Clinical study data management is a critical component of the clinical research process, serving as the backbone for the collection, storage, and analysis of data generated during clinical trials. This discipline encompasses a wide range of activities, from designing data collection tools to ensuring compliance with regulatory standards. The primary goal of clinical study data management is to ensure that the data collected is accurate, reliable, and available for analysis in a timely manner.
As clinical trials become increasingly complex, the need for robust data management practices has never been more pronounced. The landscape of clinical research is evolving rapidly, driven by advancements in technology, regulatory changes, and the growing emphasis on patient-centric approaches. As a result, data management has transitioned from a largely manual process to one that leverages sophisticated software solutions and methodologies.
This evolution not only enhances the efficiency of data handling but also improves the quality of the data collected. Understanding the intricacies of clinical study data management is essential for researchers, sponsors, and regulatory bodies alike, as it directly impacts the validity of trial outcomes and the safety of participants.
Key Takeaways
- Effective clinical study data management is crucial for reliable research outcomes.
- Optimizing data collection and storage enhances efficiency and reduces errors.
- Leveraging technology streamlines data handling and improves accuracy.
- Ensuring data security and privacy protects sensitive patient information.
- Ongoing collaboration and quality assurance drive continuous improvement in data management.
Importance of Optimizing Clinical Study Data Management
Optimizing clinical study data management is paramount for several reasons. First and foremost, efficient data management practices can significantly reduce the time required to bring new therapies to market. In an industry where time is often equated with cost, streamlining data processes can lead to substantial financial savings.
For instance, a well-organized data management system can facilitate quicker data entry and retrieval, allowing researchers to focus on analysis rather than administrative tasks. This efficiency not only accelerates the research timeline but also enhances the overall productivity of clinical teams. Moreover, optimizing data management practices contributes to improved data quality.
High-quality data is essential for making informed decisions regarding patient safety and treatment efficacy. When data is collected and managed systematically, it minimizes the risk of errors that can arise from manual processes or disorganized systems. For example, implementing standardized data entry protocols can help ensure consistency across different sites and studies.
This consistency is crucial when aggregating data from multiple sources, as it allows for more accurate comparisons and analyses.
Best Practices for Data Collection and Storage

Effective data collection and storage are foundational elements of clinical study data management. One best practice involves the use of electronic data capture (EDC) systems, which streamline the process of collecting and storing clinical trial data. EDC systems allow for real-time data entry, reducing the lag time between data collection and analysis.
Additionally, these systems often come equipped with built-in validation checks that help identify discrepancies or errors at the point of entry, thereby enhancing data integrity. Another critical aspect of data collection is the development of comprehensive case report forms (CRFs). CRFs serve as the primary tool for capturing participant information and study outcomes.
Designing CRFs that are user-friendly and aligned with study objectives can significantly improve the quality of the collected data. For instance, incorporating skip logic in CRFs can guide users through relevant questions based on previous answers, ensuring that only pertinent information is collected. Furthermore, establishing clear guidelines for data entry can help maintain consistency across different sites and personnel involved in the study.
When it comes to storage, adopting a centralized database system can facilitate easier access to data while ensuring that it remains secure. Centralized databases allow for efficient data management by consolidating information from various sources into a single repository. This approach not only simplifies data retrieval but also enhances collaboration among research teams.
Additionally, implementing regular backups and disaster recovery plans is essential to safeguard against potential data loss due to technical failures or unforeseen events.
