Clinical trials are a cornerstone of medical advancement, serving as the rigorous process through which new treatments, drugs, and medical devices are evaluated for safety and efficacy. The complexity of these trials—ranging from Phase I assessments of safety to large-scale Phase III studies confirming effectiveness—necessitates meticulous management of vast quantities of data. Historically, data collection and management in clinical trials relied heavily on paper-based methods, a system prone to errors, delays, and inefficiencies. The advent of data management systems (DMS) has fundamentally transformed this landscape, offering a structured and systematic approach to handling clinical trial data.
A Clinical Data Management System (CDMS) is a software solution designed to centralize, standardize, and streamline the entire data lifecycle within a clinical trial. This includes data collection, entry, validation, cleaning, and reporting. The primary objective of a CDMS is to ensure the integrity, accuracy, and completeness of clinical trial data, which are paramount for regulatory submissions and scientific credibility. Without robust data management, the conclusions drawn from a trial might be flawed, potentially leading to incorrect treatment decisions or the failure to bring genuinely effective therapies to patients. Think of a CDMS not as an optional add-on, but as the central nervous system of a clinical trial, coordinating and processing all vital information.
The Evolution of Clinical Data Management
The trajectory of clinical data management mirrors the broader evolution of information technology. Early clinical trials managed data manually, a labor-intensive process that involved physical case report forms (CRFs), transcription, and manual checking.
Paper-Based Systems and Their Limitations
In the era of paper-based systems, CRFs were filled out by investigators at study sites. These forms were then either mailed or faxed to a central data management team. This process was inherently slow and introduced numerous points of potential error.
- Data Transcription Errors: Manual entry of data from paper CRFs into electronic databases often led to transcription mistakes.
- Logistical Challenges: Shipping and handling of paper CRFs posed significant logistical hurdles, including potential loss or damage.
- Delayed Data Availability: The time lag between data collection at the site and its availability for analysis was substantial, hindering timely decision-making and progress monitoring.
- Difficulty in Query Resolution: Identifying and resolving discrepancies or missing data often required extensive communication back and forth between sites and data management teams, further delaying the process.
- Limited Data Validation: Manual validation checks were resource-intensive and often incomplete, leading to lower data quality.
Emergence of Electronic Data Capture (EDC)
The late 1990s and early 2000s saw the widespread adoption of Electronic Data Capture (EDC) systems. EDC systems revolutionized data collection by allowing investigators to directly enter patient data into an electronic database via a web-based interface.
- Improved Data Quality: EDC systems incorporate built-in validation checks (e.g., range checks, dependency checks) at the point of data entry, significantly reducing errors.
- Real-time Data Access: Data entered into an EDC system is immediately available to the central data management team, enabling quicker analysis and oversight.
- Faster Query Resolution: Queries for discrepancies can be generated and sent electronically to sites, facilitating rapid resolution.
- Reduced Operational Costs: While initial setup can be significant, EDC systems often reduce costs associated with printing, shipping, and manual data entry/cleaning over the course of a trial.
- Enhanced Audit Trails: EDC systems automatically record all data modifications, providing a comprehensive audit trail crucial for regulatory compliance.
Modern Integrated Data Management Systems
Today, CDMS encompasses a broader suite of functionalities beyond just EDC. Modern systems integrate various components, creating a holistic platform for clinical trial management. These include modules for randomization, supply management, safety data management, and even aspects of clinical trial management systems (CTMS). The trend is towards comprehensive, integrated platforms that serve as a single source of truth for all trial-related data. Think of a modern CDMS as a unified control tower, overseeing all aspects of data operations in a trial.
Key Features and Components of an Optimal CDMS
An effective CDMS is more than just a data entry tool; it’s a comprehensive ecosystem designed to support the entire lifecycle of clinical trial data with accuracy, security, and efficiency.
Electronic Case Report Forms (eCRFs)
eCRFs are the digital equivalent of paper CRFs. They are designed to collect specific data points from study participants according to the trial protocol.
- Intuitive User Interface: eCRFs should be user-friendly and logically structured to minimize data entry errors and reduce investigator burden.
- Built-in Edit Checks and Validation Rules: These are critical for ensuring data quality at the point of entry. Examples include range checks (e.g., blood pressure values within a physiological range), format checks (e.g., date formats), and consistency checks (e.g., age consistent with date of birth).
