Phase IV clinical trials, often referred to as post-marketing studies, represent a critical stage in the drug development process. Unlike earlier phases, which focus primarily on establishing safety and efficacy in controlled environments, Phase IV trials occur after a drug has received regulatory approval and is available on the market. These trials are essential for gathering additional information about a drug’s long-term effects, optimal usage, and overall impact on public health.
They serve as a bridge between clinical research and real-world application, allowing researchers to observe how a medication performs in diverse populations and under varying conditions. The significance of Phase IV trials cannot be overstated. They provide an opportunity to monitor the drug’s performance in a broader patient population, which may include individuals with comorbidities or those taking multiple medications—factors often excluded from earlier trial phases.
This phase is crucial for identifying rare side effects that may not have been evident during the initial trials due to limited sample sizes or specific inclusion criteria. As such, Phase IV trials play a vital role in ensuring that healthcare providers and patients have access to comprehensive information regarding the benefits and risks associated with a medication.
Key Takeaways
- Phase IV clinical trials occur after a drug’s market approval to monitor long-term safety and effectiveness.
- These trials aim to detect rare or long-term adverse effects not seen in earlier phases.
- Post-market surveillance is critical for ongoing safety monitoring and regulatory compliance.
- Comparative effectiveness research in Phase IV helps determine how a drug performs against existing treatments.
- Ethical considerations, including informed consent and patient recruitment, remain paramount throughout the trial.
Purpose and Goals of Phase IV Clinical Trial
The primary purpose of Phase IV clinical trials is to gather extensive data on the long-term safety and effectiveness of a drug once it is in widespread use. This phase aims to identify any adverse effects that may not have been apparent during earlier trials, particularly those that occur infrequently or only manifest after prolonged exposure. By monitoring the drug’s performance in a real-world setting, researchers can assess its impact on various populations, including different age groups, ethnicities, and individuals with pre-existing health conditions.
Another critical goal of Phase IV trials is to evaluate the drug’s effectiveness in comparison to other available treatments. This comparative effectiveness research helps healthcare providers make informed decisions about prescribing practices and treatment protocols. For instance, if a new medication is found to be more effective than existing therapies for a particular condition, it may lead to changes in clinical guidelines and improve patient outcomes.
Additionally, Phase IV trials can help identify optimal dosing regimens and potential drug interactions, further enhancing the therapeutic landscape.
Post-Market Surveillance and Safety Monitoring
Post-market surveillance is a fundamental component of Phase IV clinical trials, focusing on the ongoing assessment of a drug’s safety profile after it has been approved for public use. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) require manufacturers to conduct post-marketing studies to monitor adverse events and ensure that any emerging safety concerns are promptly addressed.
This surveillance can take various forms, including spontaneous reporting systems, registries, and observational studies. Safety monitoring during this phase involves collecting data from healthcare providers, patients, and other stakeholders to identify any potential safety signals. For example, if a significant number of patients report adverse reactions after starting a new medication, this information can trigger further investigation into the drug’s safety profile.
The findings from these studies can lead to label changes, additional warnings, or even the withdrawal of a drug from the market if necessary. This ongoing vigilance is crucial for maintaining public trust in pharmaceutical products and ensuring that patients receive safe and effective treatments.
Comparative Effectiveness Research in Phase IV Clinical Trial
Comparative effectiveness research (CER) is an integral aspect of Phase IV clinical trials, focusing on evaluating the relative benefits and risks of different treatment options available for a specific condition. This research aims to provide healthcare providers with evidence-based information that can guide clinical decision-making. By comparing new drugs with existing therapies or placebo treatments, researchers can determine which options yield better outcomes for patients.
For instance, consider a Phase IV trial assessing a new anticoagulant medication against traditional warfarin therapy. Researchers would analyze various factors such as efficacy in preventing thromboembolic events, incidence of bleeding complications, quality of life measures, and overall patient satisfaction. The results of such studies can significantly influence treatment guidelines and help clinicians choose the most appropriate therapy for their patients based on individual needs and circumstances.
Regulatory Requirements and Compliance in Phase IV Clinical Trial
| Metric | Description | Typical Range/Value | Importance |
|---|---|---|---|
| Sample Size | Number of participants enrolled in the trial | Several hundred to several thousand | Ensures statistical power to detect rare adverse events |
| Duration | Length of time the trial is conducted | Months to several years | Allows long-term safety and effectiveness monitoring |
| Primary Endpoint | Main outcome measured to assess drug safety or effectiveness | Adverse event incidence, long-term efficacy | Determines post-marketing safety profile |
| Adverse Event Rate | Frequency of side effects or adverse reactions | Varies by drug; often <1% to 10% | Critical for ongoing safety assessment |
| Compliance Rate | Percentage of participants adhering to treatment protocol | Typically 70% to 95% | Impacts reliability of safety and efficacy data |
| Data Collection Methods | Techniques used to gather trial data | Electronic health records, patient diaries, lab tests | Ensures comprehensive and accurate data capture |
| Regulatory Reporting | Frequency and type of reports submitted to authorities | Periodic safety update reports (PSURs), annual reports | Maintains compliance with regulatory requirements |
Regulatory requirements for Phase IV clinical trials are designed to ensure that studies are conducted ethically and that the data generated are reliable and valid. Regulatory agencies like the FDA or the European Medicines Agency (EMA) set forth guidelines that govern the design, conduct, and reporting of these trials. Compliance with these regulations is paramount for maintaining public safety and trust in pharmaceutical products.
