Clinical trials are systematic investigations designed to evaluate the safety and efficacy of new medical interventions, including drugs, devices, and treatment protocols. These trials are essential components of the medical research landscape, serving as the bridge between laboratory discoveries and clinical application. They are typically conducted in phases, each with distinct objectives and methodologies.
Phase I trials primarily focus on assessing safety and determining appropriate dosage levels, often involving a small group of healthy volunteers. Phase II trials expand the participant pool to evaluate the treatment’s effectiveness and further assess safety in a larger cohort. Phase III trials are pivotal, as they compare the new intervention against standard treatments in a randomized manner, often involving thousands of participants across multiple sites.
The design of clinical trials is governed by rigorous protocols that ensure scientific validity and ethical standards. Regulatory bodies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), oversee these trials to protect participants and ensure that the findings are credible.
The process is not only about testing new therapies but also about gathering comprehensive data that can inform future medical practices. This data can lead to significant advancements in healthcare, providing insights into disease mechanisms, treatment responses, and patient outcomes. The complexity of clinical trials reflects the multifaceted nature of human health and disease, necessitating a collaborative approach among researchers, healthcare professionals, and participants.
Key Takeaways
- Clinical trials are essential for developing new medical treatments and improving healthcare.
- Participant involvement is crucial for the success and validity of clinical research.
- Joining a trial offers potential health benefits but also involves certain risks.
- Finding suitable clinical trials requires understanding eligibility criteria and available resources.
- Participation in trials contributes significantly to medical advancements and future therapies.
The Importance of Participant Involvement
Participant involvement in clinical trials is crucial for several reasons. First and foremost, individuals who volunteer for these studies contribute to the advancement of medical knowledge. Their participation helps researchers understand how new treatments work in real-world scenarios, which is essential for developing effective therapies.
Without participants, clinical trials cannot be conducted, and the progression of medical science would be severely hindered. Each participant’s experience provides invaluable data that can lead to breakthroughs in treatment options for various diseases, from cancer to rare genetic disorders. Moreover, participant involvement fosters a sense of community and shared purpose among those affected by specific health conditions.
Many individuals who join clinical trials do so out of a desire to help others facing similar challenges. This altruistic motivation can be particularly strong in populations with limited treatment options or those suffering from chronic illnesses. By participating in clinical trials, individuals not only contribute to scientific research but also gain access to cutting-edge therapies that may not yet be available through standard care.
This dual benefit underscores the importance of participant involvement in shaping the future of healthcare.
Benefits and Risks of Participating

Participating in clinical trials offers numerous benefits, but it is essential to weigh these against potential risks. One of the primary advantages is access to innovative treatments that may be more effective than existing options. Participants often receive close monitoring and care from healthcare professionals throughout the trial, which can lead to improved health outcomes.
Additionally, many clinical trials provide participants with comprehensive health assessments and follow-up care, which can enhance their overall well-being. However, there are inherent risks associated with clinical trial participation. New treatments may have unknown side effects or may not work as intended.
Participants may experience adverse reactions that were not evident during earlier phases of testing. Furthermore, the experimental nature of clinical trials means that there is no guarantee of benefit; some participants may receive a placebo instead of an active treatment. It is crucial for potential participants to have open discussions with their healthcare providers about these risks and benefits before making a decision.
Informed consent is a fundamental aspect of clinical trials, ensuring that participants understand what they are agreeing to and can make choices aligned with their values and health goals.
How to Find Clinical Trials
Finding suitable clinical trials can be a daunting task for patients seeking participation opportunities. However, several resources are available to assist individuals in locating relevant studies. One of the most comprehensive databases is ClinicalTrials.gov, maintained by the National Institutes of Health (NIH).
This online resource provides detailed information about ongoing and completed clinical trials worldwide, including eligibility criteria, locations, and contact information for study coordinators. Users can search by condition, location, or specific interventions to find trials that match their needs. In addition to online databases, healthcare providers play a vital role in connecting patients with clinical trial opportunities.
Physicians often have access to information about local studies or collaborations with research institutions. Patients should feel empowered to ask their doctors about potential clinical trial options related to their condition. Support groups and patient advocacy organizations can also be valuable resources for finding clinical trials, as they often have networks that share information about ongoing research efforts.