- Branching Logic and Skip Patterns: These features streamline data entry by presenting only relevant questions based on previous answers, reducing unnecessary data collection and potential for errors.
- Data Dictionary Integration: Standardized terminology and definitions across all eCRFs ensure consistency and prevent ambiguity.
Data Validation and Cleaning Tools
Robust validation and cleaning processes are essential for transforming raw data into high-quality, analyzable information.
- Automated Query Generation: The CDMS should automatically flag data discrepancies or missing information based on predefined rules and generate queries for site resolution.
- Query Management System: A robust system to create, track, and resolve data queries efficiently, including audit trails of all query activities.
- Data Review Tools: Features that allow data managers to visually inspect data, identify outliers, and perform manual data review.
- Discrepancy Reporting: Comprehensive reports detailing all data discrepancies, their status, and resolution history.
Security and Compliance Features
Given the sensitive nature of patient data and stringent regulatory requirements, security and compliance are non-negotiable.
- Role-Based Access Control (RBAC): Ensures that users only have access to information and functionalities relevant to their role in the trial.
- Audit Trails: A forensic record of every action performed within the system, including who did what, when, and from where. This is crucial for verifying data integrity and regulatory accountability.
- Data Encryption: Protection of data both in transit and at rest, safeguarding against unauthorized access.
- Regulatory Compliance Support: Adherence to regulations such as FDA 21 CFR Part 11 (electronic records and electronic signatures), GDPR (General Data Protection Regulation), and HIPAA (Health Insurance Portability and Accountability Act). The system should facilitate compliance, providing tools for electronic signatures and documented procedures.
Reporting and Analytics Capabilities
The ability to extract meaningful insights from trial data is fundamental to progress monitoring, safety review, and final analysis.
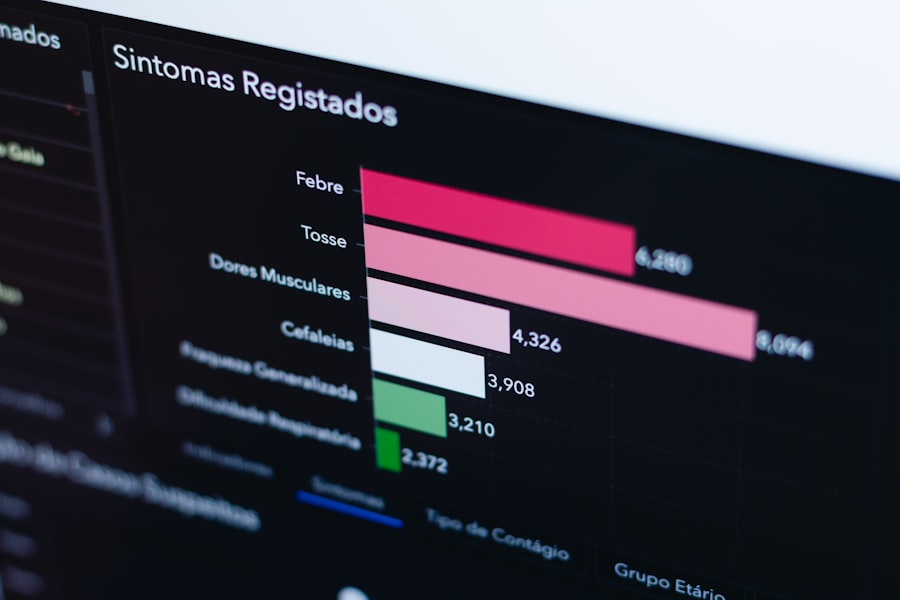
- Real-time Dashboards: Visual representations of key study metrics (e.g., enrollment status, query rates, data completeness) for quick oversight.
- Customizable Reports: The ability to generate ad-hoc and pre-defined reports on various aspects of the trial data.
- Data Export Functionality: Secure and standardized export of data in formats compatible with statistical analysis software (e.g., SAS, R, SPSS).
- Trend Analysis: Tools to identify patterns and trends in data, such as changes in adverse event reporting or medication adherence over time.
Benefits of Optimizing Clinical Trials with CDMS

Adopting and effectively utilizing a CDMS translates into tangible benefits that impact every phase and aspect of a clinical trial. It is not merely an expense, but an investment that yields significant returns in efficiency, quality, and regulatory success.
