You are now reading an overview of recent developments in neurological research. This article aims to summarize key findings and ongoing investigations across various facets of neurological science, providing a snapshot of the current landscape without extensive elaboration.
Neurodegenerative diseases represent a significant challenge in modern medicine, progressively impairing neuronal function and leading to severe disability. Recent research has focused on understanding underlying mechanisms and developing new therapeutic strategies.
Alzheimer’s Disease (AD)
Alzheimer’s disease remains a focal point of neurodegenerative research, with ongoing investigations into its complex pathophysiology. The amyloid cascade hypothesis, while continually refined, still serves as a foundational model for many studies.
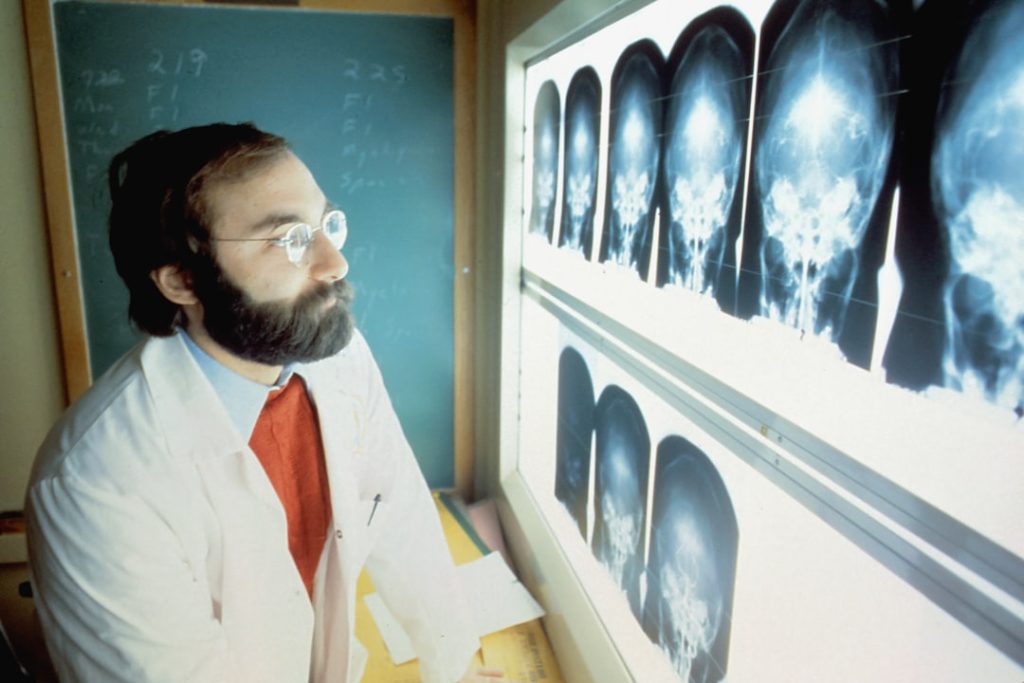
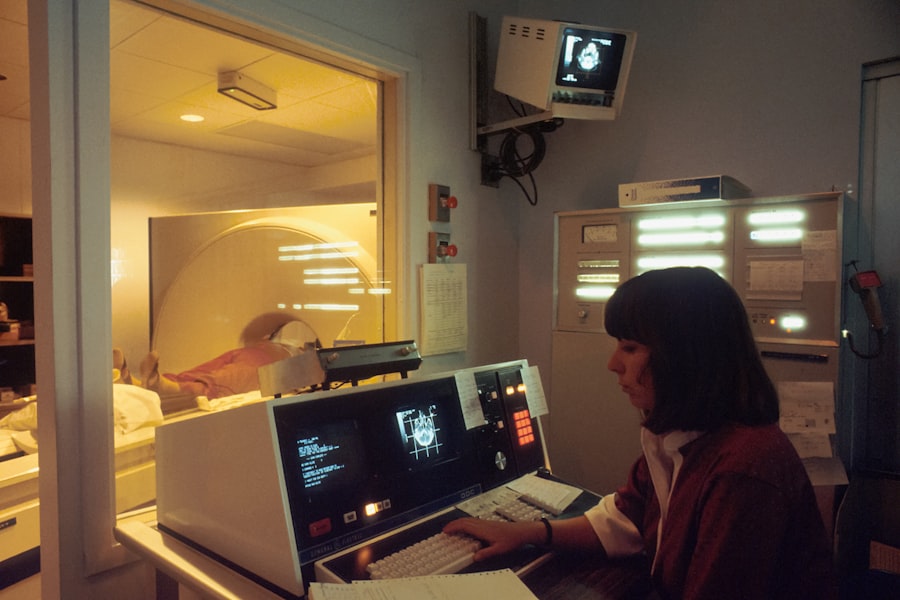
- Amyloid-beta and Tau Pathology: Research continues to explore the interplay between amyloid-beta plaques and neurofibrillary tangles composed of hyperphosphorylated tau protein. Recent imaging studies, utilizing PET scans with novel tracers, are providing clearer insights into the spatial and temporal progression of these pathologies in living individuals. For instance, some studies indicate that tau pathology may closely track clinical decline more effectively than amyloid-beta accumulation in later stages of the disease.