By leveraging these resources, individuals can navigate the complex landscape of clinical trials more effectively.
Eligibility Criteria for Participation
| Metric | Description | Value | Unit |
|---|---|---|---|
| Enrollment Rate | Percentage of eligible patients who agree to participate | 30 | % |
| Average Trial Duration | Time from enrollment to completion of the trial | 18 | Months |
| Retention Rate | Percentage of participants who complete the trial | 85 | % |
| Number of Clinical Trials | Total active clinical trials recruiting participants | 1200 | Trials |
| Common Reasons for Participation | Top motivations for joining clinical trials | Access to new treatments, Contribution to science | Qualitative |
| Common Barriers | Top reasons for declining participation | Fear of side effects, Time commitment | Qualitative |
Eligibility criteria are established for each clinical trial to ensure that participants are appropriate for the study’s objectives and that their inclusion will yield meaningful data. These criteria can vary widely depending on the nature of the trial and the specific health condition being studied. Common factors considered include age, gender, medical history, current medications, and specific disease characteristics.
For instance, a trial investigating a new cancer treatment may require participants to have a confirmed diagnosis of a particular cancer type at a specific stage. While eligibility criteria are designed to protect participants and ensure scientific rigor, they can also pose challenges for potential volunteers. Some individuals may find themselves excluded due to factors beyond their control, such as pre-existing health conditions or previous treatments that disqualify them from participation.
It is essential for potential participants to carefully review these criteria before applying for a trial and to discuss any concerns with their healthcare providers. Understanding eligibility requirements can help individuals make informed decisions about whether to pursue participation in a particular study.
What to Expect During a Clinical Trial
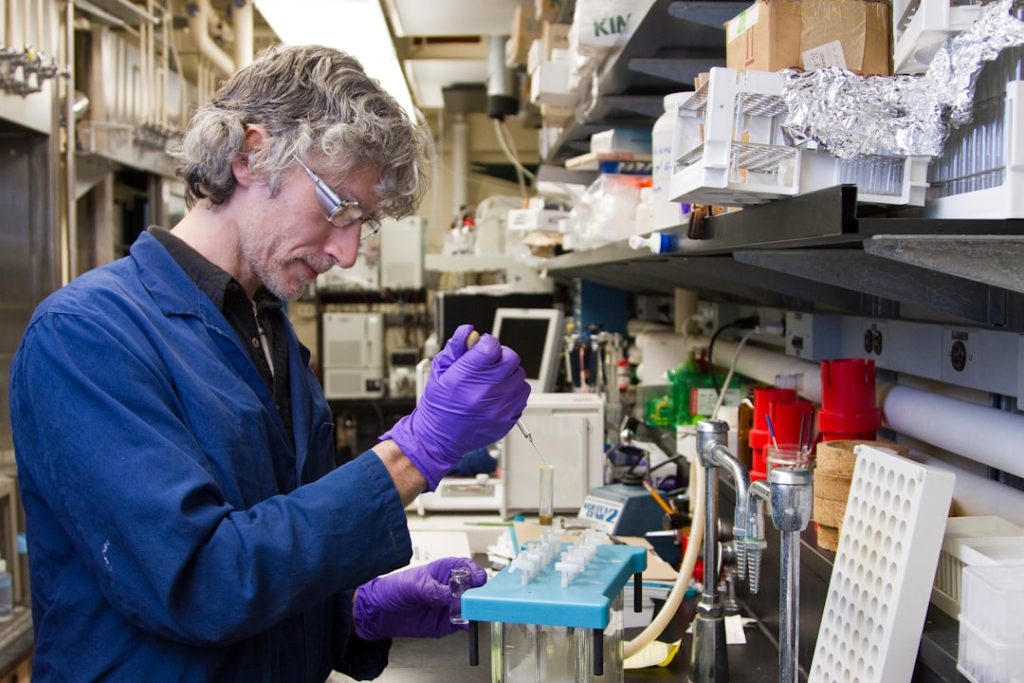
Participating in a clinical trial involves several stages and procedures that vary depending on the study’s design and objectives. Upon enrollment, participants typically undergo a thorough screening process that includes medical evaluations, laboratory tests, and assessments of their health history. This initial phase ensures that they meet the eligibility criteria and helps researchers establish baseline data for comparison throughout the trial.