Utilizing Technology for Efficient Data Management
| Technology | Purpose | Key Metrics | Benefits | Example Tools |
|---|---|---|---|---|
| Database Management Systems (DBMS) | Store and organize large datasets | Query response time, data retrieval speed, uptime | Improved data accessibility, consistency, and security | MySQL, PostgreSQL, Oracle DB |
| Cloud Storage Solutions | Remote data storage and backup | Storage capacity, data transfer speed, availability | Scalability, disaster recovery, cost efficiency | Amazon S3, Google Cloud Storage, Microsoft Azure |
| Data Analytics Platforms | Analyze and visualize data for insights | Processing speed, accuracy, user adoption rate | Better decision-making, trend identification | Tableau, Power BI, Google Data Studio |
| Data Integration Tools | Combine data from multiple sources | Integration time, error rate, data freshness | Unified data view, improved data quality | Talend, Apache Nifi, Informatica |
| Automation Software | Automate repetitive data management tasks | Task completion time, error reduction, throughput | Increased efficiency, reduced manual errors | UiPath, Automation Anywhere, Microsoft Power Automate |
The integration of technology into clinical study data management has revolutionized how researchers handle data throughout the trial lifecycle. Advanced software solutions now offer a range of functionalities that enhance efficiency and accuracy in data management processes. For example, cloud-based platforms enable real-time collaboration among team members across different geographical locations.
This capability is particularly beneficial in multi-site trials where coordination among various stakeholders is crucial. Moreover, leveraging artificial intelligence (AI) and machine learning (ML) technologies can further optimize data management practices. These technologies can analyze large datasets quickly, identifying patterns or anomalies that may not be immediately apparent to human analysts.
For instance, AI algorithms can be employed to monitor patient recruitment trends in real-time, allowing researchers to adjust their strategies proactively if enrollment rates fall short of expectations. Additionally, predictive analytics can help forecast potential challenges in trial execution based on historical data, enabling teams to implement corrective measures before issues arise. The use of mobile applications for data collection is another technological advancement that has gained traction in recent years.
Mobile apps allow for direct patient engagement and facilitate remote monitoring of participants’ health status. This approach not only enhances patient compliance but also provides researchers with timely access to real-world data that can inform study outcomes. By harnessing these technological innovations, clinical study teams can streamline their operations and focus on delivering high-quality research results.
Ensuring Data Accuracy and Integrity
Data accuracy and integrity are paramount in clinical research, as they directly influence the validity of study findings. To ensure accuracy, it is essential to implement rigorous validation processes throughout the data management lifecycle. This includes conducting regular audits of the data collected to identify any discrepancies or inconsistencies that may arise during entry or processing.
For example, double-data entry methods can be employed where two independent personnel enter the same dataset; discrepancies are then flagged for review. Another critical aspect of maintaining data integrity is establishing clear protocols for handling missing or incomplete data. Researchers must have predefined strategies in place for addressing these issues to avoid compromising the overall quality of the dataset.
Techniques such as imputation methods can be utilized to estimate missing values based on available information, ensuring that analyses remain robust despite gaps in the dataset. Training personnel involved in data management is also vital for ensuring accuracy and integrity. Comprehensive training programs should cover best practices for data entry, handling sensitive information, and understanding regulatory requirements.
By equipping team members with the necessary skills and knowledge, organizations can foster a culture of accountability and precision in their data management efforts.
Addressing Data Security and Privacy Concerns

In an era where data breaches are increasingly common, addressing security and privacy concerns in clinical study data management is more critical than ever. The sensitive nature of health-related information necessitates stringent measures to protect participant confidentiality and comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or the General Data Protection Regulation (GDPR) in Europe. Implementing robust cybersecurity protocols is essential for safeguarding clinical trial data from unauthorized access or breaches.
This includes employing encryption techniques to protect sensitive information both at rest and in transit. Additionally, access controls should be established to ensure that only authorized personnel can view or modify specific datasets. Regular security assessments and penetration testing can help identify vulnerabilities within systems before they can be exploited by malicious actors.
Furthermore, fostering a culture of privacy awareness among all team members involved in clinical research is crucial. Training programs should emphasize the importance of protecting participant information and adhering to ethical standards throughout the research process. By instilling a sense of responsibility regarding data security, organizations can mitigate risks associated with potential breaches while maintaining participant trust.
Collaboration and Communication in Data Management
Effective collaboration and communication are vital components of successful clinical study data management. Given the multifaceted nature of clinical trials, involving diverse stakeholders—including researchers, sponsors, regulatory bodies, and participants—requires clear lines of communication to ensure that everyone is aligned on objectives and expectations. Utilizing collaborative tools such as project management software can enhance communication among team members by providing a centralized platform for sharing updates, documents, and timelines.
