Cancer remains one of the most formidable challenges in modern medicine, affecting millions of individuals worldwide and presenting a complex array of biological behaviors and treatment responses. However, recent years have witnessed a surge of promising breakthroughs that are reshaping the landscape of cancer treatment. These advancements are not merely incremental improvements; they represent a paradigm shift in how we understand and combat this multifaceted disease.
From immunotherapy to precision oncology, the integration of innovative technologies and a deeper understanding of cancer biology are paving the way for more effective and personalized treatment options. The urgency for novel cancer therapies is underscored by the staggering statistics surrounding the disease. According to the World Health Organization, cancer is responsible for nearly 10 million deaths annually, making it a leading cause of mortality globally.
Traditional treatment modalities such as chemotherapy and radiation have long been the mainstays of cancer care, but they often come with significant side effects and limitations in efficacy. As researchers delve deeper into the molecular underpinnings of cancer, they are uncovering new avenues for intervention that promise to enhance patient outcomes and improve quality of life. This article explores several groundbreaking approaches that are transforming cancer treatment, highlighting their mechanisms, applications, and potential impact on future therapies.
Key Takeaways
- Immunotherapy and CAR-T cell therapy are revolutionizing cancer treatment by utilizing the immune system to target cancer cells.
- Targeted therapy and precision oncology enable personalized treatment plans based on the genetic profile of specific cancer types.
- Advances in radiation therapy are enhancing treatment accuracy and minimizing damage to healthy tissues.
- Emerging drug therapies focus on novel mechanisms to block cancer growth and overcome resistance.
- Future cancer treatments hold promise with innovative technologies that could significantly improve patient outcomes.
Immunotherapy: Harnessing the Power of the Immune System
Immunotherapy has emerged as a revolutionary approach in the fight against cancer, leveraging the body’s own immune system to identify and destroy malignant cells. Unlike traditional treatments that directly target cancer cells, immunotherapy aims to enhance or restore the immune system’s natural ability to recognize and combat tumors. This strategy has shown remarkable success in various cancers, including melanoma, lung cancer, and bladder cancer, leading to durable responses in some patients who previously had limited treatment options.
One of the most notable forms of immunotherapy is checkpoint inhibitors, which work by blocking proteins that inhibit immune responses. For instance, drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) target the PD-1 pathway, effectively unleashing T-cells to attack cancer cells. Clinical trials have demonstrated that these agents can lead to significant tumor shrinkage and prolonged survival in patients with advanced cancers.
Moreover, the development of personalized cancer vaccines is on the horizon, where vaccines are tailored to an individual’s tumor-specific antigens, further enhancing the immune response against their unique cancer profile.
Targeted Therapy: Precision Medicine for Specific Cancer Types
Targeted therapy represents another significant advancement in cancer treatment, focusing on specific molecular targets associated with cancer. This approach contrasts sharply with traditional chemotherapy, which indiscriminately affects rapidly dividing cells. By honing in on particular genetic mutations or aberrant signaling pathways that drive tumor growth, targeted therapies can provide more effective and less toxic treatment options.
One prominent example is the use of tyrosine kinase inhibitors (TKIs) in treating chronic myeloid leukemia (CML). Imatinib (Gleevec), a pioneering TKI, specifically targets the BCR-ABL fusion protein that results from a chromosomal translocation in CML patients. The introduction of imatinib revolutionized CML treatment, transforming it from a fatal disease into a manageable chronic condition for many patients.
Similarly, targeted therapies such as trastuzumab (Herceptin) have been developed for HER2-positive breast cancer, demonstrating how understanding specific tumor biology can lead to more effective interventions.
