Hypertension, commonly referred to as high blood pressure, is a chronic medical condition characterized by the elevation of blood pressure levels in the arteries. It is a significant public health concern globally, affecting approximately 1.13 billion people, according to the World Health Organization. The condition is often termed a “silent killer” because it typically presents no symptoms until it leads to severe health complications such as heart disease, stroke, and kidney failure.
The pathophysiology of hypertension is multifactorial, involving genetic predisposition, lifestyle factors such as diet and physical activity, and environmental influences. The classification of hypertension is based on systolic and diastolic blood pressure readings, with normal levels defined as less than 120/80 mmHg. Hypertension is categorized into stages: Stage 1 hypertension ranges from 130-139 systolic or 80-89 diastolic, while Stage 2 hypertension is defined as 140/90 mmHg or higher.
The management of hypertension often involves lifestyle modifications, including dietary changes, increased physical activity, and pharmacological interventions. The development of new antihypertensive medications remains a critical area of research, as effective management of blood pressure can significantly reduce the risk of cardiovascular events and improve overall health outcomes.
Key Takeaways
- Hypertension is a common condition requiring effective management strategies.
- A new drug is being tested to improve blood pressure control.
- The clinical trial aims to evaluate the drug’s safety and efficacy.
- Participants are selected based on specific inclusion and exclusion criteria.
- Study results could influence future hypertension treatment guidelines.
Overview of the New Drug
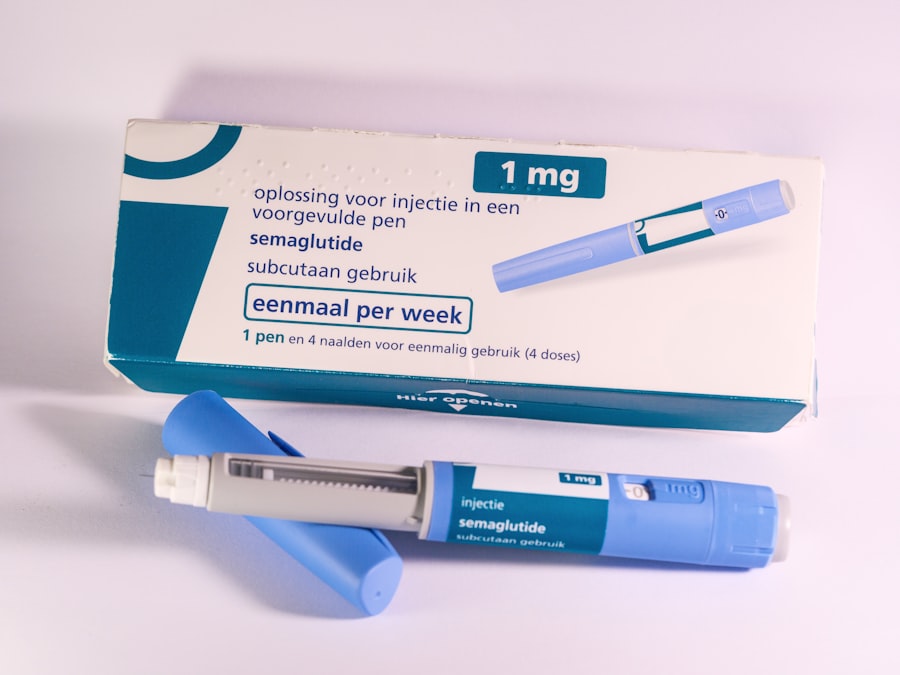
In recent years, the pharmaceutical industry has made significant strides in developing novel antihypertensive agents that target various mechanisms involved in blood pressure regulation. One such drug that has garnered attention is a new class of medication known as a dual-action angiotensin receptor-neprilysin inhibitor (ARNI). This innovative drug combines the effects of angiotensin receptor blockers (ARBs) with neprilysin inhibitors to enhance vasodilation and promote natriuresis, thereby effectively lowering blood pressure.
The mechanism of action of this new drug involves the inhibition of neprilysin, an enzyme responsible for the degradation of natriuretic peptides, which play a crucial role in cardiovascular homeostasis. By preventing the breakdown of these peptides, the drug increases their availability in the bloodstream, leading to enhanced vasodilation and diuresis. Additionally, the angiotensin receptor blockade prevents the vasoconstrictive effects of angiotensin II, further contributing to blood pressure reduction.