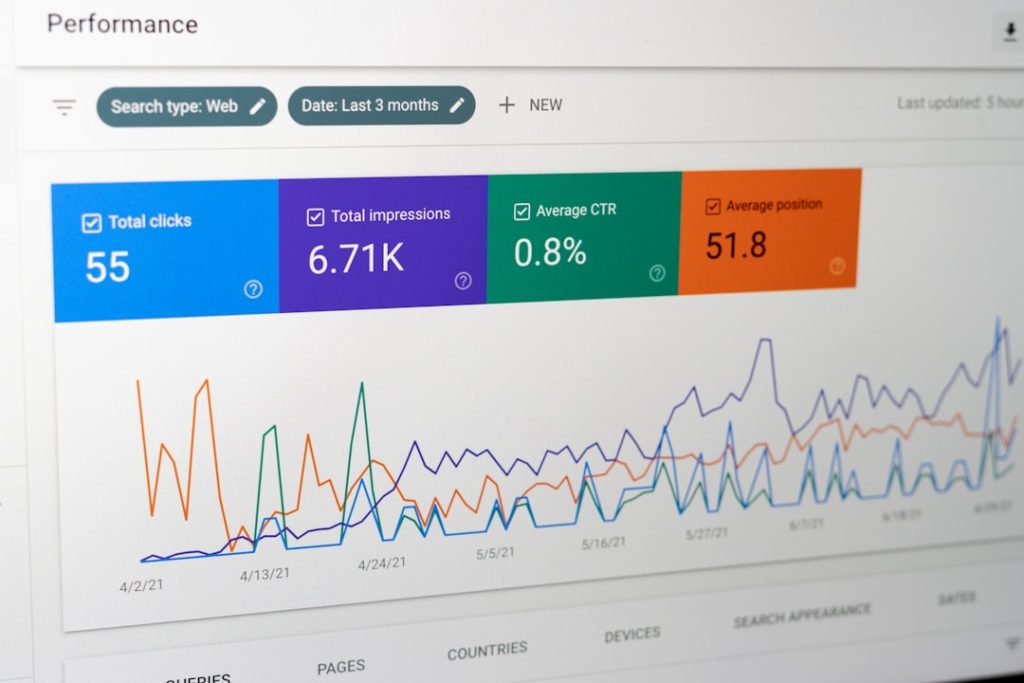
These tools facilitate transparency in project progress and allow for real-time feedback on various aspects of the study. For instance, using shared dashboards can help track key performance indicators related to patient recruitment or data collection milestones, enabling teams to address challenges promptly. Regular meetings—whether virtual or in-person—are also essential for fostering collaboration among stakeholders.
These meetings provide opportunities for team members to discuss progress, share insights, and address any concerns that may arise during the trial process. Establishing a culture of open communication encourages team members to voice their opinions or raise issues without fear of repercussions, ultimately leading to more effective problem-solving and decision-making.
Continuous Improvement and Quality Assurance in Clinical Study Data Management
Continuous improvement is a fundamental principle in clinical study data management that ensures processes remain efficient and effective over time. Implementing quality assurance (QA) measures throughout the research lifecycle helps identify areas for enhancement while maintaining compliance with regulatory standards. One approach to fostering continuous improvement is conducting regular reviews of data management processes to assess their effectiveness.
This may involve analyzing key performance metrics related to data quality, timeliness, and compliance with protocols. By identifying trends or recurring issues within these metrics, organizations can develop targeted strategies for improvement. Additionally, soliciting feedback from team members involved in various stages of the clinical trial process can provide valuable insights into potential areas for enhancement.
Creating an environment where team members feel comfortable sharing their experiences allows organizations to learn from both successes and challenges encountered during trials. Incorporating lessons learned from previous studies into future projects is another critical aspect of continuous improvement in clinical study data management. By documenting best practices and challenges faced during past trials, organizations can refine their approaches and enhance overall efficiency in subsequent studies.
In conclusion, optimizing clinical study data management through best practices, technology utilization, security measures, collaboration efforts, and continuous improvement initiatives is essential for advancing clinical research outcomes while ensuring participant safety and regulatory compliance.