- Genetic Risk Factors and Biomarkers: The role of genetic factors, such as APOE4 allele, is being further elucidated. Genome-wide association studies (GWAS) are identifying new genetic loci associated with increased AD risk, opening avenues for precision medicine approaches. Furthermore, the search for robust fluid biomarkers, particularly in blood, continues to accelerate. Plasma amyloid-beta ratios and phosphorylated tau levels show promise for early detection and monitoring disease progression, potentially enabling intervention before extensive neuronal damage occurs.
- Therapeutic Development: A new wave of monoclonal antibodies targeting amyloid-beta has shown modest clinical benefits in reducing cognitive decline in early AD stages. These agents, acting as molecular sweepers, aim to clear amyloid plaques from the brain. Concurrently, drugs targeting tau phosphorylation, aggregation, and spread are in various phases of clinical trials. Other strategies include neuroinflammation modulation, synaptic plasticity enhancers, and mitochondrial dysfunction correction. However, the multifaceted nature of AD suggests a single-target approach may be insufficient, leading to interest in combination therapies.
Parkinson’s Disease (PD)
Parkinson’s disease, characterized by motor symptoms such as tremor, rigidity, and bradykinesia, profoundly impacts patients’ quality of life. Research is expanding beyond dopaminergic pathway deficiencies.
- Alpha-synuclein and Lewy Bodies: The misfolding and aggregation of alpha-synuclein protein into Lewy bodies are central to PD pathology. Studies are investigating how alpha-synuclein spreads through the brain, akin to a slow-burning fire, potentially propagating from cell to cell. This prion-like hypothesis is guiding the development of therapies aimed at inhibiting alpha-synuclein aggregation or clearance.
- Genetic Contributions: Genetic mutations in genes like LRRK2 and GBA are known to increase PD risk. Research is exploring how these genetic variations contribute to cellular dysfunction, such as impaired lysosomal function or mitochondrial stress. These insights are informing the development of targeted small-molecule inhibitors for specific genetic subtypes of PD.
- Non-motor Symptoms: Increasingly, research recognizes the significant impact of non-motor symptoms such as sleep disorders, olfactory dysfunction, and cognitive impairment in PD. These symptoms can precede motor manifestations by years, offering potential windows for early diagnosis and intervention. Studies are exploring the neurobiological basis of these non-motor features, often involving widespread neurotransmitter system changes beyond dopamine.
- Advanced Therapies: Deep Brain Stimulation (DBS) remains a cornerstone for advanced PD, with ongoing evolution in targeting strategies and adaptive stimulation techniques. Gene therapies, aimed at delivering neurotrophic factors or modifying enzyme activity, are also under investigation, offering the potential for sustained therapeutic effects.
Stroke Research and Rehabilitation
Stroke remains a leading cause of long-term disability worldwide. Recent advancements focus on acute intervention, neuroprotection, and a more robust understanding of recovery mechanisms.
Acute Stroke Management
Timely and effective intervention during the acute phase of stroke is paramount for minimizing brain damage.
