Effective clinical trial monitoring is a cornerstone of successful clinical research, serving as a critical mechanism to ensure the integrity of data and the safety of participants. The primary objective of monitoring is to verify that the trial is conducted in accordance with the protocol, Good Clinical Practice (GCP), and applicable regulatory requirements. This oversight is essential not only for maintaining the credibility of the research but also for safeguarding the rights and well-being of participants.
Inadequate monitoring can lead to significant issues, including data discrepancies, ethical violations, and even harm to participants, which can ultimately jeopardize the entire study. Moreover, effective monitoring plays a vital role in fostering trust among stakeholders, including sponsors, regulatory authorities, and the public. When a clinical trial is monitored rigorously, it enhances the reliability of the findings, which is crucial for gaining regulatory approval and for the eventual translation of research into clinical practice.
For instance, a well-monitored trial can provide robust evidence that a new drug is both safe and effective, thereby facilitating its entry into the market. Conversely, poorly monitored trials can result in flawed conclusions that may lead to ineffective or harmful treatments being approved, underscoring the importance of diligent oversight throughout the research process.
Key Takeaways
- Effective clinical trial monitoring is crucial for ensuring data integrity and participant safety.
- Key elements include thorough planning, regular site visits, and accurate data review.
- Leveraging technology enhances monitoring efficiency and real-time data access.
- Compliance with regulatory standards is essential to maintain trial validity and approval.
- Ongoing training, stakeholder collaboration, and proactive risk management drive continuous improvement.
Key Elements of Successful Clinical Trial Monitoring
Successful clinical trial monitoring hinges on several key elements that collectively contribute to the overall effectiveness of the process. One of the most critical components is the establishment of a comprehensive monitoring plan that outlines the specific activities, responsibilities, and timelines for monitoring activities. This plan should be tailored to the unique aspects of each trial, taking into account factors such as the complexity of the study design, the therapeutic area, and the risk profile associated with the investigational product.
A well-defined monitoring plan serves as a roadmap for monitors, ensuring that all necessary aspects are addressed systematically. Another essential element is the selection and training of qualified monitors who possess not only the requisite technical knowledge but also strong interpersonal skills. Monitors must be adept at building rapport with site staff while maintaining an objective stance to ensure compliance with protocols and regulations.
Their ability to communicate effectively can significantly influence how site personnel perceive monitoring activities, which in turn can impact data quality and participant safety. Furthermore, ongoing training and development opportunities for monitors are crucial to keep them updated on evolving regulations, technologies, and best practices in clinical research.
Utilizing Technology for Efficient Monitoring
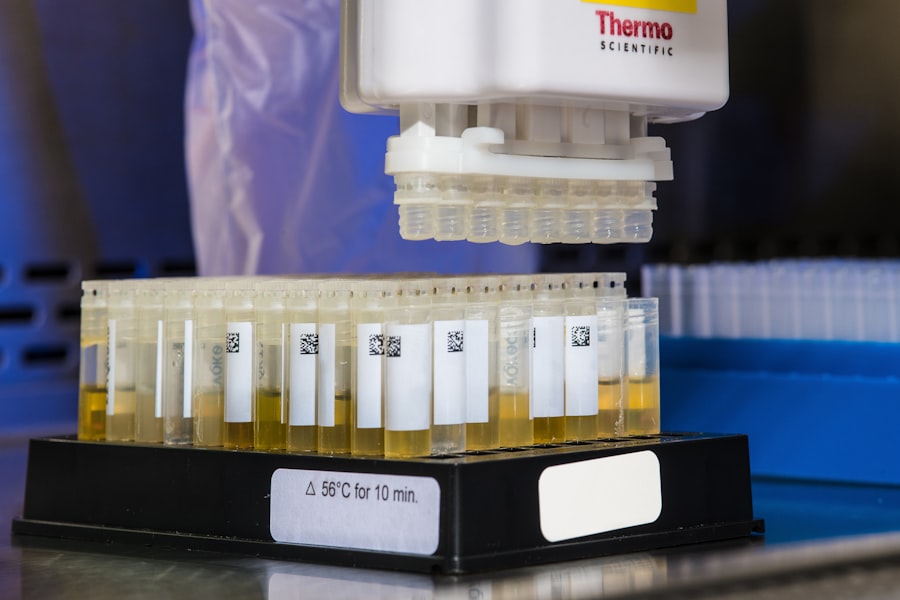
The integration of technology into clinical trial monitoring has revolutionized the way data is collected, analyzed, and reported. Electronic data capture (EDC) systems have become increasingly prevalent, allowing for real-time data entry and access. This immediacy not only enhances data accuracy but also facilitates timely identification of discrepancies or adverse events.
