Phase III clinical trials represent a critical juncture in the drug development process, serving as the final step before a new treatment can be submitted for regulatory approval. These trials are designed to assess the efficacy and safety of a drug in a larger population, typically involving hundreds to thousands of participants. The primary objective is to determine whether the new treatment is more effective than existing therapies or a placebo, thereby providing robust evidence to support its use in clinical practice.
Phase III trials are often randomized and controlled, meaning that participants are assigned to different treatment groups in a way that minimizes bias and ensures the reliability of the results. The design of Phase III trials is complex and multifaceted, often involving multiple sites and diverse patient populations to enhance the generalizability of the findings. This phase is crucial not only for evaluating the therapeutic benefits of a drug but also for identifying any potential adverse effects that may not have been evident in earlier phases.
The data collected during Phase III trials can significantly influence clinical guidelines and treatment protocols, making it essential for researchers to adhere to rigorous scientific standards throughout the process.
Key Takeaways
- Phase III clinical trials are critical for confirming a drug’s efficacy and safety before approval.
- Proper design and implementation ensure reliable and valid trial outcomes.
- Effective participant recruitment and informed consent are essential for ethical compliance.
- Continuous monitoring and accurate data collection are vital for trial integrity.
- Ethical considerations and regulatory approvals guide the conduct and future impact of these trials.
Importance of Phase III Clinical Trials in Drug Development
The significance of Phase III clinical trials cannot be overstated, as they serve as the cornerstone for regulatory approval and subsequent market entry of new pharmaceuticals. These trials provide the definitive evidence needed to demonstrate that a drug is both effective and safe for widespread use. Regulatory agencies, such as the U.S.
Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require comprehensive data from Phase III trials before granting approval for a new drug. This requirement underscores the trials’ role in protecting public health by ensuring that only those treatments that meet stringent safety and efficacy standards are made available to patients. Moreover, Phase III trials often have substantial implications for healthcare systems and economic considerations.
The outcomes of these trials can lead to changes in treatment protocols, influencing how diseases are managed on a population level. For instance, if a new cancer therapy demonstrates significant improvement over existing options, it may prompt healthcare providers to adopt it as a standard treatment, potentially improving patient outcomes and altering survival rates. Additionally, successful Phase III trials can attract investment and funding for further research, thereby fostering innovation within the pharmaceutical industry.
Design and Implementation of Phase III Clinical Trials
The design of Phase III clinical trials is characterized by its complexity and rigor, often employing randomized controlled trial (RCT) methodologies to ensure unbiased results. In an RCT, participants are randomly assigned to either the treatment group receiving the investigational drug or a control group receiving a placebo or standard therapy. This randomization helps eliminate confounding variables that could skew the results, allowing researchers to draw more accurate conclusions about the drug’s efficacy.
Furthermore, many Phase III trials utilize blinding techniques—either single-blind or double-blind—to prevent bias in both participant reporting and investigator assessment. Implementation of these trials involves meticulous planning and coordination among various stakeholders, including clinical research organizations (CROs), healthcare providers, and regulatory bodies. Researchers must develop a detailed protocol outlining the trial’s objectives, methodology, statistical analysis plan, and safety monitoring procedures.
This protocol undergoes rigorous review by institutional review boards (IRBs) or ethics committees to ensure that it meets ethical standards and protects participant welfare. Additionally, logistical considerations such as site selection, training of investigators, and data management systems must be addressed to facilitate smooth execution of the trial.
Participant Recruitment and Informed Consent in Phase III Clinical Trials
Recruiting participants for Phase III clinical trials poses significant challenges, as it requires careful consideration of inclusion and exclusion criteria to ensure that the study population accurately reflects the target patient demographic. Researchers often employ various strategies to enhance recruitment efforts, including outreach through healthcare providers, patient advocacy groups, and online platforms. Effective communication about the trial’s purpose, potential benefits, and risks is essential to attract participants who are willing to contribute to advancing medical knowledge.
Informed consent is a fundamental ethical requirement in clinical research, particularly in Phase III trials where participants may be exposed to new treatments with unknown risks. The informed consent process involves providing potential participants with comprehensive information about the trial, including its objectives, procedures, potential risks and benefits, and their right to withdraw at any time without penalty. This process not only ensures that participants make educated decisions about their involvement but also fosters trust between researchers and participants.
