Clinical research serves as the essential link between laboratory discoveries and their implementation in patient care within the medical field. It includes diverse studies designed to advance understanding of health and disease, assess new treatments, and enhance current medical practices. The fundamental objective is to produce evidence that guides clinical decision-making and improves patient outcomes.
Beyond academic pursuits, clinical research significantly impacts public health initiatives, healthcare policy development, and medical science progression. The clinical research environment incorporates multiple methodological approaches, including randomized controlled trials, observational studies, and cohort studies. Each methodology presents distinct advantages and limitations, with study design selection determined by the specific research objectives.
Randomized controlled trials represent the gold standard for intervention efficacy evaluation due to their capacity to reduce bias and control confounding variables. Observational studies prove more suitable for investigating rare diseases or long-term outcomes where controlled experimentation is impractical. Researchers must comprehend these methodological distinctions to effectively navigate clinical investigation complexities.
Key Takeaways
- Clinical research involves systematic study to evaluate medical interventions and improve patient care.
- Effective study design and clear protocols are essential for reliable and valid research outcomes.
- Ethical recruitment and informed consent protect participant rights and ensure study integrity.
- Accurate data collection and continuous monitoring are critical for maintaining data quality.
- Regulatory compliance and ethical oversight safeguard participant safety and support credible dissemination of findings.
Study Design and Protocol Development
The foundation of any successful clinical research project lies in its study design and protocol development. A well-structured study design outlines the framework for how the research will be conducted, detailing the objectives, methodology, and statistical analysis plan. This blueprint serves as a guide for researchers, ensuring that all aspects of the study are meticulously planned and executed.
The development of a robust protocol is essential not only for the integrity of the research but also for compliance with regulatory standards. In crafting a study protocol, researchers must consider several key elements, including the target population, sample size, intervention details, and outcome measures. For example, if a study aims to evaluate a new drug for hypertension, the protocol must specify the inclusion and exclusion criteria for participants, the dosage and administration route of the drug, and the primary and secondary endpoints to be measured.
Additionally, researchers must outline their plans for randomization and blinding to reduce bias. The protocol must also address potential challenges that may arise during the study, such as participant dropout or adverse events, and propose strategies for mitigating these risks.
Participant Recruitment and Informed Consent

Recruiting participants for clinical research is a critical step that can significantly influence the validity and generalizability of study findings. Effective recruitment strategies are essential to ensure that a representative sample is obtained, which enhances the external validity of the research. Researchers often employ various methods to reach potential participants, including advertisements in healthcare settings, outreach through community organizations, and collaboration with healthcare providers.
The choice of recruitment strategy may depend on the target population’s characteristics and the nature of the study. Informed consent is another crucial aspect of participant recruitment. It is not merely a formality but a fundamental ethical requirement that ensures participants are fully aware of what their involvement entails.
The informed consent process involves providing potential participants with comprehensive information about the study’s purpose, procedures, risks, benefits, and their rights as participants. This process must be conducted in a manner that is understandable to individuals from diverse backgrounds. Researchers must also ensure that consent is obtained voluntarily without any coercion or undue influence.
This ethical obligation fosters trust between researchers and participants and upholds the integrity of the research process.
Data Collection and Monitoring
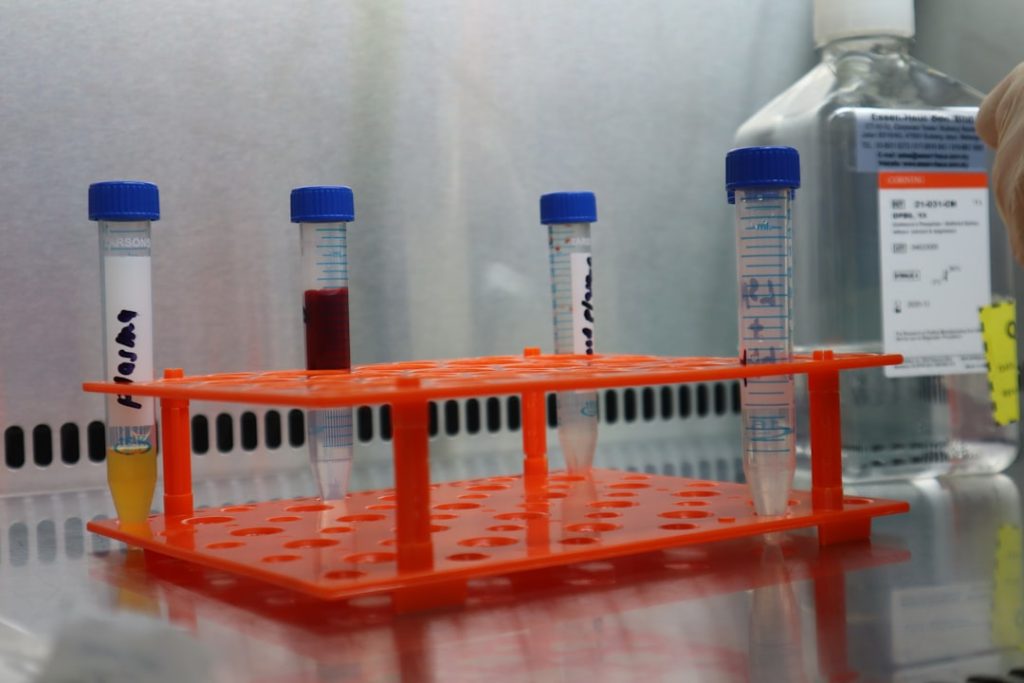
Once participants have been recruited and consented, data collection begins—a phase that requires meticulous attention to detail to ensure accuracy and reliability. Data collection methods can vary widely depending on the study design and objectives. Common techniques include surveys, interviews, clinical assessments, laboratory tests, and electronic health records.