Enhanced Data Quality and Integrity
This is perhaps the most critical benefit. High-quality data is the bedrock upon which valid scientific conclusions are built.
- Reduced Human Error: Automation of data entry checks and validation significantly minimizes errors inherent in manual processes.
- Increased Accuracy: Real-time validation and query resolution ensure data is accurate closer to the point of origin, preventing error propagation.
- Improved Consistency: Standardized eCRFs and data dictionaries enforce consistency across sites and participants.
Accelerated Timelines and Reduced Costs
Efficiency gains from a CDMS directly translate into faster trial completion and lower operational expenses.
- Faster Data Lock: Automated data cleaning and query management dramatically reduce the time required to achieve database lock, a critical milestone before statistical analysis.
- Quicker Regulatory Submissions: A clean, well-documented database streamlines the process of preparing data for regulatory authorities, accelerating review and approval timelines.
- Lower Monitoring Costs: Centralized data access allows for more efficient remote monitoring, reducing the need for costly on-site visits.
- Optimized Resource Allocation: Data managers and clinical research associates (CRAs) can focus on complex issues rather than mundane manual checks.
Improved Oversight and Decision-Making
A CDMS provides a panoramic view of trial progress, empowering stakeholders with timely and accurate information.
- Real-time Progress Monitoring: Stakeholders can track enrollment, data entry status, and key performance indicators in real time.
- Proactive Risk Management: Early identification of data trends or issues allows for prompt intervention and mitigation strategies.
- Informed Safety Monitoring: Rapid access to adverse event data supports timely safety reviews and reporting.
- Adaptive Trial Design: The availability of real-time data can support adaptive trial designs, allowing for modifications based on accumulating evidence.
Enhanced Regulatory Compliance
Navigating the complex landscape of regulatory requirements is a primary concern for clinical trial sponsors. A CDMS acts as a powerful ally in this endeavor.
- Robust Audit Trails: Detailed immutable records of all data changes and user actions provide irrefutable evidence for regulatory inspections.
- Electronic Signatures: Compliance with 21 CFR Part 11 for electronic signatures reduces reliance on paper and streamlines approval processes.
- Standardization: Adherence to industry standards (e.g., CDISC) facilitated by CDMS platforms simplifies data exchange and regulatory submissions.
- Data Traceability: The ability to trace every data point back to its source ensures accountability and transparency.
Challenges and Considerations in CDMS Implementation
| Metric | Description | Typical Value / Range | Importance |
|---|---|---|---|
| Data Entry Accuracy | Percentage of data entered without errors | 95% – 99.9% | High |
| Data Query Resolution Time | Average time to resolve data queries (days) | 1 – 5 days | High |
| System Uptime | Percentage of time the system is operational | 99.5% – 99.99% | Critical |
| Data Backup Frequency | How often data backups are performed | Daily to Weekly | High |
| Audit Trail Completeness | Extent to which all data changes are logged | 100% | Critical |
| Compliance with Regulatory Standards | Adherence to standards like 21 CFR Part 11, GDPR | Full Compliance | Critical |
| Data Export Formats Supported | Number of standard formats (e.g., CDISC, SAS) | 3 – 5 formats | Medium |
| User Access Control Granularity | Level of detail in user permissions | Role-based, fine-grained | High |
| Integration Capability | Ability to integrate with other systems (e.g., EDC, CTMS) | API, HL7, CDISC ODM support | High |
| Data Storage Capacity | Maximum volume of data supported | Terabytes to Petabytes | Medium |
While the advantages of CDMS are clear, successful implementation is not without its challenges. Organizations must anticipate and address these issues proactively.
Vendor Selection and Customization
Choosing the right CDMS vendor is a critical initial step, akin to selecting the right architect for a complex building project.
- Functional Adequacy: The chosen system must possess the features and capabilities required to support the specific trial’s protocol and data types.
- Scalability: The system should be able to scale to accommodate trials of different sizes and complexities, from small pilot studies to large multinational trials.
- Integration Capabilities: Its ability to integrate with other systems (e.g., CTMS, safety databases, lab systems) is paramount for creating a seamless data flow.
- Vendor Support and Training: Reliable customer support, comprehensive training programs, and ongoing maintenance are crucial for long-term success.
- Customization vs. Configuration: While some level of customization may be necessary, over-customization can lead to maintenance headaches and compatibility issues. Opt for configurable systems where possible.