Once enrolled, participants may be assigned to different groups based on the study’s design—such as those receiving the experimental treatment or those receiving a placebo or standard care. Throughout the trial, participants will attend regular appointments where they will receive treatment and undergo monitoring for side effects or changes in their condition. These visits may include physical examinations, blood tests, imaging studies, or questionnaires about their health status and quality of life.
Participants should expect clear communication from study coordinators regarding what is required of them during the trial and any potential risks involved.
The Impact of Clinical Trial Participation
The impact of clinical trial participation extends far beyond individual experiences; it has profound implications for public health and medical advancement. When participants engage in clinical trials, they contribute to a collective body of knowledge that informs future treatment protocols and healthcare policies. Successful trials can lead to new therapies being approved for widespread use, ultimately improving patient outcomes on a global scale.
Moreover, participation in clinical trials can empower individuals by giving them a voice in their healthcare journey. Many participants report feeling more engaged in their treatment decisions and more informed about their health conditions as a result of their involvement in research studies. This empowerment can foster a sense of agency over one’s health and encourage proactive management of chronic conditions.
Additionally, as more patients participate in clinical trials, it helps diversify research populations, ensuring that findings are applicable across different demographics and improving health equity.
The Future of Medical Research
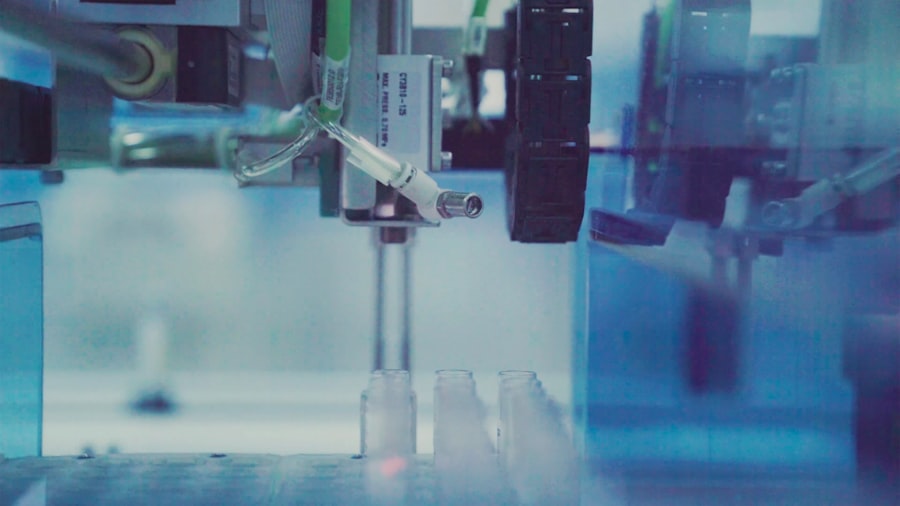
The future of medical research is poised for transformation as advancements in technology and data analytics continue to evolve. Innovations such as artificial intelligence (AI) and machine learning are increasingly being integrated into clinical trial design and execution. These technologies can streamline patient recruitment processes by identifying suitable candidates more efficiently based on electronic health records and other data sources.
Furthermore, AI can assist researchers in analyzing complex datasets generated during trials, leading to faster insights into treatment efficacy and safety. Additionally, there is a growing emphasis on patient-centered research approaches that prioritize participant experiences and preferences in study design. This shift recognizes the importance of involving patients not just as subjects but as active collaborators in research efforts.
By incorporating patient feedback into trial protocols and outcomes measures, researchers can ensure that studies address real-world concerns and improve overall relevance to those affected by specific health conditions. As we look ahead, the integration of digital health technologies—such as wearable devices and telemedicine—will likely play an increasingly significant role in clinical trials. These tools can facilitate remote monitoring of participants’ health status and enhance data collection methods while minimizing the burden on individuals participating in studies.
The convergence of these trends promises to accelerate the pace of medical research while enhancing participant engagement and improving health outcomes across diverse populations.