Clinical research nurses (CRNs) are integral to the successful execution of clinical trials and, consequently, play a significant role in shaping patient outcomes. Their work bridges the gap between research protocols and direct patient care, ensuring both scientific rigor and ethical considerations are maintained. This article explores the multifaceted impact of CRNs on patients participating in clinical research.
The role of a CRN has evolved considerably since the inception of organized clinical trials. Initially, the focus was often purely on data collection and procedural adherence. However, contemporary understanding recognizes the CRN as a central figure in patient well-being within the research context.
Historical Context of the CRN Role
Early clinical research often relied on physicians or general ward nurses to manage study participants. As the complexity of trials increased, and ethical guidelines became more stringent, the need for a specialized nursing role became apparent. This specialization allowed for dedicated attention to protocol requirements, patient safety, and data integrity. The emergence of Good Clinical Practice (GCP) guidelines further solidified the necessity of a distinct CRN role.
Current Scope of Practice
Today’s CRN navigates a complex landscape. Their responsibilities extend beyond direct patient contact to encompass regulatory compliance, data management, and ethical oversight. They act as a cornerstone, holding together the diverse elements of a research study. Their practice integrates nursing expertise with a deep understanding of research methodology, making them uniquely qualified to mitigate risks and optimize patient experiences in research settings. This integration is crucial for the reliability and validity of research findings and, consequently, for improvements in standard medical care.
Direct Patient Care and Advocacy
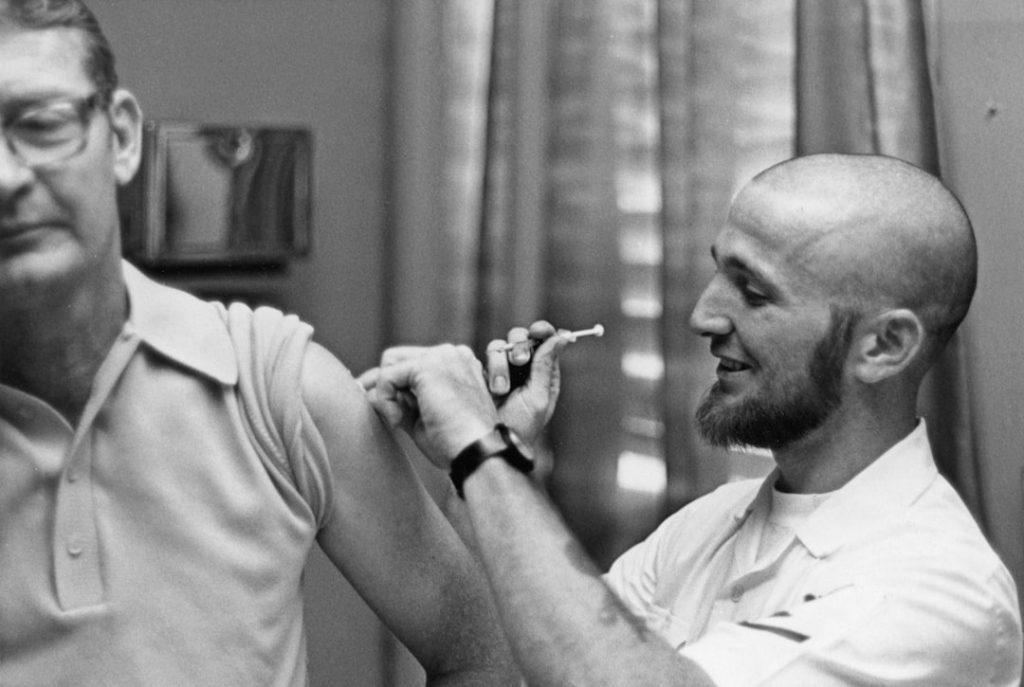
One of the most consequential contributions of CRNs is their direct engagement with patients. This engagement is often the primary touchpoint for participants throughout a study, making the CRN a crucial source of support and information.
Patient Education and Informed Consent
The informed consent process is a critical ethical prerequisite for any clinical trial. CRNs are often responsible for explaining complex study protocols, potential risks and benefits, and alternative treatment options in an understandable manner. They facilitate an environment where patients can ask questions and make autonomous decisions. A well-informed patient is more likely to adhere to the study protocol and less likely to withdraw due to misunderstandings. This comprehensive educational role ensures that patients enter research with a clear understanding of their role and the study’s implications.
Monitoring and Managing Adverse Events
Clinical trials, by their nature, involve investigating novel treatments or interventions, which carry inherent uncertainties. CRNs are at the forefront of monitoring patients for adverse events (AEs) and serious adverse events (SAEs). Their clinical assessment skills enable early detection and prompt intervention, often mitigating potential harm. They are responsible for accurate and timely reporting of these events, which is critical for patient safety and regulatory compliance. The CRN acts as an early warning system, using their clinical acumen to discern deviations from expected patient responses.
Emotional Support and Patient Retention
Participating in a clinical trial can be a challenging experience for patients, fraught with anxiety, hope, and uncertainty. CRNs provide essential emotional support, acting as a consistent and empathetic point of contact. This support infrastructure helps to maintain patient morale and, consequently, improve retention rates. High retention rates are vital for the statistical power and generalizability of trial findings. The CRN often serves as a lifeline, offering a blend of clinical expertise and human compassion that can be invaluable to patients navigating the complexities of a research study.
