In the realm of clinical research, the efficiency of data collection processes can significantly influence the overall success of a study. Streamlined data collection refers to the systematic approach of gathering information in a manner that minimizes redundancy and maximizes accuracy. Traditional methods often involve cumbersome paperwork and manual entry, which can lead to errors and delays.
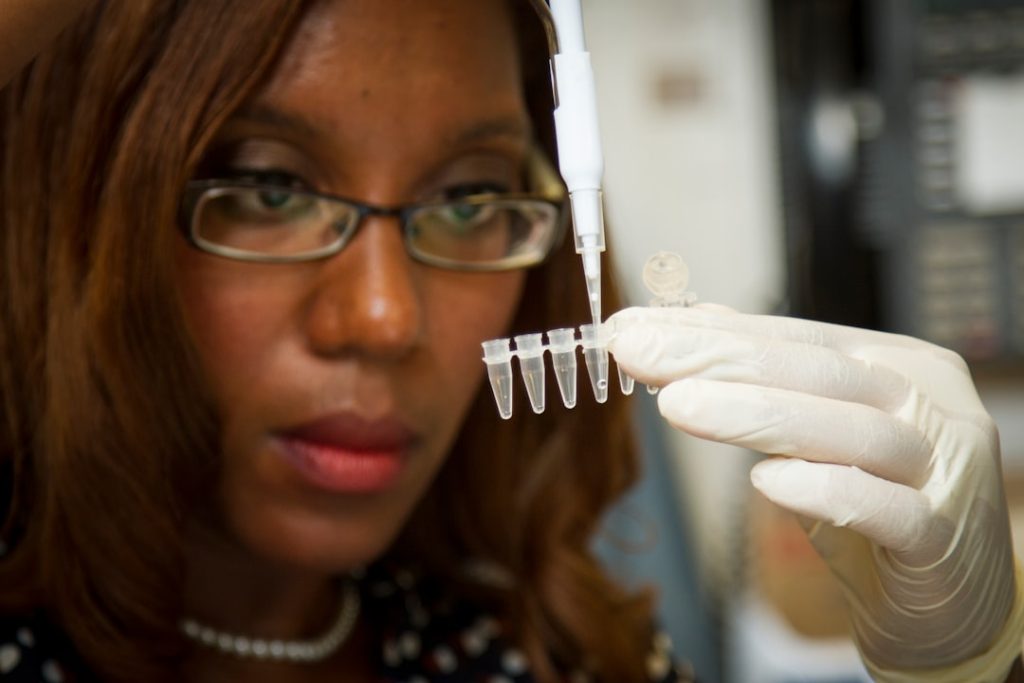
However, with the advent of electronic data capture (EDC) systems, researchers can now collect data in real-time, directly from the source. This transition not only reduces the time spent on data entry but also enhances the quality of the data collected. Moreover, streamlined data collection facilitates better participant engagement.
By utilizing mobile applications and online platforms, researchers can reach participants more effectively, allowing for quicker responses and more comprehensive data sets. For instance, a clinical trial investigating a new medication for diabetes may employ a mobile app that allows participants to log their blood sugar levels daily. This immediate feedback loop not only keeps participants engaged but also provides researchers with timely insights into the medication’s efficacy.
The integration of technology in data collection processes is transforming how clinical trials are conducted, making them more efficient and participant-friendly.
Key Takeaways
- Streamlined data collection simplifies and accelerates gathering research information.
- Real-time data monitoring enables immediate oversight and quick issue resolution.
- Improved data accuracy reduces errors, enhancing the reliability of study results.
- Enhanced patient safety is achieved through better tracking and management of participant data.
- Faster study timelines and cost savings result from efficient study management and regulatory compliance.
Real-time Data Monitoring
Real-time data monitoring is a critical advancement in clinical research that allows researchers to track data as it is being collected. This capability is particularly important in studies where patient safety is paramount, such as those involving new drug therapies or medical devices. By employing real-time monitoring systems, researchers can identify trends and anomalies almost instantaneously, enabling them to make informed decisions quickly.
For example, if a sudden spike in adverse events is detected during a trial, researchers can immediately investigate the cause and take necessary actions to protect participants. The benefits of real-time data monitoring extend beyond just safety; they also enhance the overall quality of the research. Continuous oversight allows for immediate adjustments to study protocols if needed, ensuring that the research remains aligned with its objectives.
