Clinical trial site selection is a critical early step in the drug development process. Inadequate site selection can lead to significant delays, increased costs, and compromised data quality. This article outlines strategies for optimizing clinical trial site selection, emphasizing a data-driven and structured approach.
Effective site selection is not merely about identifying facilities capable of conducting a trial. It involves a strategic evaluation of numerous factors convergent at a site, ensuring alignment with the trial’s specific requirements. Think of site selection as laying the foundation of a building; a weak foundation will inevitably lead to structural problems, but a robust one supports successful construction.
Defining Trial-Specific Needs
Before external engagement begins, the core needs of the clinical trial must be thoroughly articulated. This involves detailing the protocol’s demands and anticipated population characteristics.
Protocol Complexity and Resource Requirements
The complexity of the clinical trial protocol directly influences the type of site required. Protocols with numerous assessments, specialized procedures, or extended visit schedules demand sites with robust infrastructure, experienced staff, and ample resources. For instance, a trial requiring frequent PET scans necessitates sites with readily available imaging equipment and expert technicians.
Target Patient Population Characteristics
Understanding the target patient population is paramount. Factors such as disease prevalence, demographic characteristics, comorbidities, and socio-economic status influence a site’s ability to recruit and retain participants. A rare disease trial, for example, will require sites with established patient registries or strong referral networks for that specific condition. Geographic distribution of the target population also plays a role in site selection to ensure accessibility and representation.
Data-Driven Site Identification
Modern site selection leverages data analytics and historical performance metrics to move beyond anecdotal evidence or prior relationships. This shift from gut feeling to evidence-based decision-making minimizes risk.
Utilizing Historical Performance Data
Historical data provides invaluable insights into a site’s capabilities and past performance. This includes metrics related to patient recruitment, retention, data quality, and regulatory compliance.
Recruitment Metrics
Analyzing a site’s historical recruitment rates for similar trials offers a predictive indicator of future performance. This includes the number of patients screened, enrolled, and randomized, as well as screen-fail rates. A site consistently failing to meet recruitment targets in previous trials poses a risk to the current trial’s timelines.
Retention and Compliance Rates
High patient retention is crucial for data integrity. Sites with a history of low patient dropout rates and high protocol adherence among participants are more desirable. Conversely, sites with frequent protocol deviations or high withdrawal rates warrant closer scrutiny.
Data Quality and Timeliness
The promptness and accuracy of data submission are critical. Sites with a track record of timely and clean data entry reduce monitoring burden and accelerate database lock. Consider metrics like query resolution time and the frequency of data entry errors.
Leveraging Real-World Data (RWD)
Real-world data, including electronic health records (EHRs), claims data, and public health registries, can provide current insights into patient populations and disease prevalence.
Enhancing Patient Landscape Understanding
RWD offers a current snapshot of patient populations, including disease prevalence within specific geographic areas. This can inform the feasibility of recruiting a sufficient number of eligible participants at a given site. For example, analyzing EHR data in a particular hospital system might reveal a larger-than-anticipated patient pool for a specific oncological indication.
Identifying Investigator Expertise
EHRs can also highlight investigators with substantial experience treating the target patient population or those who frequently refer patients to clinical trials. This helps in identifying potential investigators who may not be immediately apparent through traditional channels.
Site Qualification and Evaluation

Once potential sites are identified, a systematic qualification and evaluation process is necessary. This moves beyond initial data points to a deeper assessment of operational capabilities and environmental factors. This stage is analogous to a meticulous inspection before purchasing a complex piece of machinery; you want to ensure all components function as expected.
Operational Capabilities Assessment
A comprehensive assessment of a site’s operational capabilities ensures it can execute the trial protocol efficiently and compliantly.
Staffing Experience and Availability
Adequate staffing, including qualified investigators, research coordinators, nurses, and administrative support, is essential. The experience level of the research team with similar trial phases and therapeutic areas directly impacts trial success. High staff turnover is a red flag, as it can indicate an unstable research environment or excessive workload.
