The National Cancer Institute (NCI) plays a pivotal role in the landscape of cancer research, particularly through its extensive network of clinical trials. These trials are meticulously designed studies that evaluate new treatments, diagnostic methods, and preventive strategies for cancer. The NCI, as part of the National Institutes of Health (NIH), is dedicated to understanding cancer’s complexities and improving patient outcomes.
By conducting clinical trials, the NCI aims to translate laboratory discoveries into effective therapies that can be used in clinical practice. This process is essential for validating new approaches to cancer treatment and ensuring that they are both safe and effective for patients. Clinical trials under the NCI umbrella encompass a wide range of research initiatives, from early-phase studies that test new drugs or treatment combinations to late-phase trials that compare existing therapies.
Each trial is designed with specific objectives, such as determining the efficacy of a new medication or assessing the quality of life for patients undergoing a particular treatment regimen. The rigorous protocols established by the NCI ensure that these trials adhere to high scientific and ethical standards, ultimately contributing to the body of knowledge that informs cancer care.
Key Takeaways
- NCI clinical trials are essential for developing new cancer treatments and improving patient outcomes.
- These trials follow rigorous protocols to ensure safety and scientific validity.
- Participant involvement is crucial for the success and advancement of cancer research.
- Ethical standards guide the conduct of NCI clinical trials to protect participants.
- Emerging trends in NCI trials focus on personalized medicine and innovative therapies.
The Importance of NCI Clinical Trials in Advancing Medical Research
NCI clinical trials are crucial for advancing medical research, particularly in the field of oncology. They serve as a bridge between laboratory research and clinical application, allowing scientists to test hypotheses in real-world settings. The data generated from these trials not only enhances our understanding of cancer biology but also informs the development of new therapeutic strategies.
For instance, the identification of specific genetic mutations in tumors has led to targeted therapies that can significantly improve patient outcomes. Clinical trials are essential for validating these innovative approaches and ensuring they are effective across diverse patient populations. Moreover, NCI clinical trials contribute to the establishment of evidence-based guidelines for cancer treatment.
By systematically evaluating the safety and efficacy of new interventions, these trials provide the necessary data to support clinical decision-making. This is particularly important in an era where personalized medicine is becoming increasingly prevalent. As researchers uncover the genetic and molecular underpinnings of various cancers, clinical trials help determine which treatments are most effective for specific patient subgroups.
This not only enhances treatment efficacy but also minimizes unnecessary side effects, ultimately leading to improved quality of life for patients.
How NCI Clinical Trials Work
The operation of NCI clinical trials is a complex process that involves multiple phases, each with distinct objectives and methodologies. Typically, clinical trials are categorized into four phases: Phase I trials focus on assessing safety and dosage; Phase II trials evaluate efficacy and side effects; Phase III trials compare new treatments with standard therapies; and Phase IV trials monitor long-term effects after a treatment has been approved. Each phase is designed to answer specific research questions while ensuring participant safety throughout the process.
Before a trial can commence, it undergoes a rigorous review process that includes approval from institutional review boards (IRBs) to ensure ethical standards are met. Once approved, participants are recruited based on specific eligibility criteria, which may include factors such as age, cancer type, stage of disease, and previous treatment history. Informed consent is a critical component of this process, ensuring that participants understand the potential risks and benefits associated with their involvement in the trial.
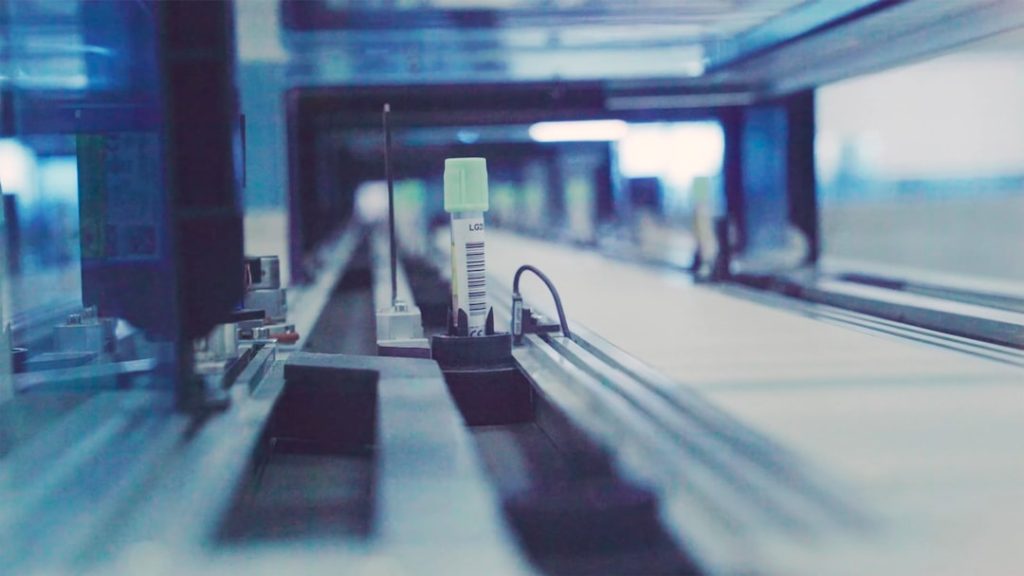
Throughout the trial, data is meticulously collected and analyzed to assess outcomes, with regular monitoring to ensure participant safety and adherence to the study protocol.
