Clinical trials are pivotal in advancing medical knowledge and treatment options, particularly in the realm of oncology. At the heart of these trials is the Principal Investigator (PI), a key figure responsible for overseeing the study’s design, implementation, and adherence to regulatory standards. The PI ensures that the trial is conducted ethically and that the data collected is reliable and valid.
This role is not only crucial for the integrity of the research but also for the safety and well-being of the participants involved. The PI coordinates a multidisciplinary team, including researchers, nurses, and data analysts, to facilitate the trial’s progress and address any challenges that may arise. The significance of the PI extends beyond mere administration; they are often the driving force behind innovative treatment approaches.
In cancer research, where therapies can be complex and multifaceted, the PI’s expertise in both clinical practice and research methodology is essential. They must navigate a landscape filled with regulatory requirements, ethical considerations, and scientific rigor while maintaining a focus on patient care. This balance is particularly critical in oncology, where the stakes are high, and the potential for breakthroughs can lead to life-saving treatments for patients facing dire prognoses.
Key Takeaways
- The Principal Investigator oversees the clinical trial to ensure safety and scientific integrity.
- The new cancer treatment offers innovative approaches targeting specific cancer types.
- Eligibility criteria determine which patients can enroll based on health and medical history.
- Participants may experience potential benefits but also face risks and side effects.
- Patients share personal testimonials highlighting their experiences and outcomes in the trial.
Understanding the New Cancer Treatment
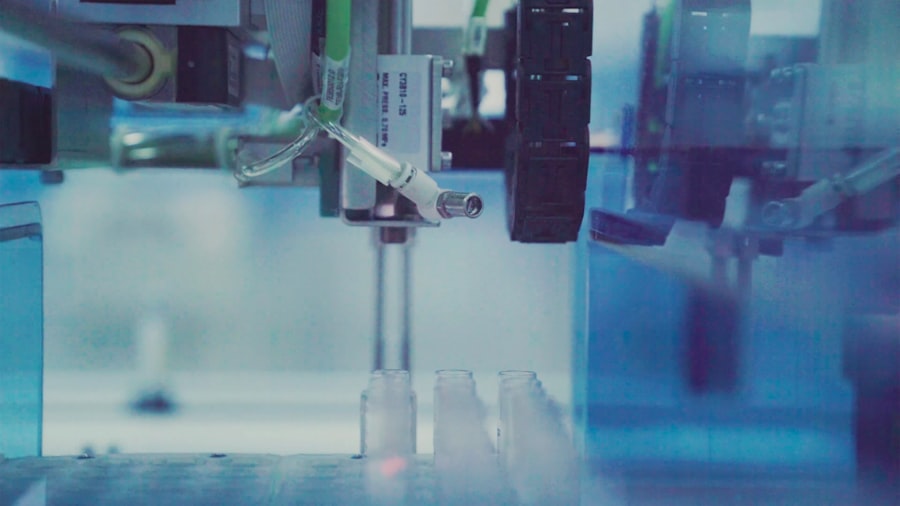
The new cancer treatment under investigation in this clinical trial represents a novel approach to combating malignancies that have proven resistant to conventional therapies. This treatment may involve innovative mechanisms such as targeted therapy, immunotherapy, or gene editing techniques like CRISPR. For instance, targeted therapies aim to exploit specific genetic mutations within cancer cells, allowing for a more personalized treatment strategy that minimizes damage to healthy tissues.
By focusing on the unique characteristics of an individual’s tumor, these therapies can enhance efficacy while reducing side effects commonly associated with traditional chemotherapy. Immunotherapy, another promising avenue in cancer treatment, harnesses the body’s immune system to identify and destroy cancer cells. This approach has shown remarkable success in certain types of cancer, such as melanoma and lung cancer, where immune checkpoint inhibitors have led to significant improvements in patient outcomes.
The clinical trial may explore a combination of these strategies or introduce a completely new agent designed to enhance immune response or target specific tumor markers. Understanding the underlying science of these treatments is crucial for potential participants, as it informs their decision-making process regarding enrollment and participation.
Eligibility and Enrollment Criteria for the Clinical Trial

Eligibility criteria for clinical trials are meticulously designed to ensure that participants are suitable for the study while also safeguarding their health and safety. These criteria often include specific factors such as age, gender, type and stage of cancer, previous treatments received, and overall health status. For instance, a trial investigating a new immunotherapy might require participants to have a confirmed diagnosis of a particular cancer type that has not responded to standard treatments.