For example, if a site reports an unexpected increase in adverse events, monitors can quickly investigate and address potential issues before they escalate. Additionally, EDC systems often come equipped with built-in validation checks that help ensure data integrity at the point of entry. Moreover, remote monitoring technologies have gained traction, particularly in light of recent global events that have necessitated more flexible approaches to clinical trials.
Remote monitoring allows for virtual site visits and real-time communication between monitors and site staff, reducing travel costs and time while maintaining oversight. Tools such as video conferencing and secure messaging platforms enable monitors to conduct discussions with site personnel without being physically present. This shift not only streamlines monitoring processes but also allows for greater adaptability in response to unforeseen challenges that may arise during a trial.
Ensuring Compliance with Regulatory Requirements
| Metric | Description | Target | Current Value | Frequency of Measurement |
|---|---|---|---|---|
| Regulatory Audit Pass Rate | Percentage of audits passed without major findings | 95% | 92% | Quarterly |
| Number of Compliance Incidents | Count of reported compliance violations or breaches | 0 | 3 | Monthly |
| Employee Training Completion Rate | Percentage of employees completing mandatory compliance training | 100% | 87% | Annually |
| Time to Resolve Compliance Issues | Average days taken to resolve identified compliance issues | 30 days | 45 days | Monthly |
| Policy Review Frequency | Number of times compliance policies are reviewed and updated | 4 times/year | 3 times/year | Annually |
| Third-Party Compliance Rate | Percentage of third-party vendors meeting compliance standards | 100% | 95% | Bi-Annually |
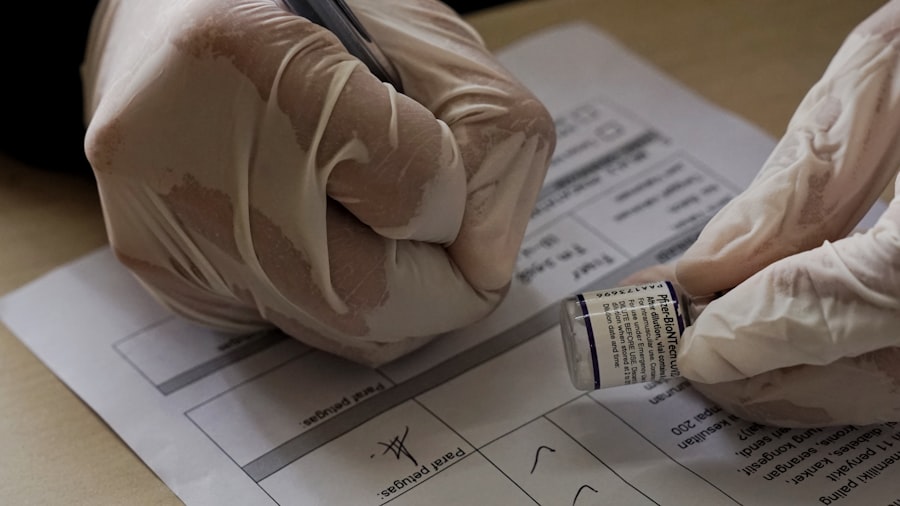
Compliance with regulatory requirements is paramount in clinical trial monitoring, as it ensures that studies are conducted ethically and that participant safety is prioritized. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have established stringent guidelines that govern clinical research practices.
Monitors play a crucial role in ensuring adherence to these regulations by conducting regular audits and inspections of trial sites. These activities help identify any deviations from protocol or regulatory standards early on, allowing for corrective actions to be implemented promptly. In addition to routine compliance checks, monitors must also stay abreast of changes in regulatory requirements that may impact ongoing trials.