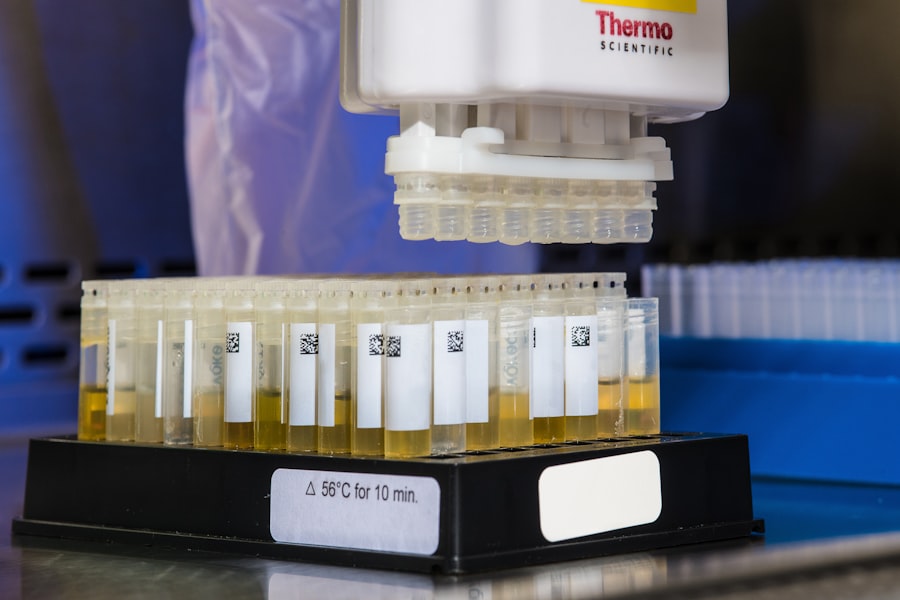
Infrastructure and Equipment
Sites must possess the necessary infrastructure and equipment to support all protocol-mandated procedures. This includes calibrated laboratory equipment, secure drug storage facilities, appropriate patient examination rooms, and IT systems capable of handling electronic data capture (EDC). For complex trials, access to specialized diagnostic or therapeutic facilities is critical.
Regulatory and Ethical Compliance
A site’s history of adherence to Good Clinical Practice (GCP) and local regulatory requirements is non-negotiable. This includes past audit findings, institutional review board (IRB)/ethics committee approval processes, and documentation practices. Sites with a history of significant regulatory infractions pose substantial risk to data integrity and participant safety.
Investigator Engagement and Commitment
Beyond technical capabilities, the investigator’s enthusiasm, commitment, and alignment with the study’s scientific objectives are crucial. The investigator is the conductor of the orchestra that is the clinical trial; an uncommitted conductor will result in a discordant performance.
Demonstrated Interest and Therapeutic Area Expertise
The principal investigator’s (PI) genuine interest in the specific trial and their deep scientific and clinical expertise in the therapeutic area are strong indicators of potential success. During pre-study visits, assess their understanding of the protocol and their ability to articulate scientific rationale.
Access to Target Patient Population
Evaluate the investigator’s established patient base and their referral networks. A PI can have impressive credentials, but if their patient base does not align with the trial’s inclusion/exclusion criteria, recruitment will suffer. Direct questions about how they plan to identify and recruit eligible patients are necessary.
Risk Mitigation and Contingency Planning
Optimizing site selection also involves proactively identifying potential risks and developing contingency plans. No site is perfect, and anticipating challenges can prevent significant setbacks.
Identifying Potential Recruitment Bottlenecks
Even with thorough planning, recruitment challenges can emerge. Proactive identification of potential bottlenecks allows for the development of strategies to mitigate them.
Competing Trials and Patient Overlap
Investigate if the site is participating in multiple competing trials that target the same patient population. This poses a risk of patient overlap and can dilute recruitment efforts for the current trial. Understanding the site’s entire research portfolio is important.