Additionally, patients may need to meet certain laboratory values or performance status scores to ensure they can tolerate the experimental treatment. Enrollment processes typically involve comprehensive screening procedures that may include medical history reviews, physical examinations, and diagnostic tests such as imaging studies or biopsies. This thorough vetting process helps to identify individuals who are most likely to benefit from the new treatment while minimizing risks associated with participation.
Furthermore, informed consent is a critical component of enrollment; potential participants must be fully educated about the trial’s purpose, procedures, potential risks, and benefits before agreeing to take part. This transparency fosters trust between researchers and participants and ensures that individuals are making informed decisions about their involvement.
Potential Benefits and Risks of the Treatment
Participating in a clinical trial can offer several potential benefits for patients with cancer. One of the most significant advantages is access to cutting-edge treatments that are not yet available through standard care pathways. For patients with limited options due to advanced disease or treatment resistance, enrolling in a trial may provide an opportunity for improved outcomes or even remission.
Additionally, participants often receive close monitoring and care from a dedicated team of healthcare professionals who are focused on their well-being throughout the study. However, it is essential to recognize that participation in clinical trials also carries inherent risks. Experimental treatments may lead to unforeseen side effects or adverse reactions that are not fully understood at the outset.
Patients may experience symptoms ranging from mild discomfort to severe complications depending on how their bodies respond to the new therapy. Moreover, there is no guarantee that the treatment will be effective; some participants may not experience any benefit at all. Understanding these potential risks is crucial for patients as they weigh their options and consider whether participation aligns with their personal health goals and values.
Patient Experience and Testimonials
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Number of Clinical Trials Led | Total count of clinical trials where the investigator is the principal investigator (PI) | 1 – 50+ | Indicates experience and leadership in clinical research |
| Trial Phases Managed | Phases of clinical trials the PI has managed (Phase I, II, III, IV) | Phase I – IV | Shows breadth of expertise across different trial stages |
| Patient Enrollment Rate | Average number of patients enrolled per trial per month | 5 – 50 patients/month | Reflects efficiency in recruiting participants |
| Trial Completion Rate | Percentage of trials completed successfully under the PI | 70% – 100% | Measures ability to see trials through to completion |
| Regulatory Compliance | Number of audits passed without major findings | 90% – 100% | Indicates adherence to regulatory standards and quality |
| Publication Count | Number of peer-reviewed publications resulting from PI-led trials | 0 – 30+ | Demonstrates contribution to scientific knowledge |
| Average Trial Duration | Average length of time to complete a clinical trial (months) | 6 – 36 months | Impacts speed of bringing treatments to market |
The patient experience within clinical trials can vary widely based on individual circumstances and the nature of the treatment being studied. Many participants report feeling empowered by their involvement in research that could potentially benefit future patients facing similar challenges. Testimonials from individuals who have participated in clinical trials often highlight feelings of hope and purpose as they contribute to advancing medical knowledge.
For example, one participant might share how being part of a trial provided them with access to a promising new therapy that significantly improved their quality of life during treatment. Conversely, some patients may encounter challenges during their trial experience, including managing side effects or navigating complex treatment protocols. These experiences underscore the importance of robust support systems within clinical trials.
Healthcare teams play a vital role in providing education, emotional support, and resources to help patients cope with the demands of participation. Sharing stories from past participants can serve as an invaluable resource for prospective enrollees, offering insights into what they might expect throughout their journey in the trial.