CAR-T Cell Therapy: Engineering the Body’s Own Immune Cells to Fight Cancer
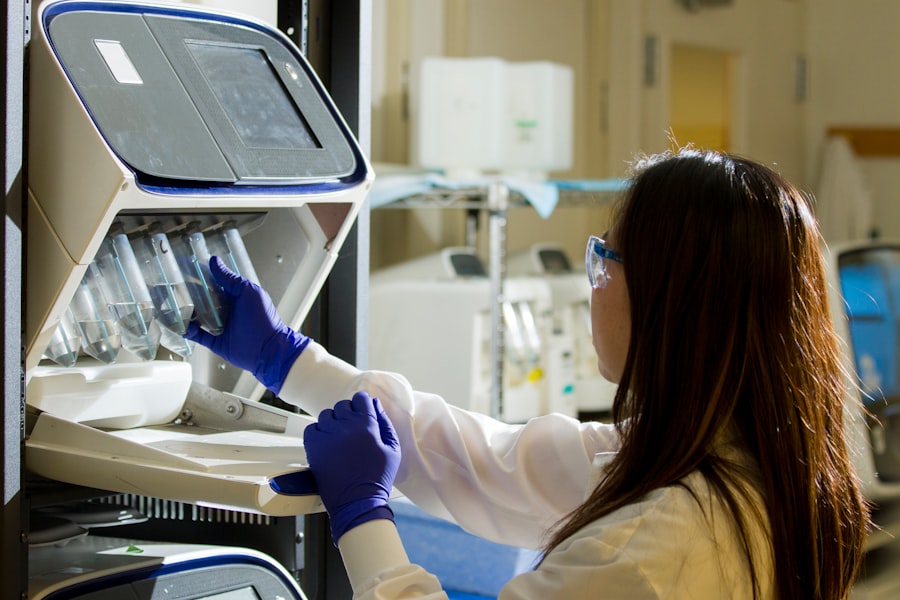
Chimeric Antigen Receptor T-cell (CAR-T) therapy represents a groundbreaking innovation in cancer treatment that involves genetically modifying a patient’s T-cells to better recognize and attack cancer cells. This personalized approach has shown remarkable efficacy in hematological malignancies such as acute lymphoblastic leukemia (ALL) and certain types of lymphoma. The process begins with collecting T-cells from the patient’s blood, which are then engineered in the laboratory to express CARs that target specific antigens found on cancer cells.
Once these modified T-cells are infused back into the patient, they proliferate and mount a robust immune response against the tumor. The success of CAR-T therapy has been exemplified by the approval of products like tisagenlecleucel (Kymriah) for treating pediatric ALL, where it has led to complete remission in a significant proportion of patients who had exhausted other treatment options. However, this therapy is not without challenges; potential side effects such as cytokine release syndrome (CRS) and neurotoxicity require careful management and monitoring.
Precision Oncology: Personalized Treatment Plans Based on Genetic Testing
| Metric | Description | Value | Unit | Year |
|---|---|---|---|---|
| Number of Clinical Trials | Total registered clinical trials worldwide | 350,000 | trials | 2023 |
| Average Duration of Clinical Trials | Time from trial start to completion | 3.5 | years | 2023 |
| Global Medical Research Funding | Total funding allocated to medical research | 150 | billion | 2023 |
| Number of Published Medical Research Papers | Annual number of peer-reviewed publications | 1,200,000 | papers | 2023 |
| Average Success Rate of Clinical Trials | Percentage of trials leading to approved treatments | 14 | % | 2023 |
| Top Research Areas | Most studied medical fields | Oncology, Cardiology, Neurology | fields | 2023 |
Precision oncology is an evolving field that tailors cancer treatment based on an individual’s genetic makeup and the specific characteristics of their tumor. By utilizing advanced genomic sequencing technologies, oncologists can identify mutations and alterations that drive tumor growth, allowing for more informed treatment decisions. This approach not only enhances the likelihood of treatment success but also minimizes unnecessary exposure to ineffective therapies.
For instance, patients with non-small cell lung cancer (NSCLC) may undergo genetic testing to identify mutations in genes such as EGFR or ALK. If a mutation is detected, targeted therapies like erlotinib (Tarceva) or crizotinib (Xalkori) can be employed, leading to improved outcomes compared to traditional chemotherapy. The integration of liquid biopsies—non-invasive tests that analyze circulating tumor DNA—further exemplifies how precision oncology is advancing.
