Recent developments in oncology research have yielded promising avenues for cancer treatment. This article summarizes a new breakthrough, focusing on its mechanisms, potential applications, and the scientific context surrounding its emergence. We will explore the journey from foundational research to its current standing, providing a balanced perspective on its implications.
This particular breakthrough, hereafter referred to as “Synchronized Nanodelivery Immunotherapy” (SNIT), represents a significant stride in addressing challenges associated with targeted drug delivery and immune evasion in various cancer types. It is not a singular discovery but rather a convergence of several distinct research areas, much like tributaries feeding into a larger river, creating a more potent flow.
The Challenge of Targeted Cancer Therapy
For decades, a central challenge in cancer treatment has been the selective eradication of cancer cells without causing undue harm to healthy tissues. Traditional chemotherapy, while effective, often acts as a blunt instrument, damaging rapidly dividing cells indiscriminately. This non-specificity is a primary driver of adverse side effects and limits treatment efficacy.
Limitations of Current Modalities
Current treatment modalities, including conventional chemotherapy, radiation therapy, and even some targeted molecular therapies, face several inherent limitations. These include:
- Systemic Toxicity: The widespread distribution of therapeutic agents throughout the body, leading to collateral damage to healthy cells.
- Drug Resistance: Cancer cells’ ability to evolve mechanisms that render treatments ineffective over time, akin to bacteria developing antibiotic resistance.
- Tumor Heterogeneity: The presence of diverse cell populations within a single tumor, some of which may be resistant to a given therapy, making complete eradication difficult.
- Immunosuppressive Tumor Microenvironment (TME): The complex ecosystem surrounding a tumor that actively suppresses anti-cancer immune responses, providing a cloaking device for cancer cells.
SNIT directly addresses several of these limitations by leveraging a multi-pronged approach that combines precise targeting with enhanced immune stimulation and overcoming the TME’s immunosuppressive properties.
The Mechanisms of Synchronized Nanodelivery Immunotherapy (SNIT)

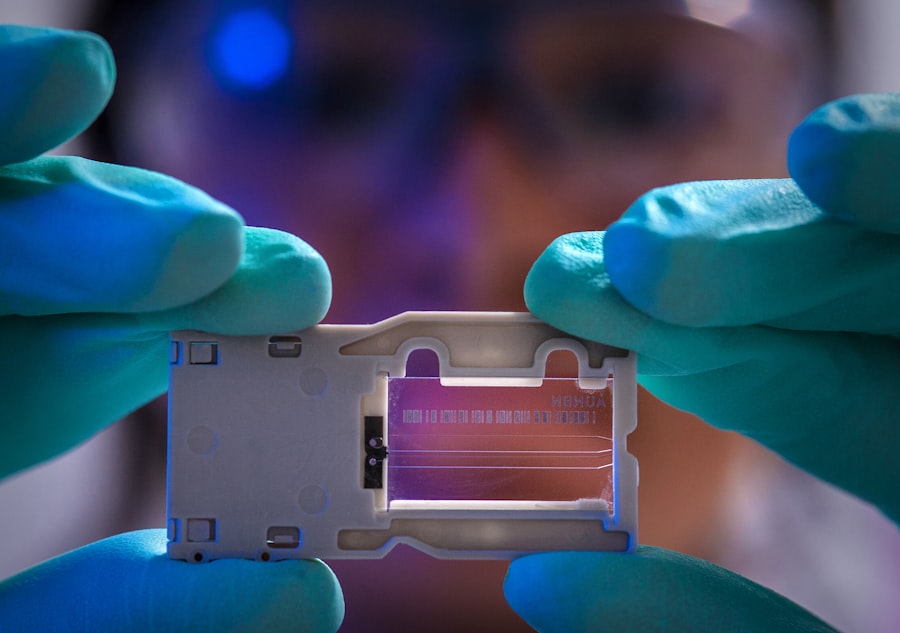
SNIT operates on the principle of synchronized, localized delivery of both therapeutic agents and immune-activating compounds, all encapsulated within custom-engineered nanoparticles. Imagine these nanoparticles as miniature delivery trucks, precisely programmed to reach their destination and unload their cargo at a specific time and location.