- Thrombolysis and Thrombectomy: Improvements in intravenous thrombolysis (e.g., using alteplase or tenecteplase) and endovascular thrombectomy have revolutionized acute ischemic stroke care. Research continues to refine patient selection criteria, optimize treatment windows (extending therapy to patients with larger vessel occlusions and favorable imaging profiles), and improve workflow efficiencies within stroke centers. Multimodal imaging, such as CT perfusion and MRI diffusion/perfusion, plays a critical role in guiding these decisions.
- Neuroprotection Strategies: While clinical trials for standalone neuroprotective agents have largely been unsuccessful, research continues to explore combination therapies or novel approaches to protect neurons from ischemic injury. This includes investigating hypothermia, free radical scavengers, and glutamate receptor antagonists, often in conjunction with reperfusion strategies. The challenge lies in translating promising preclinical findings into effective human treatments, given the complex molecular cascade initiated by ischemia.
- Hemorrhagic Stroke Management: Research in hemorrhagic stroke, particularly intracerebral hemorrhage (ICH), focuses on minimizing hematoma expansion and managing secondary brain injury. Strategies include aggressive blood pressure control, reversal of anticoagulation, and surgical evacuation where appropriate. Novel hemostatic agents and minimal invasive surgical techniques are under investigation.
Stroke Rehabilitation
Rehabilitation is a crucial component of stroke recovery, driving functional gains and improving quality of life.
- Neuroplasticity and Recovery: Understanding the mechanisms of post-stroke neuroplasticity is central to optimizing rehabilitation. Research is investigating how the brain reorganizes itself after injury, forming new connections and strengthening existing ones. This includes studies on cortical reorganization, axonal sprouting, and synaptogenesis.
- Technology-Assisted Rehabilitation: The integration of technology into rehabilitation is expanding. Robotics, virtual reality (VR), and brain-computer interfaces (BCIs) offer structured, repetitive, and engaging training paradigms. Robotics can facilitate motor recovery, VR provides immersive environments for functional training, and BCIs hold promise for individuals with severe motor deficits by allowing them to control external devices or even stimulate their own muscles using brain signals.
- Pharmacological Adjuncts to Rehabilitation: Research is exploring whether pharmacological agents can enhance the effects of rehabilitation. Medications that modulate neurotransmitter systems, such as selective serotonin reuptake inhibitors (SSRIs) or noradrenergic agents, are being investigated for their potential to promote motor recovery or improve mood and cognition in stroke survivors.
- Personalized Rehabilitation: The concept of personalized rehabilitation, tailoring interventions based on individual patient characteristics, lesion location, and recovery potential, is gaining traction. This involves using imaging biomarkers and physiological measures to predict recovery trajectories and optimize intervention strategies.
Multiple Sclerosis (MS) and Demyelinating Disorders
Multiple Sclerosis is an autoimmune disease affecting the central nervous system, characterized by demyelination, inflammation, and neurodegeneration. Research in this field is rapidly evolving, leading to a broader array of treatment options.
Disease-Modifying Therapies (DMTs)
The landscape of MS treatment has been significantly transformed by the development of numerous DMTs, aiming to reduce relapse rates and slow disease progression.
- Immunomodulation and Immunosuppression: DMTs operate through various mechanisms, including broad immunosuppression (e.g., fingolimod, cladribine), selective immunomodulation targeting specific immune cell populations (e.g., alemtuzumab targeting CD52, ocrelizumab targeting CD20 B cells), and interferon-beta and glatiramer acetate, which modulate the immune response. These treatments act as gatekeepers, reducing the flow of harmful immune cells into the CNS.
- Oral and Infusion Therapies: The introduction of oral DMTs has improved convenience and adherence for many patients. Con currently, highly effective, periodically administered infusion therapies offer potent immunomodulation. Research continues to compare the efficacy and safety profiles of these different therapeutic classes to guide personalized treatment decisions.
- Predictive Biomarkers for Response: Identifying biomarkers that predict an individual’s response to a specific DMT is an active area of research. This could allow for more targeted and effective initial treatment selection, minimizing trial-and-error approaches. For instance, genetic polymorphisms or specific immune cell signatures are being investigated as potential predictors.