Data Integrity and Research Fidelity

The validity of research findings hinges on the accuracy and completeness of collected data. CRNs are instrumental in upholding data integrity, thereby protecting the scientific merit of a study.
Accurate Data Collection and Documentation
CRNs are responsible for meticulous data collection according to study protocols. This involves precise measurements, accurate symptom recording, and diligent documentation of interventions and patient responses. Errors in data collection can compromise the entire study, leading to flawed conclusions and wasted resources. Their role is akin to a meticulous archivist, ensuring every piece of information is recorded correctly and completely.
Adherence to Protocol and Standard Operating Procedures
Deviation from study protocols can introduce bias and invalidate trial results. CRNs ensure strict adherence to all protocol requirements and standard operating procedures (SOPs). This includes appropriate dosing, timing of interventions, and correct specimen collection. Their vigilance acts as a bulwark against inconsistencies, preserving the scientific rigor of the trial. The CRN operates as the guardian of the research blueprint, ensuring all steps are followed precisely.
Quality Assurance and Audits
CRNs often participate in internal quality assurance activities, reviewing collected data and processes to identify potential issues. They also play a key role in preparing for and participating in external audits by regulatory bodies or sponsors. Their clear and organized documentation is crucial for demonstrating compliance and maintaining the credibility of the research site. This proactive role in quality ensures that the research process can withstand scrutiny.
Ethical Considerations and Regulatory Compliance

Clinical research is heavily regulated to protect human subjects. CRNs are at the vanguard of ensuring ethical conduct and regulatory compliance throughout the study lifecycle.
Upholding Patient Rights and Confidentiality
CRNs are staunch advocates for patient rights, ensuring that participants are treated with dignity and respect. They strictly adhere to confidentiality protocols, safeguarding sensitive patient information in accordance with privacy regulations such as HIPAA. Their commitment to these principles reinforces trust between researchers and participants. The CRN acts as a sentinel, protecting the fundamental rights and privacy of each participant.
Compliance with Good Clinical Practice (GCP)
Good Clinical Practice (GCP) is an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve the participation of human subjects. CRNs are trained in and strictly adhere to GCP guidelines. This adherence ensures the credibility of the data and the safety of the participants, which are paramount for regulatory approval of new treatments. Their understanding of GCP is not merely academic; it is applied knowledge that governs every aspect of their practice.
Liaising with Institutional Review Boards (IRBs)
CRNs often assist in preparing submissions to Institutional Review Boards (IRBs) or Ethics Committees (ECs), which are independent bodies responsible for reviewing and approving research protocols involving human subjects. They may also be involved in responding to queries from these boards, ensuring that ethical concerns are addressed proactively. This liaison role facilitates ethical oversight and ensures that the research remains aligned with societal values and ethical principles.
Impact on Subsequent Clinical Practice
| Metric | Description | Typical Value/Range | Unit |
|---|---|---|---|
| Average Patient Enrollment | Number of patients enrolled in clinical trials per month | 5 – 20 | patients/month |
| Protocol Compliance Rate | Percentage of clinical trial procedures completed according to protocol | 95 – 100 | % |
| Adverse Event Reporting Time | Average time taken to report adverse events after occurrence | 24 – 48 | hours |
| Patient Retention Rate | Percentage of patients who complete the clinical trial | 80 – 95 | % |
| Data Entry Accuracy | Percentage of clinical data entered without errors | 98 – 100 | % |
| Time Spent on Patient Education | Average time spent educating patients about the trial and procedures | 30 – 60 | minutes/session |
| Number of Clinical Trials Supported | Number of active clinical trials a nurse supports simultaneously | 1 – 5 | trials |
The meticulous work of CRNs in clinical trials has a ripple effect, directly influencing the development of new treatments and subsequently improving standard patient care.
Advancing Medical Knowledge and New Therapies
By contributing to robust and reliable data collection, CRNs enable the accurate assessment of experimental treatments. The insights gained from these trials form the bedrock of evidence-based medicine, leading to the development and approval of new and effective therapies. Without their contributions, the pipeline for medical innovation would be severely hampered. The CRN’s efforts are a vital current in the river of medical progress.
Translating Research Findings into Practice
CRNs often play a role in the dissemination of research findings, either informally through discussions with clinical colleagues or formally through presentations and publications. Their direct experience with the study population and the intervention provides valuable context for interpreting results and informing future clinical practice. This translational role bridges the divide between experimental results and practical application.
Shaping Future Research Directions
The day-to-day interactions and observations of CRNs can identify unmet patient needs or emergent clinical questions. This ground-level insight can inform and shape the design of future clinical trials, ensuring that research remains relevant and addresses genuine healthcare challenges. Their unique perspective on patient experiences within a research framework offers a fertile ground for identifying new avenues of investigation.
In conclusion, the clinical research nurse is an indispensable conduit through which new treatments and interventions are developed and rigorously tested. Their impact on patient outcomes is multifaceted, encompassing direct care, ethical oversight, data integrity, and the ultimate translation of research into improved medical care. Without the dedicated and specialized expertise of CRNs, the integrity and efficacy of the clinical research enterprise, and by extension the quality of global healthcare, would be significantly diminished. Their presence is a foundational element in the complex machinery of medical progress.