The Role of the Principal Investigator in the Clinical Trial
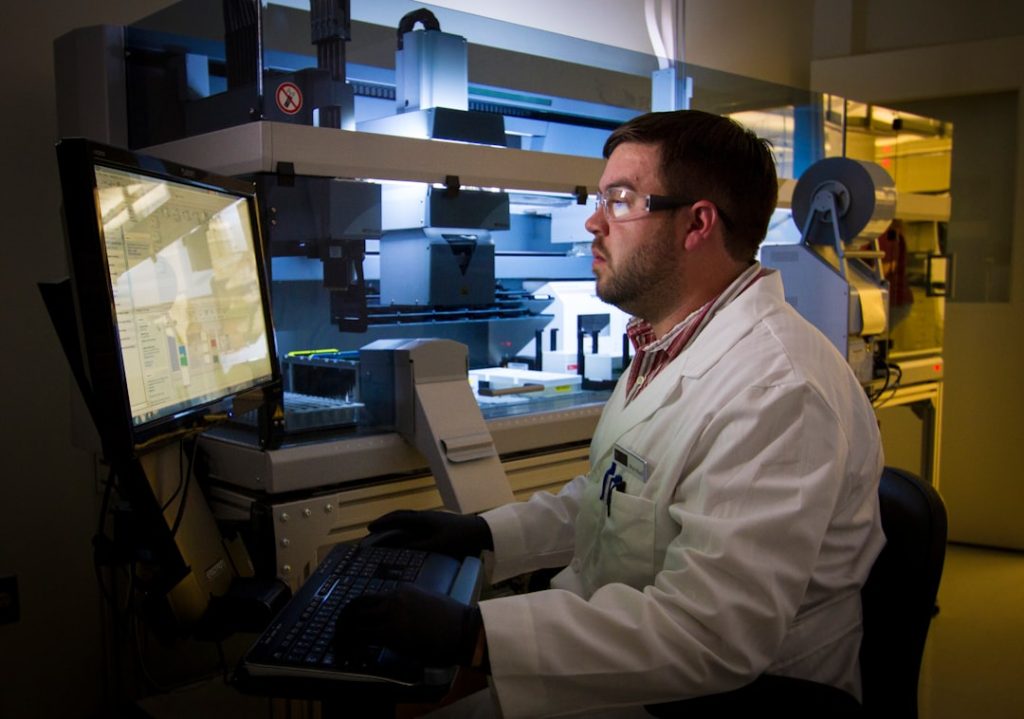
The Principal Investigator serves as the cornerstone of any clinical trial, embodying both leadership and accountability throughout the research process. Their responsibilities encompass a wide range of tasks, from designing the study protocol to ensuring compliance with ethical standards and regulatory requirements. The PI must possess a deep understanding of both the scientific principles underlying the research and the practical aspects of patient care.
This dual expertise allows them to make informed decisions regarding study design modifications or patient management strategies as needed. Moreover, effective communication is paramount for a Principal Investigator. They must engage with various stakeholders, including regulatory bodies, funding agencies, and institutional review boards (IRBs), while also fostering collaboration among team members involved in the trial.
The PI often serves as a mentor to junior researchers and staff, guiding them through complex processes and encouraging professional development within the field. Their leadership not only shapes the trajectory of the trial but also influences the broader landscape of cancer research by contributing valuable data that can inform future studies.
Future Implications and Research Opportunities
The outcomes of clinical trials led by Principal Investigators can have far-reaching implications for cancer treatment paradigms. Successful trials may lead to new standards of care that redefine how specific cancers are treated or managed. For instance, if a novel immunotherapy demonstrates significant efficacy in a clinical trial setting, it could pave the way for its approval by regulatory agencies like the FDA, ultimately making it accessible to a broader patient population.
Such advancements can shift clinical practice guidelines and influence how oncologists approach treatment planning for their patients. Furthermore, clinical trials often generate valuable data that can inform future research directions. Insights gained from participant responses can lead to new hypotheses about disease mechanisms or treatment combinations worth exploring in subsequent studies.
The iterative nature of clinical research means that each trial builds upon previous findings, creating a cumulative body of knowledge that drives innovation in cancer care. As researchers continue to explore novel therapies and refine existing ones, opportunities for collaboration across disciplines will likely emerge, fostering an environment ripe for groundbreaking discoveries.
How to Get Involved in the Clinical Trial
For patients interested in participating in clinical trials, several avenues exist for finding relevant studies that align with their health needs and preferences. One effective approach is consulting with healthcare providers who can offer guidance on available trials based on individual medical history and current treatment options. Oncologists often have access to databases listing ongoing studies and can provide insights into which trials may be appropriate for their patients.
Additionally, online resources such as ClinicalTrials.gov serve as comprehensive platforms where individuals can search for trials by location, condition, or intervention type. These databases provide essential information about eligibility criteria, study locations, and contact details for research teams overseeing each trial. Engaging with patient advocacy groups can also be beneficial; these organizations often have resources dedicated to helping patients navigate clinical trial opportunities while providing support throughout their journey.
In conclusion, understanding the multifaceted aspects of clinical trials—particularly those led by Principal Investigators—can empower patients facing cancer diagnoses to make informed decisions about their treatment options. By exploring eligibility criteria, weighing potential benefits against risks, and considering personal experiences shared by others who have participated in trials, individuals can take proactive steps toward engaging with cutting-edge research that may ultimately enhance their health outcomes.