These tests can provide real-time insights into tumor dynamics and treatment response, enabling oncologists to adapt treatment plans swiftly based on evolving tumor characteristics.
Advances in Radiation Therapy: Improving Accuracy and Effectiveness

Radiation therapy has long been a cornerstone of cancer treatment, but recent technological advancements have significantly improved its accuracy and effectiveness. Innovations such as intensity-modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT) allow for precise targeting of tumors while sparing surrounding healthy tissue. This precision reduces side effects and enhances the overall therapeutic ratio.
IMRT utilizes advanced imaging techniques to create detailed three-dimensional models of tumors, enabling oncologists to deliver varying radiation doses to different parts of the tumor while minimizing exposure to adjacent organs. This technique has been particularly beneficial in treating cancers located near critical structures, such as prostate or head and neck cancers. SBRT takes this precision a step further by delivering high doses of radiation over fewer sessions, which can be particularly effective for small tumors or metastases.
Moreover, advancements in radiopharmaceuticals are expanding the scope of radiation therapy beyond external beam techniques. Targeted radionuclide therapy involves administering radioactive substances that selectively bind to cancer cells, delivering localized radiation while minimizing systemic exposure. This approach has shown promise in treating certain types of neuroendocrine tumors and metastatic prostate cancer.
Emerging Drug Therapies: Novel Approaches to Blocking Cancer Growth
The landscape of drug therapies for cancer is rapidly evolving, with numerous novel agents being developed to block various pathways involved in tumor growth and survival. One area of focus is the inhibition of specific signaling pathways that are often dysregulated in cancer cells. For example, inhibitors targeting the PI3K/AKT/mTOR pathway have gained attention due to their role in cell proliferation and survival.
Drugs like idelalisib (Zydelig) target PI3K and have shown efficacy in treating chronic lymphocytic leukemia (CLL) and follicular lymphoma. Similarly, mTOR inhibitors such as everolimus (Afinitor) have been utilized in renal cell carcinoma and neuroendocrine tumors. These targeted approaches aim not only to halt tumor growth but also to induce apoptosis in malignant cells.
Another promising avenue involves the development of agents that exploit vulnerabilities unique to cancer cells. For instance, PARP inhibitors like olaparib (Lynparza) have been designed for patients with BRCA1 or BRCA2 mutations, capitalizing on the concept of synthetic lethality. By inhibiting DNA repair mechanisms in these genetically predisposed tumors, PARP inhibitors can lead to significant therapeutic responses.
The Future of Cancer Treatment: Potential Game-Changing Technologies and Therapies
As we look toward the future of cancer treatment, several emerging technologies hold great promise for revolutionizing patient care. One such area is artificial intelligence (AI), which is increasingly being integrated into oncology for predictive analytics and personalized treatment recommendations. AI algorithms can analyze vast datasets from clinical trials and patient records to identify patterns that may inform treatment decisions or predict outcomes more accurately than traditional methods.
Additionally, advancements in nanotechnology are paving the way for targeted drug delivery systems that can enhance therapeutic efficacy while minimizing side effects. Nanoparticles can be engineered to deliver chemotherapeutic agents directly to tumor sites or even facilitate imaging techniques that allow for real-time monitoring of treatment response. Furthermore, ongoing research into combination therapies—integrating immunotherapy with targeted therapies or radiation—holds potential for synergistic effects that could enhance overall treatment efficacy.
As our understanding of tumor biology deepens and new technologies emerge, the future landscape of cancer treatment promises not only improved survival rates but also a greater emphasis on quality of life for patients navigating their cancer journeys. In conclusion, the field of oncology is undergoing a transformative evolution driven by innovative therapies and technologies that harness our understanding of cancer biology. As these breakthroughs continue to unfold, they offer hope for more effective treatments tailored to individual patients’ needs, ultimately changing the narrative around cancer from one of despair to one of optimism and possibility.