Progressive MS Research
Addressing progressive forms of MS, particularly primary progressive MS (PPMS) and secondary progressive MS (SPMS), remains a significant unmet need.
- Neurodegeneration Focus: Research increasingly recognizes that progressive MS involves substantial neurodegeneration in addition to inflammation. Studies are exploring therapies that directly protect neurons and oligodendrocytes, or promote remyelination, independent of immune suppression. This represents a shift from purely anti-inflammatory strategies.
- Remyelination Strategies: Promoting remyelination, the process of repairing damaged myelin sheaths, is a major goal. Investigations include agents that stimulate oligodendrocyte precursor cell differentiation and maturation, such as antagonists of specific receptors or growth factors. The hope is to restore nerve conduction and prevent further axonal damage.
- Targeting Chronic Inflammation: Even in progressive MS, a smoldering, chronic inflammatory process persists within the CNS, often compartmentalized. Research is exploring therapies that can penetrate the blood-brain barrier to target these localized inflammatory sites more effectively, and reduce the sustained low-level assault on neural tissue.
Epilepsy and Seizure Disorders
Epilepsy, a chronic neurological disorder characterized by recurrent unprovoked seizures, presents diverse challenges due to its varied etiologies and manifestations.
Antiseizure Medications (ASMs)
The development of new ASMs continues to broaden therapeutic options for patients, aiming for seizure freedom with minimal side effects.
- Novel Mechanisms of Action: Newer ASMs often target different molecular pathways compared to older generations. This includes modulators of sodium or calcium channels, enhancers of GABAergic transmission, regulators of synaptic vesicle release (e.g., levetiracetam, brivaracetam), and agents with broad-spectrum effects. This expansion of mechanisms provides more options for patients who do not respond to initial treatments, akin to finding the right key for a complex lock.
- Personalized Medicine Approaches: Genetic testing is increasingly used to identify specific etiologies of epilepsy, particularly in childhood epilepsies, and to guide ASM selection. For instance, certain genetic mutations predict response or adverse reactions to specific drugs. This move towards precision medicine helps to optimize treatment strategies from the outset.
- Drug-Resistant Epilepsy: A significant proportion of patients experience drug-resistant epilepsy. Research focuses on understanding the underlying mechanisms of drug resistance (e.g., drug efflux pumps, altered receptor sensitivity) and developing novel ASMs specifically for this population. There is also increased interest in non-pharmacological interventions for these individuals.
Advanced Therapeutic Options
For patients whose seizures are not controlled by ASMs, several advanced therapies are available or under investigation.
- Epilepsy Surgery: For focal epilepsy, surgical resection of the epileptogenic zone remains a highly effective treatment option. Advances in presurgical evaluation, including advanced neuroimaging (fMRI, MEG, PET), intracranial EEG monitoring, and brain mapping, help to precisely localize seizure onset zones while minimizing damage to critical brain functions.
- Neurostimulation Devices: Vagus Nerve Stimulation (VNS), Responsive Neurostimulation (RNS), and Deep Brain Stimulation (DBS) offer alternative treatment modalities. RNS, in particular, provides closed-loop stimulation, detecting and responding to epileptiform activity. Research is refining the targeting, programming, and long-term efficacy of these devices.
- Ketogenic Diet and Other Dietary Therapies: The ketogenic diet, a high-fat, low-carbohydrate diet, has proven efficacy in certain types of epilepsy, especially in children. Research explores the metabolic mechanisms by which it exerts its antiseizure effects, including altered neurotransmitter levels and mitochondrial function. Other dietary interventions are also being investigated.
- Gene Therapies: Gene therapy approaches are in preclinical and early clinical stages, aiming to correct genetic defects causing epilepsy or deliver genes that can suppress seizure activity. This holds promise for specific genetic epilepsies, offering the potential for a disease-modifying treatment rather than symptomatic control.