The Impact of NCI Clinical Trials on Cancer Treatment
The impact of NCI clinical trials on cancer treatment is profound and far-reaching. These trials have led to significant breakthroughs in oncology, resulting in the approval of numerous therapies that have transformed patient care. For example, the development of immunotherapy has been largely driven by findings from clinical trials that demonstrated the ability of certain drugs to harness the body’s immune system to fight cancer.
Agents such as checkpoint inhibitors have revolutionized treatment paradigms for melanoma and lung cancer, offering hope to patients who previously had limited options. Additionally, NCI clinical trials have played a critical role in establishing standard treatment protocols for various cancers. The results from large-scale Phase III trials often lead to changes in clinical practice guidelines, influencing how oncologists approach treatment decisions.
For instance, the use of adjuvant chemotherapy following surgery for breast cancer was solidified through evidence gathered from clinical trials demonstrating improved survival rates. Such advancements underscore the importance of ongoing research and the need for continued investment in clinical trial infrastructure to facilitate future discoveries.
The Role of Participants in NCI Clinical Trials
| Metric | Description | Value | Source |
|---|---|---|---|
| Number of Active Trials | Total number of ongoing clinical trials registered with NCI | 1,200+ | NCI Clinical Trials Database |
| Trial Phases | Distribution of trials by phase | Phase 1: 25%, Phase 2: 40%, Phase 3: 30%, Phase 4: 5% | NCI Clinical Trials Database |
| Enrollment Size | Average number of participants per trial | 150 participants | NCI Clinical Trials Reports |
| Common Cancer Types Studied | Most frequently studied cancers in NCI trials | Lung, Breast, Prostate, Colorectal | NCI Clinical Trials Database |
| Trial Locations | Number of trial sites across the US | 500+ | NCI Clinical Trials Network |
| Trial Completion Rate | Percentage of trials completed as planned | 70% | NCI Annual Report |
Participants are at the heart of NCI clinical trials, serving as essential contributors to the advancement of cancer research. Their involvement not only helps researchers gather critical data but also provides participants with access to cutting-edge treatments that may not yet be available through standard care pathways. Many individuals choose to participate in clinical trials out of a desire to contribute to scientific knowledge or to help others facing similar challenges.
This altruistic motivation is often coupled with the hope that they may benefit personally from novel therapies being tested. The experience of participating in an NCI clinical trial can vary significantly depending on the study design and individual circumstances. Participants may undergo additional monitoring and assessments compared to standard treatment protocols, which can provide valuable insights into their health status and treatment response.
However, it is essential for participants to be fully informed about what participation entails, including potential risks and benefits. The informed consent process is designed to ensure that individuals understand their rights and responsibilities throughout the trial, fostering an environment of transparency and trust between researchers and participants.
Ethical Considerations in NCI Clinical Trials

Ethical considerations are paramount in the conduct of NCI clinical trials, given the vulnerable population involved—cancer patients seeking new treatment options. The principles of respect for persons, beneficence, and justice guide ethical decision-making in research involving human subjects. Researchers must ensure that participants are treated with dignity and that their autonomy is respected throughout the trial process.
This includes providing comprehensive information about the study’s purpose, procedures, potential risks, and alternative treatment options. In addition to informed consent, ongoing ethical oversight is critical during the trial’s duration. Institutional review boards (IRBs) play a vital role in reviewing study protocols to ensure participant safety and ethical compliance.
They monitor adverse events and assess whether the potential benefits of the research outweigh any risks involved. Furthermore, researchers must be vigilant about maintaining confidentiality and protecting sensitive patient information throughout the study. These ethical frameworks are essential for fostering public trust in clinical research and ensuring that participants feel safe and valued during their involvement.
Current and Future Trends in NCI Clinical Trials
The landscape of NCI clinical trials is continually evolving, driven by advancements in technology and a deeper understanding of cancer biology. One notable trend is the increasing use of precision medicine approaches in clinical trial design. By leveraging genomic profiling and molecular characterization of tumors, researchers can identify specific biomarkers that predict treatment response.
This shift towards personalized therapies allows for more targeted interventions that are tailored to individual patients’ unique cancer profiles. Another emerging trend is the integration of digital health technologies into clinical trials. Remote monitoring tools, telemedicine consultations, and mobile health applications are being utilized to enhance patient engagement and streamline data collection processes.
These innovations not only improve accessibility for participants but also facilitate real-time monitoring of treatment responses and side effects. As technology continues to advance, it is likely that NCI clinical trials will increasingly incorporate these tools to enhance efficiency and improve patient experiences.
The Future of NCI Clinical Trials in Advancing Medical Research
As we look toward the future, NCI clinical trials will remain a cornerstone of cancer research and treatment innovation. The ongoing commitment to rigorous scientific inquiry combined with ethical considerations will ensure that these trials continue to yield valuable insights into cancer biology and therapy effectiveness. With advancements in technology and a growing emphasis on personalized medicine, the potential for breakthroughs in cancer treatment is greater than ever before.
The collaborative efforts among researchers, healthcare providers, patients, and regulatory bodies will be essential in shaping the future landscape of NCI clinical trials. By fostering an environment that encourages participation and prioritizes patient safety, we can continue to make significant strides in understanding cancer and improving outcomes for those affected by this disease. The journey from bench to bedside is complex but vital; through continued investment in clinical research, we can aspire to transform cancer care for generations to come.