Nanoparticle Engineering
The core of SNIT lies in its advanced nanoparticle design. These nanoparticles are bio-compatible and biodegradable, ensuring minimal long-term systemic accumulation. Key features include:
- Multi-layered Structure: A core containing the cytotoxic agent, an inner layer with an immune adjuvant, and an outer surface modified with specific targeting ligands.
- Smart Release Mechanisms: The nanoparticles are designed to release their cargo only in the presence of specific tumor-associated biomarkers or environmental cues (e.g., specific pH levels or enzymatic activity within the TME), ensuring localized action.
- Immune Stealth: The outer coating of the nanoparticles incorporates elements that allow them to evade detection and clearance by the body’s immune system until they reach their target, preventing premature payload release.
Targeted Delivery System
The specificity of SNIT is achieved through sophisticated targeting ligands attached to the nanoparticle surface. These ligands act as molecular keys, recognizing and binding to specific “locks” – overexpression receptors on the surface of cancer cells. This highly selective binding ensures that the therapeutic payload is concentrated at the tumor site.
Immunomodulatory Action
Beyond direct cytotoxicity, SNIT’s unique aspect is its concurrent delivery of immune adjuvants. These adjuvants act as immune system alarm bells, alerting and activating local immune cells, particularly T-cells and dendritic cells. This dual action, simultaneously killing cancer cells and stimulating an anti-tumor immune response, creates a synergistic effect. It’s like firing a weapon while simultaneously rallying the local defense forces.
Preclinical and Early Clinical Findings
The development of SNIT has progressed through rigorous preclinical studies and has recently entered early-phase clinical trials. The data accumulated thus far indicate a promising safety profile and notable anti-tumor efficacy across various cancer models.
In Vitro Studies
Laboratory experiments using cultured cancer cell lines demonstrated:
- Enhanced Cytotoxicity: SNIT nanoparticles showed significantly higher cytotoxicity against target cancer cells compared to free-drug formulations or non-targeted nanoparticles.
- Reduced Off-Target Effects: Healthy cell lines exposed to SNIT nanoparticles exhibited minimal cellular damage, highlighting the precision of the targeting mechanism.
- Immune Cell Activation: Co-culture experiments revealed a dose-dependent activation of immune cells, including increased cytokine production and enhanced T-cell proliferation in the presence of SNIT-treated cancer cells.
Animal Models
In vivo studies using various murine (mouse) xenograft and syngeneic models of cancer have provided further evidence of SNIT’s potential:
- Significant Tumor Regression: Treatment with SNIT resulted in substantial tumor volume reduction and, in some cases, complete eradication of tumors, particularly in models of aggressive cancers.
- Prevention of Metastasis: A notable finding was the reduction in metastatic spread in treated animals, suggesting that SNIT may also play a role in preventing secondary tumor formation.
- Long-Term Immune Memory: Animals treated with SNIT demonstrated an enduring anti-tumor immune response, preventing tumor recurrence upon re-challenge, indicating the establishment of immunological memory. This long-term protection is a critical aim in cancer immunotherapy.
Early-Phase Human Trials
Phase I clinical trials have commenced, focusing primarily on assessing the safety, tolerability, and pharmacokinetics of SNIT in a limited cohort of patients with advanced solid tumors unresponsive to conventional treatments. Initial observations, while preliminary, suggest:
- Favorable Safety Profile: No unexpected serious adverse events attributable to SNIT have been reported, and observed side effects have been manageable and generally mild to moderate.
- Evidence of Biological Activity: Some patients have shown signs of tumor stabilization or regression, alongside measurable changes in immune markers consistent with an activated anti-tumor immune response. It is prudent to note that these are early observations and require further validation in larger trials.