Neurological Manifestations of Systemic Diseases and Emerging Threats
| Study Name | Institution | Focus Area | Participants | Duration | Status |
|---|---|---|---|---|---|
| Cardiovascular Health Study | City Medical Center | Heart Disease Prevention | 150 | 12 months | Ongoing |
| Diabetes Management Trial | Regional Health Institute | Type 2 Diabetes | 200 | 18 months | Recruiting |
| Respiratory Therapy Evaluation | University Hospital | Asthma Treatment | 100 | 6 months | Completed |
| Nutrition and Obesity Study | Health Research Center | Obesity Prevention | 120 | 9 months | Ongoing |
| Mental Health Awareness Program | Community Clinic | Depression and Anxiety | 80 | 4 months | Recruiting |
The brain is not an isolated organ, and systemic conditions frequently impact neurological health. Furthermore, novel pathogens and environmental factors pose evolving threats.
Neuroinflammation and Autoimmunity
Understanding the complex interactions between systemic inflammation, the immune system, and the central nervous system is a growing area of focus.
- Autoimmune Encephalitis: The recognition of various autoimmune encephalitides, often characterized by antibodies against neuronal surface antigens (e.g., anti-NMDAR encephalitis), has revolutionized the diagnosis and treatment of previously unexplained neuropsychiatric syndromes. Research continues to identify new autoantibodies and mechanisms of autoimmune brain injury.
- Systemic Inflammatory Conditions and the Brain: Chronic systemic inflammatory conditions, such as rheumatoid arthritis or inflammatory bowel disease, are increasingly linked to neurological complications, including cognitive impairment, stroke risk, and mood disorders. Studies are unraveling the pathways by which peripheral inflammation can affect brain function and integrity, often involving blood-brain barrier disruption and microglial activation.
- Microglia and Astrocytes in Disease: Beyond their traditional support roles, microglia and astrocytes are recognized as active participants in neuroinflammation and neurodegeneration. Research is delineating their diverse phenotypes and functions in health and disease, identifying them as potential therapeutic targets for a range of neurological disorders.
Neurological Impact of Emerging Pathogens
Recent global health crises highlight the brain’s vulnerability to viral infections and other pathogens.
- COVID-19 and Neurological Sequelae: The COVID-19 pandemic revealed a spectrum of neurological manifestations, ranging from acute encephalopathy and stroke to long-term cognitive impairment and fatigue (often termed “long COVID”). Research is actively investigating the mechanisms of viral entry into the brain, inflammatory responses, and potential for neurodegeneration induced by SARS-CoV-2. This includes studies on direct viral invasion, immune-mediated damage, and microvascular injury.
- Zika Virus and Congenital Brain Malformations: The Zika virus outbreak underscored the devastating impact of neurotropic viruses, particularly on fetal brain development, leading to microcephaly and other severe neurological defects. Research focused on understanding viral neurotropism and developing effective prevention and intervention strategies.
- Other Neurotropic Infections: Ongoing surveillance and research into other neurotropic viruses and pathogens (e.g., West Nile virus, Japanese encephalitis virus, tick-borne encephalitis virus) remain critical for public health. Understanding their pathogenesis and developing effective vaccines or antiviral treatments is a continuous effort.
Environmental Factors and Neurological Health
The burgeoning field of environmental neuroscience investigates how external factors influence brain health and disease risk.
- Air Pollution and Neurological Disorders: Exposure to air pollutants, particularly fine particulate matter, is increasingly linked to an elevated risk of stroke, dementia, and neurodevelopmental disorders. Research is exploring how airborne toxins enter the brain (e.g., via the olfactory bulb), induce neuroinflammation, and contribute to protein misfolding or vascular damage.
- Pesticides and Neurotoxicity: Certain pesticides are known neurotoxins, and chronic exposure is associated with an increased risk of Parkinson’s disease and other neurological conditions. Studies are investigating the molecular mechanisms of pesticide-induced neurotoxicity, often involving mitochondrial dysfunction and oxidative stress.
- Heavy Metals and Neurodevelopment: Exposure to heavy metals such as lead and mercury, even at low levels, can have profound and lasting effects on neurodevelopment in children, leading to cognitive deficits and behavioral problems. Research focuses on understanding critical exposure periods and developing mitigation strategies.
This overview provides a glimpse into the dynamic and complex field of neurology. As our understanding of the brain deepens, we anticipate continued progress in diagnostics, therapeutics, and ultimately, improved outcomes for individuals affected by neurological conditions.