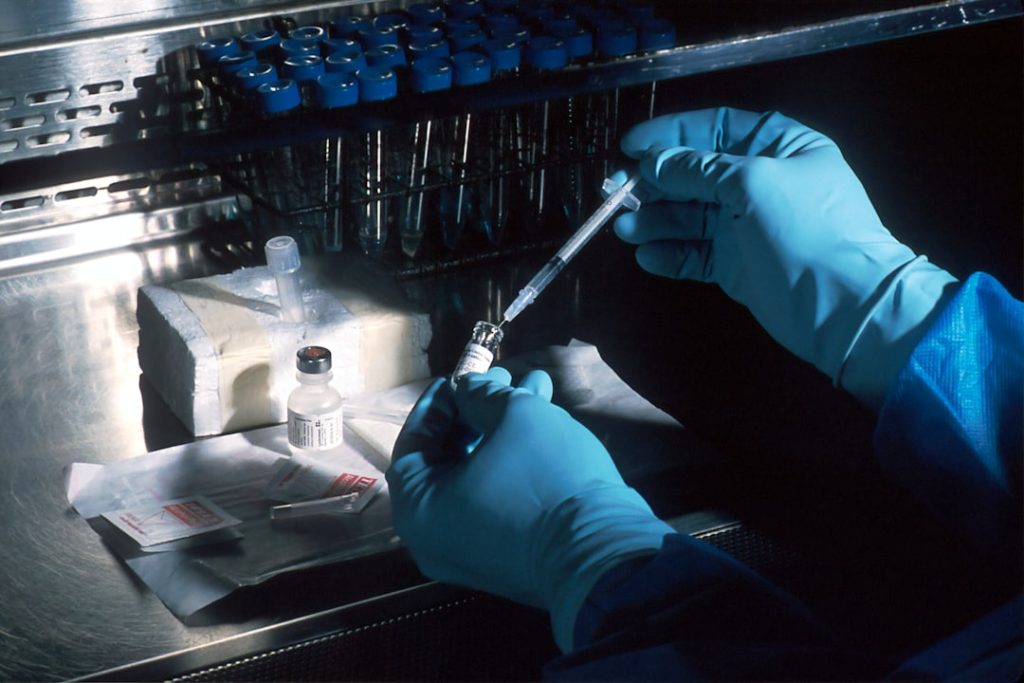
Data Collection Strategies
The quality of the data directly impacts the quality of the research. Robust data collection strategies are essential to minimize errors and ensure consistency.
- Case Report Forms (CRFs): Standardized documents used to collect data from each participant according to the protocol. They can be paper-based or electronic (eCRFs).
- Data Entry and Validation: Careful attention must be paid to accurate data entry, often involving double-entry methods or automated validation checks to identify and correct errors.
- Data Security and Privacy: Protecting participant data is not only an ethical imperative but also a legal requirement. Secure storage, anonymization, and adherence to data protection regulations (e.g., GDPR, HIPAA) are crucial.
Statistical Analysis
Statistics provide the tools to interpret data and draw inferences. The choice of statistical methods depends on the study design, type of data, and research question.
- Descriptive Statistics: Summarize and describe the main features of a dataset (e.g., means, medians, standard deviations, frequencies).
- Inferential Statistics: Allow researchers to make generalizations about a population based on a sample (e.g., t-tests, ANOVA, regression analysis).
- Sample Size Calculation: Before commencing a study, an adequate sample size must be determined to ensure sufficient statistical power to detect a clinically meaningful effect. An underpowered study is a wasted effort, like trying to catch a fish with a net full of holes.
- Statistical Software: Specialized software packages (e.g., SAS, R, SPSS, STATA) are used to perform complex statistical analyses.
Quality Assurance and Control

Maintaining the integrity and credibility of clinical research demands a continuous commitment to quality. This translates into systematic processes that proactively prevent errors and identify deviations from established protocols.
Monitoring and Auditing
These activities serve as a continuous oversight mechanism, ensuring that the research is conducted in accordance with the protocol, ethical guidelines, and regulatory requirements.
- Clinical Monitoring: Clinical research associates (CRAs) review study progress, verify data accuracy against source documents, ensure informed consent processes are followed, and address any protocol deviations. They are the eyes and ears of the sponsor at the research sites.
- Audits: Independent assessments of the research process and documentation to evaluate compliance with regulatory requirements and internal procedures. Audits are more formal and comprehensive than routine monitoring.
Quality Management Systems (QMS)
A robust QMS provides a structured framework for managing quality throughout the entire research lifecycle. It’s like the operating system for your research program, orchestrating all the moving parts.
- Standard Operating Procedures (SOPs): Detailed, written instructions for performing specific tasks consistently. SOPs are the recipe book for your research kitchen, ensuring every dish is prepared to the same standard.