It is crucial that consent forms are written in clear language that is easily understandable, taking into account the diverse backgrounds and literacy levels of potential participants.
Monitoring and Data Collection in Phase III Clinical Trials
| Metric | Description | Typical Range/Value |
|---|---|---|
| Number of Participants | The total number of patients enrolled in the trial | 300 – 3,000 |
| Duration | Length of time the trial is conducted | 1 – 4 years |
| Primary Endpoint | Main outcome measured to determine treatment effect | Varies by study (e.g., survival rate, symptom improvement) |
| Randomization | Method of assigning participants to treatment or control groups | Randomized controlled |
| Blinding | Whether participants and/or investigators are unaware of treatment assignments | Double-blind or single-blind |
| Adverse Event Rate | Percentage of participants experiencing side effects | Varies widely, often 10% – 50% |
| Success Rate | Proportion of trials meeting primary endpoints | Approximately 30% – 50% |
| Regulatory Approval Rate | Percentage of drugs passing phase III and gaining approval | About 60% – 70% |
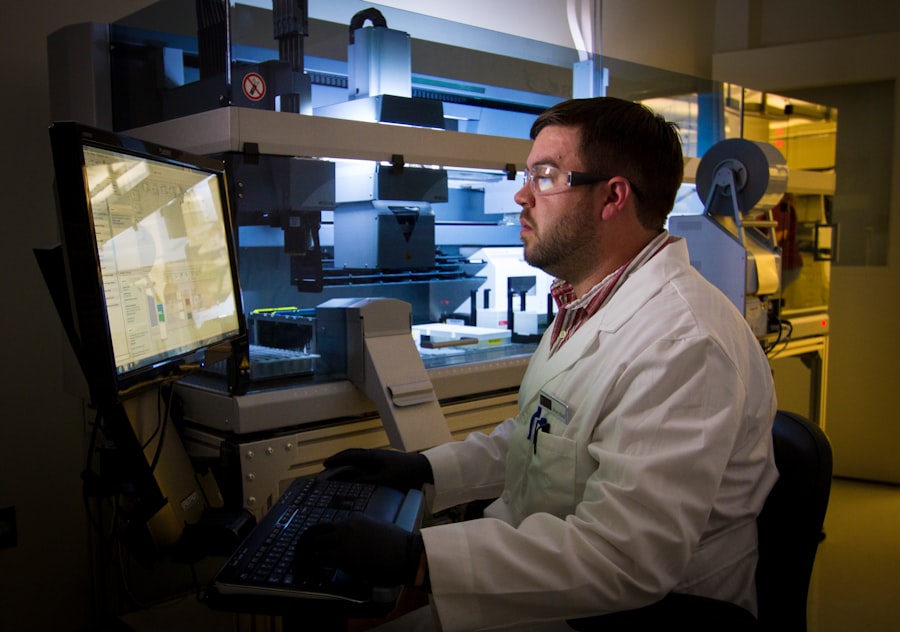
Monitoring during Phase III clinical trials is vital for ensuring participant safety and data integrity throughout the study duration. Independent Data Monitoring Committees (DMCs) are often established to oversee trial progress, assess safety data, and make recommendations regarding trial continuation or modification based on interim findings. These committees play an essential role in identifying any adverse events or unexpected outcomes that may arise during the trial, allowing for timely interventions if necessary.