Geographic and Socioeconomic Barriers
Consider geographic barriers that might limit patient access to the site (e.g., long travel distances, lack of public transportation). Socioeconomic factors, such as insurance coverage or out-of-pocket expenses for participants, can also influence recruitment and retention.
Developing Contingency Strategies
Robust site selection includes preparing for potential underperformance or unforeseen circumstances.
Backup Sites and Investigator Networks
Identify a pool of backup sites or investigators that can be activated if primary sites underperform. Establishing relationships with these potential alternatives early can expedite their activation.
Enhanced Support and Training
For sites with strong potential but some areas for improvement, consider offering enhanced training, additional resources, or dedicated monitoring support. This can involve providing extra personnel for specific tasks or more frequent monitoring visits.
Continuous Monitoring and Adaptation
| Metric | Description | Importance | Typical Value/Range | Impact on Site Selection |
|---|---|---|---|---|
| Patient Recruitment Rate | Number of patients enrolled per month at the site | High | 5-20 patients/month | Sites with higher recruitment rates are preferred to meet enrollment timelines |
| Site Activation Time | Time from site selection to site readiness for enrollment | Medium | 4-12 weeks | Shorter activation times accelerate trial start-up |
| Regulatory Approval Time | Duration for obtaining local regulatory and ethics approvals | High | 6-16 weeks | Sites with faster approvals reduce delays |
| Investigator Experience | Number of previous clinical trials conducted by the investigator | High | 0-50+ trials | Experienced investigators improve data quality and compliance |
| Site Infrastructure | Availability of necessary equipment and facilities | High | Qualitative assessment | Sites with adequate infrastructure ensure protocol adherence |
| Data Quality Metrics | Rate of data queries and protocol deviations | High | Query rate <5%, deviations <2% | Lower rates indicate higher data reliability |
| Patient Population Access | Availability of target patient demographics at the site | High | Varies by indication | Sites with access to target populations improve recruitment feasibility |
| Site Staff Turnover | Frequency of key staff changes during trial | Medium | Low turnover preferred | Stable staff supports consistent trial conduct |
| Previous Trial Performance | Historical adherence to timelines and quality standards | High | Qualitative and quantitative data | Good past performance predicts successful trial execution |
Site selection is not a one-time event; it is an ongoing process throughout the trial lifecycle. Continuous monitoring and a willingness to adapt are essential for sustained success.
Performance Tracking and Metrics
Regularly track key performance indicators (KPIs) for each site. This allows for early detection of underperformance and timely intervention.
Recruitment and Enrollment Progress
Monitor screening rates, screen failure rates, and actual enrollment against projected targets. Deviations from the plan necessitate investigation and potentially corrective actions.
Data Quality and Compliance
Evaluate the quality and timeliness of data submission, query resolution rates, and the incidence of protocol deviations. Consistent data quality issues may indicate a need for further training or increased monitoring.
Adaptive Management Strategies
Be prepared to adapt the site selection strategy based on ongoing performance. Rigidity in the face of underperformance can be detrimental.
Investigator Engagement and Motivation
If sites are struggling, re-engage with investigators to understand challenges and provide necessary support. Sometimes, renewed motivation or additional resources can turn a site around.
Deactivation and New Site Activation
In extreme cases of persistent underperformance or unforeseen circumstances, the deactivation of a site may be necessary. Simultaneously, activating new, higher-performing sites or expanding existing ones can help compensate for lost ground. This requires a well-defined process for site close-out and rapid ramp-up of new clinical locations.
By adhering to a structured, data-driven, and adaptive approach to clinical trial site selection, sponsors and contract research organizations can significantly increase the likelihood of achieving recruitment targets, maintaining data quality, and ultimately accelerating drug development. The process demands meticulous planning, proactive risk assessment, and continuous vigilance, ensuring that the trial’s foundation remains strong throughout its duration.