Data Migration and Integration
For organizations transitioning from legacy systems or paper-based methods, data migration can be a complex undertaking.
- Data Standardization: Ensuring consistent data formats and definitions across disparate sources before migration is essential.
- Data Mapping: Precisely mapping fields from source systems to the CDMS to prevent data loss or misinterpretation.
- Validation of Migrated Data: Thoroughly validating migrated data to ensure accuracy and completeness after transfer.
- Integration with Third-Party Systems: Establishing secure and efficient interfaces with external systems to facilitate data exchange.
User Adoption and Training
Even the most sophisticated CDMS will fail if its users are unwilling or unable to adopt it effectively.
- Change Management: Implementing a robust change management strategy to address user concerns and mitigate resistance to change.
- Comprehensive Training Programs: Tailored training for different user roles (investigators, CRAs, data managers) covering system functionalities, best practices, and troubleshooting.
- Ongoing Support: Providing accessible help desks and support resources to address user queries and issues promptly.
- User-Friendly Design: Prioritizing systems with intuitive interfaces and logical workflows to minimize the learning curve.
Regulatory Landscape and Compliance Updates
The regulatory environment for clinical trials is dynamic, requiring continuous adaptation.
- Staying Current with Regulations: Ensuring the CDMS and its processes remain compliant with evolving regulations (e.g., new versions of GDPR, updated FDA guidance).
- System Validation: Periodically validating the CDMS to demonstrate its fitness for purpose and compliance (e.g., GAMP 5 guidelines).
- Documentation: Maintaining comprehensive documentation of system processes, validation activities, and compliance measures.
The Future of Clinical Data Management
The landscape of clinical data management is continuously evolving, driven by technological advancements and the increasing complexity of clinical research.
Artificial Intelligence and Machine Learning in CDMS
AI and ML are poised to revolutionize several aspects of clinical data management.
- Predictive Analytics for Data Quality: AI algorithms can predict potential data quality issues, allowing for proactive intervention.
- Automated Query Resolution: Machine learning can identify patterns in data discrepancies and suggest or even automate the resolution of routine queries.
- Intelligent Data Monitoring: AI can sift through vast datasets to identify subtle trends or anomalies that might indicate safety signals or protocol deviations.
- Improved eCRF Design: AI can analyze data entry patterns to optimize eCRF design for user efficiency and data quality.
Integration with Wearables and Real-World Data (RWD)
The proliferation of wearable devices and the growing importance of RWD sources are expanding the scope of clinical data.
- Direct Data Capture from Wearables: CDMS systems will increasingly integrate with wearable devices to collect continuous physiological data directly from participants, reducing recall bias and providing richer datasets.
- Incorporation of RWD: Integrating data from electronic health records (EHRs), claims databases, and patient registries into CDMS platforms for a more complete understanding of patient outcomes and treatment effectiveness in real-world settings.
- Hybrid Trials: Facilitating hybrid trial designs that blend traditional site-based data collection with remote monitoring and RWD.
Blockchain for Data Integrity and Security
Blockchain technology holds potential for enhancing the security and integrity of clinical trial data.
- Immutable Audit Trails: Blockchain’s distributed ledger technology can create an unchangeable and verifiable record of all data transactions, further bolstering data integrity and regulatory compliance.
- Enhanced Data Sharing: Secure and transparent sharing of data among authorized parties while maintaining patient privacy.
- Decentralized Trials: Supporting decentralized clinical trials (DCTs) by providing a secure and transparent framework for data collection and management from multiple remote sources.
Cloud-Based CDMS Solutions
Cloud computing has become the standard for modern CDMS solutions, offering flexibility and scalability.
- Accessibility and Collaboration: Cloud-based platforms allow global access and seamless collaboration among geographically dispersed teams.
- Reduced Infrastructure Costs: Eliminates the need for on-premise servers and associated maintenance costs.
- Scalability on Demand: Easily scale computing resources up or down based on trial needs, optimizing resource utilization.
- Enhanced Security Protocols: Cloud providers typically invest heavily in robust security infrastructure and compliance certifications.
In conclusion, the optimization of clinical trials through advanced data management systems is not merely a technological upgrade but a strategic imperative. As clinical research continues to evolve in complexity and scope, a robust, intelligent, and integrated CDMS will remain at the core of ensuring the integrity, efficiency, and regulatory compliance essential for bringing safe and effective therapies to patients worldwide.