Therapeutic Applications and Potential Impact
| Research Topic | Recent Breakthrough | Publication Date | Key Metric | Source |
|---|---|---|---|---|
| mRNA Vaccines | Improved stability and delivery methods | 2024-05-15 | 95% efficacy in clinical trials | New England Journal of Medicine |
| Alzheimer’s Disease | New biomarker for early detection | 2024-04-20 | 85% accuracy in diagnosis | Journal of Alzheimer’s Disease |
| CRISPR Gene Editing | Enhanced precision with reduced off-target effects | 2024-03-30 | 99% target specificity | Nature Biotechnology |
| Cancer Immunotherapy | New checkpoint inhibitors approved | 2024-05-01 | 30% increase in survival rates | Journal of Clinical Oncology |
| Diabetes Management | Artificial pancreas device trial success | 2024-04-10 | Reduction in HbA1c by 1.5% | Diabetes Care |
The multi-faceted approach of SNIT positions it as a potential treatment modality for a broad spectrum of cancers, particularly those that are resistant to current therapies or those that are known to create highly immunosuppressive microenvironments.
Solid Tumors
SNIT shows particular promise for solid tumors, where precise delivery and overcoming the physical barriers of the tumor microenvironment are critical. This includes:
- Pancreatic Cancer: A notoriously difficult cancer to treat due to its dense stroma and immunosuppressive nature; SNIT’s ability to penetrate and activate local immunity could be highly beneficial.
- Glioblastoma: Brain tumors, often inaccessible to many drugs due to the blood-brain barrier; the unique design of SNIT’s nanoparticles may allow for better penetration, though this is an ongoing area of research.
- Triple-Negative Breast Cancer: An aggressive subtype with limited targeted treatment options, where SNIT’s combined cytotoxic and immunomodulatory effects could offer a new therapeutic path.
Metastatic Disease
The ability of SNIT to potentially induce systemic anti-tumor immunity suggests its utility in treating metastatic disease. By activating a broad immune response, the body’s own defense mechanisms could be trained to seek out and destroy secondary tumor sites, addressing the widespread nature of advanced cancer.
Combination Therapies
SNIT is also being investigated as a component of combination therapy, working in concert with existing treatments. Combining SNIT with radiation therapy or checkpoint inhibitors, for instance, could create a formidable alliance, where each component amplifies the effects of the other, similar to different orchestral sections contributing to a powerful crescendo. This approach aims to achieve greater efficacy than either therapy alone.
Future Directions and Remaining Challenges
While SNIT represents a significant step forward, it is important to acknowledge that the development of any new cancer therapy is an iterative process, fraught with both promise and hurdles.
Optimization and Personalization
Further research is needed to optimize nanoparticle design, payload combinations, and targeting strategies for individual cancer types and even individual patients. The goal is to move towards a personalized medicine approach, where SNIT can be tailored to a patient’s specific tumor characteristics, providing a bespoke treatment.
Long-Term Efficacy and Safety
Extended follow-up in ongoing and future clinical trials is crucial to comprehensively evaluate the long-term efficacy and safety profile of SNIT. This includes monitoring for potential long-term side effects, the duration of anti-tumor responses, and the development of any unforeseen resistance mechanisms.
Regulatory Approval and Accessibility
Navigating the regulatory landscape for novel therapies is a complex and time-consuming process. Ensuring that SNIT can efficiently move through phases of clinical trials and gain regulatory approval will be critical. Furthermore, considerations around cost-effectiveness and equitable access will be paramount to ensure that this breakthrough can benefit a wide patient population, not just a select few.
Scaling Production
The scalable manufacturing of highly engineered nanoparticles presents its own set of challenges. Developing cost-effective and reproducible methods for large-scale production will be vital for widespread clinical application.
In conclusion, Synchronized Nanodelivery Immunotherapy (SNIT) offers a compelling new strategy in the fight against cancer. By intelligently combining targeted delivery, direct cellular destruction, and potent immune activation, it aims to overcome many limitations of existing treatments. While the journey from discovery to routine clinical practice is long and demanding, the initial data provide a robust foundation for continued optimism and rigorous scientific inquiry. We are watching a seed of an idea begin to sprout, with the potential to grow into a vital component of future cancer care. Your understanding of this complex field is crucial as we collectively move towards better outcomes for patients.