For instance, recent updates to GCP guidelines or new legislation regarding data privacy can have significant implications for how trials are conducted. Continuous education and training on these evolving regulations are essential for monitors to effectively navigate compliance challenges. By fostering a culture of compliance within trial teams and ensuring that all stakeholders understand their responsibilities, monitors can help mitigate risks associated with regulatory non-compliance.
Strategies for Proactive Risk Management
Proactive risk management is an essential strategy in clinical trial monitoring that aims to identify potential issues before they manifest into significant problems. One effective approach is conducting risk assessments at the outset of a trial to identify areas that may pose challenges or uncertainties. This assessment should consider factors such as patient population characteristics, site capabilities, and historical data from similar trials.
By understanding these risks early on, monitors can develop targeted strategies to mitigate them throughout the study. Another key strategy involves implementing a risk-based monitoring approach that prioritizes resources based on identified risks. Instead of applying uniform monitoring efforts across all sites and participants, this approach allows monitors to focus their attention on higher-risk areas that require more intensive oversight.
For example, if a particular site has a history of data discrepancies or protocol deviations, it may warrant more frequent visits or additional training sessions for site staff. By allocating resources strategically based on risk profiles, organizations can enhance overall trial efficiency while ensuring participant safety.
Collaboration and Communication among Stakeholders
Collaboration and communication among stakeholders are vital components of effective clinical trial monitoring. The success of a trial often hinges on how well various parties—sponsors, investigators, site staff, and monitors—work together towards common goals. Establishing clear lines of communication from the outset can help facilitate information sharing and foster a collaborative environment.
Regular meetings and updates can ensure that all stakeholders are aligned on study objectives, timelines, and any emerging issues that may require collective problem-solving. Furthermore, leveraging collaborative tools can enhance communication efficiency among stakeholders. Platforms that allow for shared access to study documents, real-time data updates, and centralized communication channels can streamline interactions between monitors and site personnel.
For instance, using cloud-based project management tools enables all parties to track progress and address concerns promptly without relying solely on traditional methods such as emails or phone calls. This level of transparency not only improves operational efficiency but also strengthens relationships among stakeholders by promoting accountability and trust.
Training and Development for Clinical Trial Monitors
The training and development of clinical trial monitors are critical for ensuring they possess the necessary skills and knowledge to perform their roles effectively. Comprehensive training programs should encompass various aspects of clinical research, including GCP guidelines, regulatory requirements, therapeutic area specifics, and data management practices. Additionally, training should emphasize soft skills such as communication, conflict resolution, and cultural competency to prepare monitors for interactions with diverse site staff and participants.
Ongoing professional development opportunities are equally important in keeping monitors informed about industry trends and advancements in technology. Workshops, webinars, and conferences can provide valuable insights into emerging best practices in clinical trial monitoring. Furthermore, mentorship programs can facilitate knowledge transfer from experienced monitors to newcomers in the field.
By investing in continuous education and skill enhancement for monitors, organizations can cultivate a highly competent workforce capable of navigating the complexities of modern clinical trials.
Continuous Improvement and Adaptation for Optimal Monitoring
Continuous improvement is an essential philosophy in clinical trial monitoring that encourages organizations to regularly evaluate their processes and outcomes to identify areas for enhancement. Implementing feedback mechanisms allows monitors to gather insights from site staff regarding their experiences with monitoring activities. This feedback can inform adjustments to monitoring strategies or training programs to better meet the needs of sites while maintaining compliance with regulatory standards.
Adaptation is equally crucial in an ever-evolving landscape of clinical research. As new technologies emerge and regulatory frameworks shift, organizations must remain agile in their monitoring approaches. For instance, incorporating adaptive trial designs may necessitate modifications in monitoring strategies to accommodate changes in study protocols or participant enrollment criteria.
By fostering a culture of innovation and flexibility within clinical trial teams, organizations can optimize their monitoring efforts while ensuring that they remain responsive to emerging challenges in the field. In conclusion, effective clinical trial monitoring encompasses a multifaceted approach that integrates rigorous oversight with proactive risk management strategies while leveraging technology for enhanced efficiency. By prioritizing collaboration among stakeholders and investing in training for monitors, organizations can ensure compliance with regulatory requirements while continuously improving their processes for optimal outcomes in clinical research.