Clinical trials have shown promising results regarding the efficacy and safety profile of this new drug, making it a potential game-changer in the management of hypertension.
Purpose and Objectives of the Clinical Trial

The primary purpose of the clinical trial evaluating this new antihypertensive drug is to assess its efficacy in lowering blood pressure compared to standard treatment options. The trial aims to determine whether this dual-action ARNI can achieve superior blood pressure control while maintaining an acceptable safety profile. Secondary objectives include evaluating the drug’s impact on cardiovascular outcomes, quality of life measures, and its long-term effects on renal function.
To achieve these objectives, the trial will employ a randomized, double-blind design to minimize bias and ensure robust data collection. Participants will be assigned to receive either the new drug or a placebo, with blood pressure measurements taken at regular intervals throughout the study period. Additionally, researchers will monitor participants for any adverse events or side effects associated with the medication.
By rigorously evaluating both efficacy and safety, the trial aims to provide comprehensive data that could support regulatory approval and clinical use of this innovative treatment for hypertension.
Inclusion and Exclusion Criteria for Participants
| Criteria Type | Description | Example Metrics | Purpose |
|---|---|---|---|
| Inclusion Criteria | Characteristics that participants must have to be eligible for the study |
|
Ensure participants are appropriate for the study objectives |
| Exclusion Criteria | Characteristics that disqualify participants from the study |
|
Protect participant safety and maintain data integrity |
| Screening Metrics | Data collected to assess eligibility |
|
Determine if participants meet inclusion/exclusion criteria |
| Enrollment Rate | Number of participants enrolled per time period | Participants per week/month | Monitor recruitment efficiency |
| Screen Failure Rate | Percentage of screened participants who do not meet criteria | Screen failures / total screened × 100% | Evaluate strictness and feasibility of criteria |
The selection of participants for clinical trials is critical to ensuring that the results are applicable to the broader population. For this study, specific inclusion criteria have been established to identify individuals who would benefit most from the new drug. Eligible participants must be adults aged 18 years or older diagnosed with Stage 1 or Stage 2 hypertension, with baseline systolic blood pressure readings between 130-180 mmHg.
Additionally, participants should not have any contraindications to ARNI therapy or significant comorbidities that could confound the results. Conversely, exclusion criteria are equally important in maintaining the integrity of the trial. Individuals with secondary hypertension due to identifiable causes such as renal artery stenosis or endocrine disorders will be excluded from participation.
Furthermore, those currently taking other antihypertensive medications that could interfere with the study drug’s effects will not be eligible. Pregnant or breastfeeding women, as well as individuals with a history of severe allergic reactions to any components of the study drug, will also be excluded to ensure participant safety and minimize potential risks during the trial.
Study Design and Methodology
The clinical trial will utilize a randomized controlled design, which is considered the gold standard for evaluating new treatments. Participants will be randomly assigned to receive either the new dual-action ARNI or a placebo for a predetermined duration, typically ranging from 12 to 24 weeks. This approach allows researchers to compare outcomes between groups while controlling for confounding variables that could influence blood pressure readings.
The methodology will involve regular monitoring of participants’ blood pressure at baseline and throughout the study period using standardized measurement techniques. In addition to blood pressure assessments, researchers will collect data on participants’ adherence to medication regimens through self-reported diaries and pill counts. Quality of life will be evaluated using validated questionnaires designed to assess how hypertension and its treatment impact daily living.