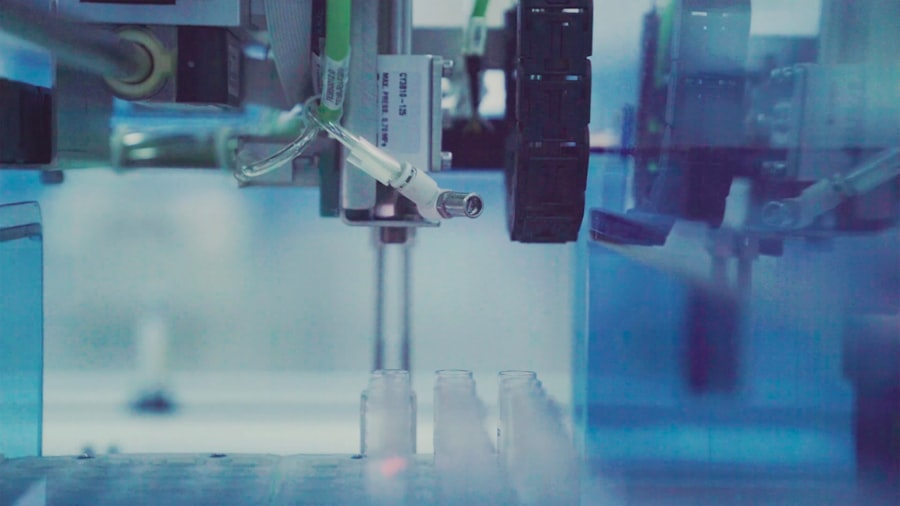
Data collection methods in Phase III trials are meticulously designed to capture relevant information while minimizing bias. Researchers utilize standardized case report forms (CRFs) to systematically record participant data, including demographic information, clinical outcomes, laboratory results, and adverse events. Electronic data capture systems are increasingly employed to streamline data collection processes and enhance accuracy.
Rigorous quality control measures are implemented to ensure that data is collected consistently across all trial sites, which is crucial for maintaining the validity of the study’s findings.
Analysis and Interpretation of Results in Phase III Clinical Trials
The analysis of data collected during Phase III clinical trials is a critical step that determines whether the investigational drug meets its primary endpoints—typically defined as specific clinical outcomes such as improvement in symptoms or survival rates. Statistical methods are employed to analyze the data rigorously, allowing researchers to assess the significance of their findings. Common statistical tests include t-tests for comparing means between groups or chi-square tests for categorical data analysis.
The choice of statistical methods depends on the study design and the nature of the data collected. Interpreting results from Phase III trials requires careful consideration of both statistical significance and clinical relevance. A statistically significant result indicates that the observed effect is unlikely due to chance; however, it does not necessarily imply that the effect is meaningful in a real-world context.
Researchers must evaluate whether the magnitude of benefit justifies any associated risks or side effects. For instance, if a new medication shows a statistically significant reduction in disease progression but comes with severe adverse effects, clinicians must weigh these factors when considering its use in practice.
Ethical Considerations and Regulatory Approval in Phase III Clinical Trials
Ethical considerations are paramount throughout all phases of clinical research, particularly in Phase III trials where large numbers of participants are involved. Researchers must adhere to principles outlined in ethical guidelines such as the Declaration of Helsinki and Good Clinical Practice (GCP) standards. These guidelines emphasize respect for persons, beneficence, and justice—ensuring that participants are treated with dignity, that their welfare is prioritized, and that vulnerable populations are protected from exploitation.
Regulatory approval is contingent upon comprehensive documentation of trial conduct and results submitted to agencies like the FDA or EMThis submission includes detailed reports on trial design, methodology, statistical analyses, safety data, and any adverse events encountered during the study. Regulatory bodies conduct thorough reviews to assess whether the benefits of the new treatment outweigh its risks before granting marketing authorization. This process can be lengthy and may involve additional requests for information or clarification from sponsors.
Future Implications and Impact of Phase III Clinical Trials
The outcomes of Phase III clinical trials have far-reaching implications for both patients and healthcare systems worldwide. Successful trials can lead to the introduction of innovative therapies that significantly improve patient outcomes across various medical conditions. For example, advancements in oncology have been driven by robust Phase III studies demonstrating improved survival rates with novel immunotherapies or targeted agents compared to traditional chemotherapy regimens.
Moreover, as healthcare continues to evolve with advancements in technology and personalized medicine approaches, Phase III trials will likely adapt accordingly. The integration of real-world evidence (RWE) into trial designs may become more prevalent, allowing researchers to assess treatment effectiveness in broader populations outside controlled environments. This shift could enhance our understanding of how new therapies perform in everyday clinical settings while also addressing issues related to health disparities among different demographic groups.
In conclusion, Phase III clinical trials play an indispensable role in drug development by providing critical evidence regarding safety and efficacy before new treatments reach patients. Their design, implementation, monitoring processes, ethical considerations, and regulatory pathways are all integral components that ensure rigorous scientific standards are upheld throughout this pivotal stage of research. As we look toward the future, ongoing innovations in trial methodologies will continue to shape how we evaluate new therapies and ultimately improve patient care on a global scale.