In a recent clinical trial for a cardiovascular drug, real-time monitoring enabled researchers to adjust dosages based on participants’ responses, ultimately leading to more accurate results. This dynamic approach not only improves the integrity of the study but also fosters a culture of responsiveness and adaptability within research teams.
Improved Data Accuracy

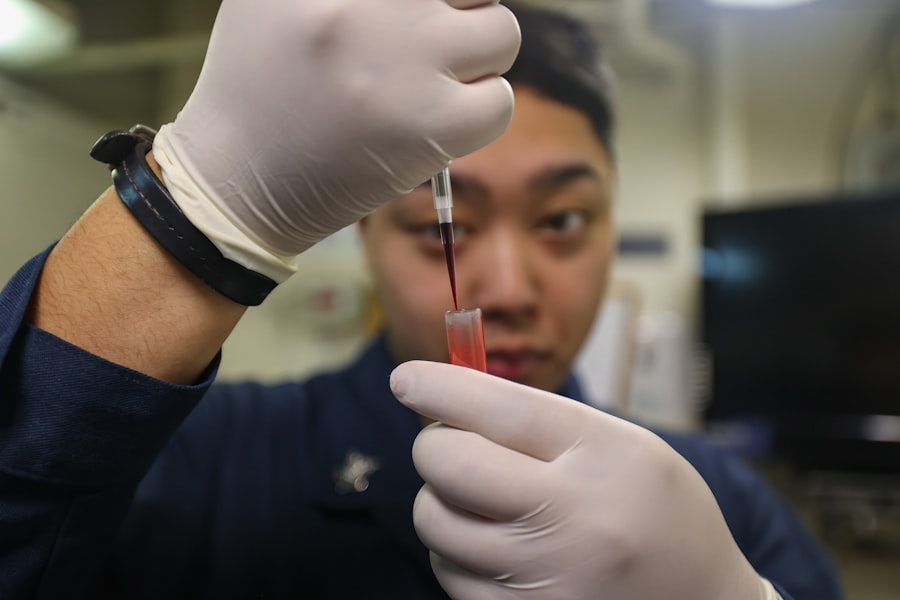
Data accuracy is paramount in clinical research, as even minor errors can lead to significant consequences in patient outcomes and regulatory compliance. Improved data accuracy is achieved through various means, including automated data entry systems and rigorous validation processes. By minimizing human intervention in data collection and entry, researchers can significantly reduce the likelihood of errors.
For instance, using barcode scanning technology to capture patient information ensures that data is recorded correctly and consistently. Additionally, advanced analytics tools play a crucial role in enhancing data accuracy. These tools can identify inconsistencies or outliers in datasets that may indicate errors or require further investigation.
For example, if a participant’s reported weight fluctuates dramatically over a short period, analytics software can flag this anomaly for review. This proactive approach not only helps maintain high standards of data integrity but also builds trust among stakeholders, including regulatory bodies and funding organizations.
Enhanced Patient Safety
| Metric | Description | Typical Value/Range | Impact on Patient Safety |
|---|---|---|---|
| Medication Error Rate | Percentage of medication errors per 1,000 prescriptions | 1-5 errors per 1,000 prescriptions | Lower rates indicate improved medication safety |
| Hospital-Acquired Infection (HAI) Rate | Number of HAIs per 1,000 patient days | 0.5-2 infections per 1,000 patient days | Reduction decreases patient morbidity and mortality |
| Patient Fall Rate | Number of patient falls per 1,000 patient days | 2-8 falls per 1,000 patient days | Lower fall rates reduce injury risk |
| Adverse Drug Event (ADE) Rate | Incidence of ADEs per 1,000 patient days | 5-10 ADEs per 1,000 patient days | Fewer ADEs improve overall patient outcomes |
| Hand Hygiene Compliance | Percentage of hand hygiene opportunities correctly performed | 80-95% | Higher compliance reduces infection transmission |
| Patient Identification Accuracy | Percentage of correct patient identifications before procedures | 99-100% | Ensures correct treatment and reduces errors |
| Time to Respond to Alarms | Average time in seconds to respond to patient alarms | Less than 60 seconds | Faster response improves patient safety and outcomes |
Patient safety is at the forefront of clinical research, and advancements in technology have significantly bolstered efforts to protect participants throughout the study process. Enhanced patient safety measures include comprehensive monitoring systems that track participants’ health status in real-time. For instance, wearable devices can continuously monitor vital signs such as heart rate and blood pressure, alerting researchers to any concerning changes that may require immediate attention.