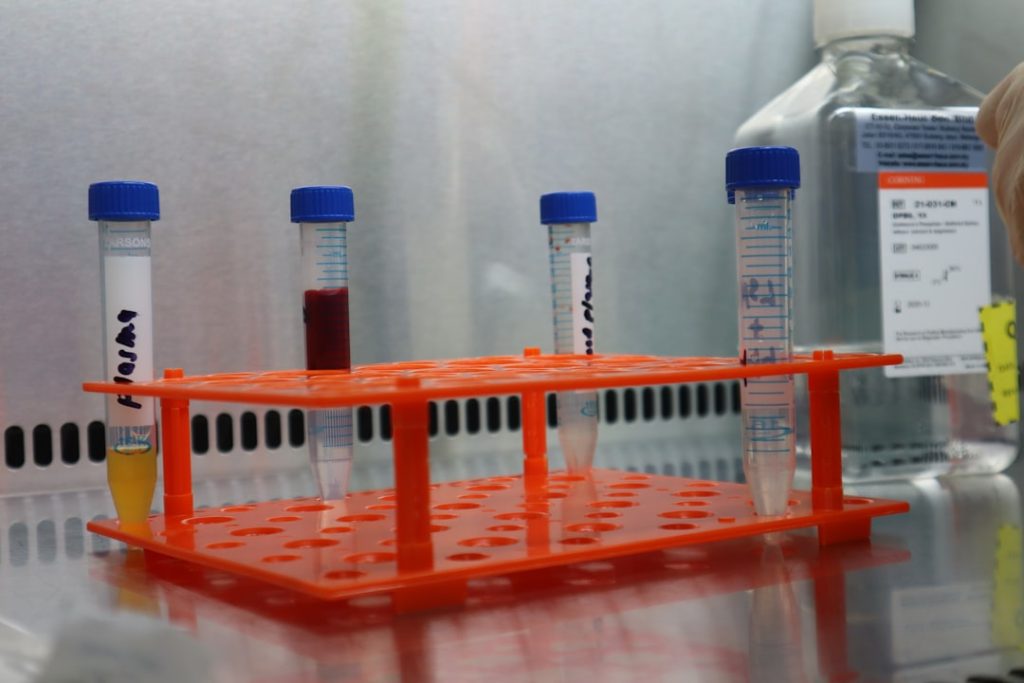
The study will also include laboratory assessments to monitor renal function and electrolyte levels, ensuring that any potential adverse effects are promptly identified and managed.
Data Collection and Analysis
Data collection in this clinical trial will be systematic and comprehensive to ensure that all relevant information is captured accurately. Blood pressure measurements will be taken at multiple time points during the study, allowing for a detailed analysis of changes over time. Additionally, researchers will collect demographic information, medical history, and lifestyle factors that may influence blood pressure outcomes.
Once data collection is complete, statistical analysis will be performed using appropriate methods to compare outcomes between the treatment and placebo groups. The primary endpoint will be the change in systolic blood pressure from baseline to the end of the study period. Secondary endpoints may include changes in diastolic blood pressure, quality of life scores, and incidence rates of adverse events.
Advanced statistical techniques such as intention-to-treat analysis will be employed to account for any dropouts or non-compliance among participants, ensuring that findings are robust and reliable.
Potential Risks and Benefits
As with any clinical trial involving new medications, there are potential risks and benefits associated with participation. The primary benefit of enrolling in this study is access to an innovative treatment option that may provide superior blood pressure control compared to existing therapies. Participants may experience improved cardiovascular health outcomes as a result of effective hypertension management.
However, potential risks must also be carefully considered. Adverse effects associated with ARNI therapy may include hypotension, hyperkalemia, renal impairment, or allergic reactions. Participants will be closely monitored throughout the trial for any signs of these complications, and appropriate measures will be taken to address them promptly.
Informed consent will be obtained from all participants before enrollment, ensuring they are fully aware of both potential benefits and risks associated with their participation in the study.
Conclusion and Future Implications
The ongoing research into new antihypertensive medications like the dual-action ARNI represents a significant advancement in the management of hypertension. As clinical trials continue to evaluate their efficacy and safety profiles, there is hope that these innovative treatments will provide better outcomes for patients struggling with high blood pressure. If successful, this new drug could not only improve individual health but also reduce the overall burden of cardiovascular disease on healthcare systems worldwide.
The implications of this research extend beyond immediate clinical applications; they may also inform future guidelines for hypertension management and shape public health policies aimed at reducing hypertension prevalence. As more data becomes available regarding long-term outcomes associated with this new therapy, healthcare providers may gain valuable insights into optimizing treatment strategies for diverse patient populations. Ultimately, continued investment in research and development within this field holds promise for transforming how hypertension is treated and managed in the years to come.