Each method has its advantages and limitations; for instance, while surveys can gather large amounts of data quickly, they may be subject to response bias. Monitoring data collection is equally important to maintain the quality of the research. This involves regular oversight to ensure that data is being collected according to the established protocol and that any deviations are documented and addressed promptly.
Data monitoring committees may be established to oversee ongoing studies, particularly those involving high-risk interventions or vulnerable populations. These committees play a critical role in safeguarding participant welfare by reviewing data for safety signals and ensuring that the study remains ethically sound throughout its duration.
Data Analysis and Interpretation
| Phase | Purpose | Number of Participants | Duration | Key Focus | Outcome |
|---|---|---|---|---|---|
| Phase 0 | Microdosing to gather preliminary data on pharmacodynamics and pharmacokinetics | 10-15 healthy volunteers | Several months | Safety and biological activity | Initial human data to support further testing |
| Phase I | Assess safety, dosage range, and side effects | 20-100 healthy volunteers or patients | Several months | Safety and dosage | Safe dosage range and identification of side effects |
| Phase II | Evaluate efficacy and side effects | 100-300 patients | Several months to 2 years | Efficacy and side effects | Preliminary data on effectiveness and further safety evaluation |
| Phase III | Confirm effectiveness, monitor side effects, compare to commonly used treatments | 1,000-3,000 patients | 1-4 years | Effectiveness and safety | Definitive evidence for regulatory approval |
| Phase IV | Post-marketing surveillance to detect long-term effects | Various (thousands) | Ongoing | Long-term safety and effectiveness | Monitoring of drug in general population |
After data collection is complete, researchers embark on data analysis—a process that transforms raw data into meaningful insights. The choice of statistical methods depends on the study design and research questions posed. For example, if a randomized controlled trial aims to compare two treatment groups’ efficacy, researchers might employ techniques such as t-tests or ANOVA to assess differences in outcomes.
In contrast, observational studies may utilize regression analyses to control for confounding variables. Interpreting data requires not only statistical expertise but also a deep understanding of the clinical context. Researchers must consider whether their findings are clinically significant in addition to being statistically significant.
For instance, a new treatment may show a statistically significant reduction in symptoms compared to a placebo; however, if the effect size is small or not clinically meaningful, its practical implications may be limited. Furthermore, researchers must be cautious about overgeneralizing their findings beyond the study population or context in which they were derived.
Regulatory Approval and Ethical Considerations

Navigating regulatory approval is a critical step in conducting clinical research. Before initiating a study involving human participants, researchers must submit their protocols to institutional review boards (IRBs) or ethics committees for review. These bodies assess whether the proposed research meets ethical standards and protects participants’ rights and welfare.
The review process often involves evaluating informed consent procedures, risk-benefit analyses, and plans for data confidentiality. Ethical considerations extend beyond regulatory compliance; they are integral to maintaining public trust in clinical research. Researchers must be vigilant about potential conflicts of interest that could compromise study integrity.
Transparency in funding sources and affiliations with pharmaceutical companies or other stakeholders is essential to uphold ethical standards. Additionally, researchers should prioritize participant safety throughout the study by implementing monitoring mechanisms for adverse events and ensuring that participants can withdraw from the study at any time without penalty.
Publication and Dissemination of Results
Once data analysis is complete and findings are interpreted, researchers face the task of disseminating their results to the broader scientific community and stakeholders. Publication in peer-reviewed journals is one of the most common avenues for sharing research findings; this process involves submitting manuscripts that undergo rigorous evaluation by experts in the field before publication. Peer review serves as a quality control mechanism that helps ensure that only high-quality research enters the scientific literature.
Dissemination goes beyond publication; it also includes presenting findings at conferences, engaging with healthcare professionals through workshops or seminars, and utilizing social media platforms to reach wider audiences. Effective communication of results is crucial for translating research into practice; healthcare providers need access to evidence-based information to inform their clinical decisions. Moreover, engaging with patients and advocacy groups can help bridge the gap between research findings and real-world applications.
Future Directions and Implications for Clinical Practice
As clinical research continues to evolve, several future directions hold promise for enhancing its impact on healthcare practice. One significant trend is the increasing use of technology in clinical trials—such as telemedicine for remote monitoring or mobile health applications for data collection—which can improve participant engagement and streamline processes. These innovations have become particularly relevant in light of recent global health challenges that necessitate flexible approaches to research.
Another important consideration is the emphasis on patient-centered research approaches that prioritize participants’ perspectives throughout the research process. Engaging patients as partners in research can lead to more relevant questions being asked and more meaningful outcomes being measured. This shift towards patient-centeredness not only enhances the quality of research but also fosters trust between researchers and communities.
The implications of these advancements are profound; as clinical research becomes more accessible and aligned with patient needs, it has the potential to drive significant improvements in healthcare delivery and outcomes. By continuing to refine methodologies, uphold ethical standards, and prioritize transparency in dissemination efforts, clinical research can remain at the forefront of medical innovation—ultimately leading to better health for individuals and populations alike.