Furthermore, enhanced patient safety protocols often involve robust informed consent processes that ensure participants are fully aware of potential risks associated with their involvement in a study. By utilizing digital platforms for consent management, researchers can provide participants with clear and accessible information about the study’s objectives, procedures, and potential side effects. This transparency not only empowers participants but also fosters a culture of safety and ethical responsibility within research teams.
Cost Savings
Cost savings are a significant consideration in clinical research, where budgets can quickly escalate due to inefficiencies and unforeseen challenges. Streamlining processes through technology can lead to substantial financial benefits for research organizations. For example, by implementing electronic data capture systems, organizations can reduce the costs associated with paper-based documentation, including printing, storage, and manual labor for data entry.
Moreover, cost savings extend beyond direct expenses; they also encompass time savings that translate into financial efficiency. Faster recruitment processes enabled by digital platforms can lead to quicker enrollment of participants, reducing the overall duration of the study. In a recent oncology trial, the use of online recruitment strategies resulted in a 30% reduction in enrollment time compared to traditional methods.
This acceleration not only saves money but also allows researchers to bring new treatments to market more swiftly.
Efficient Study Management
Efficient study management is essential for ensuring that clinical trials are conducted smoothly and effectively. The integration of project management tools and software has revolutionized how research teams coordinate their efforts. These tools facilitate better communication among team members, streamline task assignments, and provide real-time updates on study progress.
For instance, using a centralized platform for project management allows researchers to track milestones and deadlines easily, ensuring that all team members are aligned with the study’s objectives. Additionally, efficient study management involves meticulous planning and resource allocation. By employing predictive analytics, research teams can anticipate potential challenges and allocate resources accordingly.
For example, if historical data indicates that certain sites tend to experience delays in patient recruitment, teams can proactively allocate additional resources or adjust timelines to mitigate these risks. This strategic approach not only enhances operational efficiency but also contributes to the overall success of the study.
Regulatory Compliance
Regulatory compliance is a critical aspect of clinical research that ensures studies are conducted ethically and safely. Adhering to regulatory guidelines is essential for protecting participants’ rights and maintaining the integrity of the research process. The implementation of electronic systems for documentation and reporting has greatly simplified compliance efforts.
These systems often include built-in features that facilitate adherence to regulatory requirements by automating documentation processes and providing audit trails. Moreover, training programs focused on regulatory compliance are increasingly being integrated into research organizations’ workflows. By ensuring that all team members are well-versed in regulatory standards and best practices, organizations can minimize the risk of non-compliance issues arising during a study.
For instance, regular training sessions on Good Clinical Practice (GCP) guidelines help researchers understand their responsibilities regarding participant safety and data integrity. This proactive approach not only safeguards participants but also enhances the credibility of the research findings.
Faster Study Timelines
The ability to conduct clinical trials within shorter timelines is a significant advantage in today’s fast-paced healthcare environment. Faster study timelines are achieved through various strategies, including streamlined processes and advanced technologies that facilitate quicker decision-making. For example, utilizing adaptive trial designs allows researchers to modify study parameters based on interim results without compromising scientific rigor.
This flexibility can lead to faster conclusions about a treatment’s efficacy or safety. Additionally, leveraging digital tools for participant engagement can expedite recruitment and retention efforts. Online platforms enable researchers to reach a broader audience quickly, allowing for faster enrollment of eligible participants.
In a recent trial for a novel vaccine, digital outreach strategies resulted in enrollment being completed weeks ahead of schedule compared to previous trials using traditional methods. The ability to bring new treatments to market more rapidly not only benefits patients but also enhances the competitive edge of research organizations in an increasingly crowded landscape. In summary, advancements in technology and methodologies are transforming clinical research across multiple dimensions—from streamlined data collection to faster study timelines—ultimately leading to improved outcomes for both researchers and participants alike.