One key aspect of regulatory compliance involves submitting detailed protocols for review before initiating a Phase IV trial. These protocols outline the study’s objectives, methodology, statistical analysis plans, and safety monitoring procedures. Additionally, researchers must adhere to Good Clinical Practice (GCP) guidelines, which encompass ethical considerations such as informed consent and patient confidentiality.
Failure to comply with these regulations can result in severe consequences, including fines, sanctions, or even the revocation of a drug’s market approval.
Patient Recruitment and Informed Consent in Phase IV Clinical Trial
Patient recruitment for Phase IV clinical trials presents unique challenges compared to earlier phases of clinical research. Since these trials often involve larger populations and diverse demographics, researchers must develop strategies to engage patients effectively. Recruitment efforts may include outreach through healthcare providers, community organizations, or online platforms to reach potential participants who may benefit from the study.
Informed consent is another critical component of patient recruitment in Phase IV trials. Participants must be fully aware of the study’s purpose, procedures, potential risks, and benefits before agreeing to take part. This process is particularly important in post-marketing studies where patients may already be using the medication under investigation.
Researchers must ensure that participants understand their rights and can make informed decisions about their involvement in the trial without any coercion or undue influence.
Data Collection and Analysis in Phase IV Clinical Trial
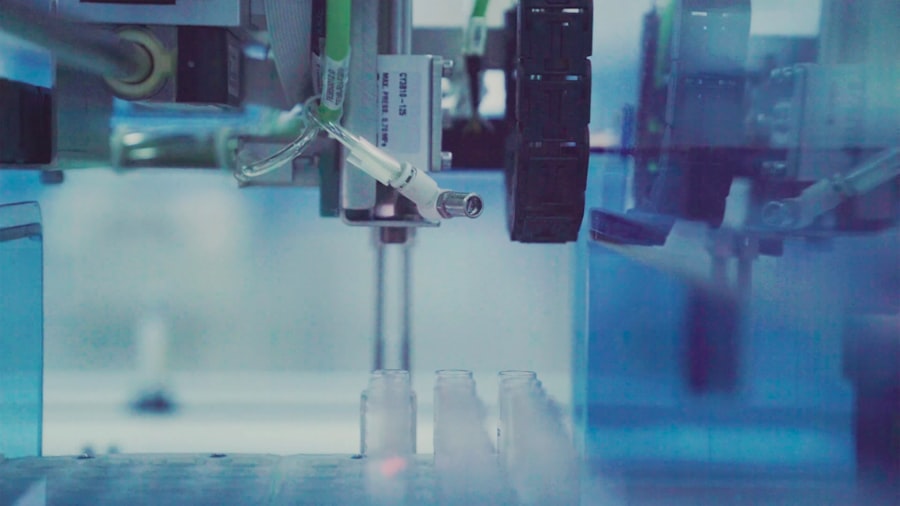
Data collection in Phase IV clinical trials is multifaceted and often involves various methodologies to capture comprehensive information about a drug’s performance in real-world settings. Researchers may utilize electronic health records (EHRs), patient registries, surveys, and direct patient interviews to gather data on treatment outcomes, adverse events, and patient-reported outcomes. The diversity of data sources allows for a more holistic understanding of how a medication affects different populations over time.
Once data is collected, rigorous statistical analysis is conducted to interpret the findings accurately. Researchers employ various analytical techniques to assess the relationship between treatment exposure and outcomes while controlling for confounding variables that could skew results. For example, if a study examines the long-term effects of a new diabetes medication on cardiovascular health, analysts must account for factors such as age, gender, baseline health status, and concurrent medications that could influence cardiovascular outcomes.
The robustness of these analyses is crucial for drawing valid conclusions that can inform clinical practice.
Ethical Considerations in Phase IV Clinical Trial
Ethical considerations are paramount in Phase IV clinical trials due to the complexities involved in post-marketing research. One significant ethical concern revolves around patient safety; researchers must prioritize monitoring adverse events and ensuring that any emerging safety issues are addressed promptly. Transparency in reporting findings is also essential; stakeholders must be informed about both positive outcomes and potential risks associated with the medication.
Additionally, ethical considerations extend to issues of equity and access. Researchers must ensure that diverse populations are represented in Phase IV trials to avoid disparities in treatment outcomes based on race, ethnicity, or socioeconomic status. Engaging with community stakeholders can help address these concerns by fostering trust and encouraging participation from underrepresented groups.
Ultimately, ethical conduct in Phase IV clinical trials not only protects participants but also enhances the credibility of research findings and contributes to improved public health outcomes.