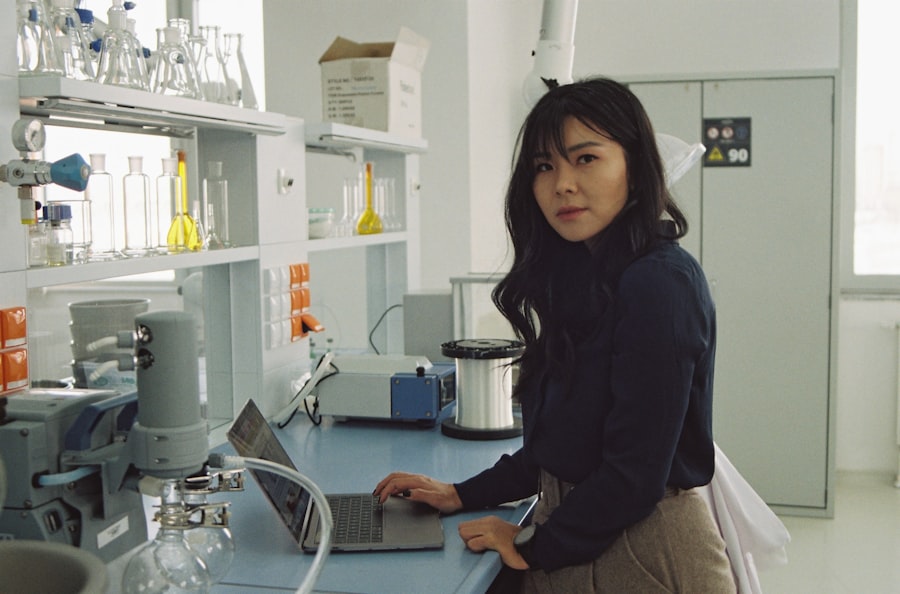
- Training and Competency: Ensuring that all personnel involved in the research are adequately trained and competent to perform their assigned tasks. Continuous education is vital in a rapidly evolving field.
- Documentation and Record Keeping: Meticulous documentation of all research activities, decisions, and data. Accurate and complete records are essential for demonstrating compliance, reproducing findings, and responding to inquiries.
Dissemination and Translation
| Metric | Details |
|---|---|
| Program Duration | 1 to 2 years (full-time) |
| Core Subjects | Clinical Trial Design, Biostatistics, Pharmacology, Regulatory Affairs, Ethics in Clinical Research |
| Eligibility | Bachelor’s degree in Life Sciences, Medicine, Pharmacy, or related field |
| Average Class Size | 20-40 students |
| Internship/Practical Training | 6 months to 1 year in clinical research organizations or hospitals |
| Career Opportunities | Clinical Research Associate, Data Manager, Regulatory Affairs Specialist, Clinical Trial Manager |
| Average Salary Range | 30,000 to 60,000 per annum (varies by country and experience) |
| Research Focus | Drug development, patient safety, clinical trial management, data analysis |
| Accreditation Bodies | ACRP (Association of Clinical Research Professionals), SOCRA (Society of Clinical Research Associates) |
The ultimate purpose of clinical research is to advance medical knowledge and improve patient care. This objective can only be realized through the effective dissemination of findings and their eventual translation into practice.
Publication and Presentation
Sharing research results with the scientific community is a moral and ethical obligation. Publication in peer-reviewed journals is the primary mechanism for disseminating new knowledge.
- Manuscript Preparation: Crafting a clear, concise, and accurate research manuscript that adheres to journal-specific guidelines. This includes a robust introduction, methods, results, and discussion section.
- Peer Review: The cornerstone of scientific publishing, where expert reviewers critically evaluate the manuscript for scientific rigor, validity, and ethical conduct. This process ensures the quality and credibility of published research.
- Conference Presentations: Opportunities to present preliminary or completed research findings to a wider audience, fostering discussion and collaboration within the scientific community.
Knowledge Translation
Moving research findings from the laboratory bench and clinical trial results into real-world clinical practice is a complex, multi-stage process. It’s about bridging the gap between discovery and impact.
- Guideline Development: Research findings often inform the development of clinical practice guidelines, providing evidence-based recommendations for healthcare professionals.
- Education and Training: Healthcare providers need to be educated about new research findings and their implications for patient care.
- Policy Changes: Significant research findings can influence healthcare policies, leading to changes in treatment algorithms, funding priorities, and public health initiatives. This is the ultimate goal, where the ripple effect of your work extends to impact entire populations.
Mastering clinical research is not a terminal destination but an ongoing journey of learning and refinement. It requires intellectual curiosity, meticulous attention to detail, unwavering ethical principles, and a commitment to scientific integrity. By embracing these tenets, you contribute to the advancement of medicine, ultimately impacting the lives of countless individuals.