Cancer remains one of the most formidable health challenges of our time, affecting millions of individuals globally. The complexity of cancer, characterized by its diverse types and stages, necessitates a multifaceted approach to treatment. As research continues to evolve, the landscape of cancer treatment options has expanded significantly, offering hope to patients and their families.
Understanding the various treatment modalities available is crucial for informed decision-making and effective management of the disease. The treatment of cancer typically involves a combination of therapies tailored to the individual’s specific type of cancer, its stage, and the patient’s overall health. Traditional methods such as surgery, chemotherapy, and radiation therapy have long been the cornerstone of cancer treatment.
However, advancements in medical science have led to the development of innovative therapies that promise improved outcomes and fewer side effects. This article delves into both traditional and emerging treatment options, highlighting the importance of personalized approaches in the fight against cancer.
Key Takeaways
- Cancer treatment includes traditional methods like surgery, chemotherapy, and radiation.
- Emerging options focus on immunotherapy and targeted therapies for more precise treatment.
- Personalized medicine tailors treatments based on individual genetic profiles.
- Advances in radiation therapy improve accuracy and reduce side effects.
- Integrative and complementary therapies support overall patient well-being alongside conventional treatments.
Traditional Cancer Treatments
Traditional cancer treatments have been the foundation of oncology for decades, with surgery often serving as the first line of defense against localized tumors. Surgical intervention aims to remove cancerous tissue from the body, which can be curative in cases where the cancer has not metastasized. For instance, lumpectomy and mastectomy are common surgical procedures for breast cancer, while colectomy is frequently performed for colorectal cancer.
The effectiveness of surgery largely depends on the tumor’s size, location, and stage at diagnosis. Chemotherapy is another cornerstone of traditional cancer treatment, employing cytotoxic drugs to target rapidly dividing cancer cells. This systemic approach can be particularly effective for cancers that have spread beyond their original site.
For example, combination chemotherapy regimens are often used in treating leukemia and lymphoma, where multiple drugs work synergistically to enhance efficacy. However, chemotherapy is not without its drawbacks; it can lead to significant side effects such as nausea, fatigue, and immunosuppression due to its impact on healthy cells. Despite these challenges, chemotherapy remains a vital tool in the oncologist’s arsenal.
Radiation therapy is also a traditional method that utilizes high-energy particles or waves to destroy or damage cancer cells. It can be used as a primary treatment or adjuvantly after surgery to eliminate residual disease. Techniques such as external beam radiation therapy (EBRT) and brachytherapy allow for targeted delivery of radiation, minimizing damage to surrounding healthy tissues.
For instance, EBRT is commonly employed in prostate cancer treatment, while brachytherapy is often used for cervical cancer. The precision of modern radiation techniques has significantly improved outcomes while reducing side effects.
Emerging Cancer Treatment Options

As our understanding of cancer biology deepens, new treatment modalities are emerging that offer innovative approaches to combat this complex disease. One such area of advancement is the development of novel drug therapies that target specific molecular pathways involved in cancer progression. These targeted therapies aim to disrupt the mechanisms that allow cancer cells to grow and divide uncontrollably.
For example, tyrosine kinase inhibitors like imatinib have revolutionized the treatment of chronic myeloid leukemia by specifically targeting the BCR-ABL fusion protein responsible for the disease. Another promising avenue in emerging cancer treatments is the use of gene therapy. This approach involves modifying or manipulating genes within a patient’s cells to treat or prevent disease.
For instance, CAR T-cell therapy has gained significant attention for its success in treating certain types of blood cancers. In this process, a patient’s T-cells are genetically engineered to express chimeric antigen receptors (CARs) that recognize and attack cancer cells. Clinical trials have demonstrated remarkable remission rates in patients with refractory B-cell malignancies, showcasing the potential of gene therapy as a transformative treatment option.
Additionally, advancements in nanotechnology are paving the way for more effective drug delivery systems that can enhance the efficacy of existing treatments while minimizing side effects. Nanoparticles can be engineered to deliver chemotherapeutic agents directly to tumor sites, improving drug concentration at the target while reducing systemic exposure. This targeted delivery not only enhances therapeutic outcomes but also mitigates adverse effects associated with conventional chemotherapy.
Immunotherapy and Targeted Therapy
Immunotherapy represents a paradigm shift in cancer treatment by harnessing the body’s immune system to recognize and destroy cancer cells. Unlike traditional therapies that directly target tumor cells, immunotherapy aims to enhance or restore immune function. Checkpoint inhibitors, such as pembrolizumab and nivolumab, have emerged as groundbreaking treatments for various cancers by blocking proteins that inhibit immune responses.
These agents have shown remarkable efficacy in melanoma and lung cancer, leading to durable responses in some patients. Targeted therapy complements immunotherapy by focusing on specific molecular targets associated with cancer growth and progression. These therapies are designed to interfere with particular pathways that tumors exploit for survival.
For example, trastuzumab targets the HER2 protein overexpressed in some breast cancers, leading to improved outcomes for patients with HER2-positive tumors. The precision of targeted therapies allows for more tailored treatment plans that can significantly enhance patient outcomes while minimizing toxicity. The integration of immunotherapy and targeted therapy is an area of active research, with combination strategies being explored to maximize therapeutic benefits.
Clinical trials are investigating how these modalities can work synergistically to overcome resistance mechanisms and improve response rates across various cancer types. The potential for combining these innovative approaches represents a significant advancement in oncology, offering new hope for patients with previously untreatable cancers.
Personalized Medicine in Cancer Treatment
| Metric | Description | Value | Unit |
|---|---|---|---|
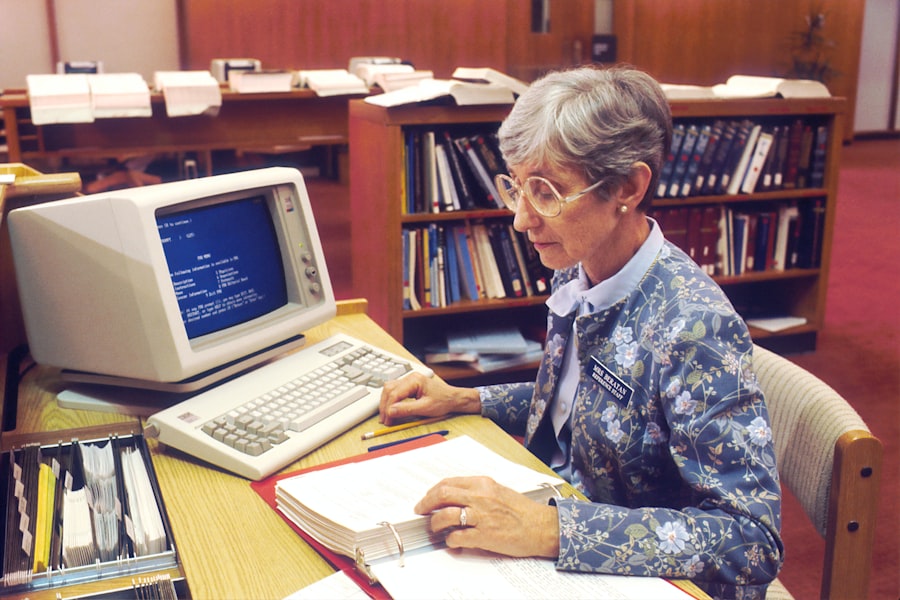
| Number of Journals | Total peer-reviewed medical journals available | 12,500 | Titles |
| Annual Research Articles Accessed | Number of research articles accessed by users annually | 150,000 | Articles |
| Database Subscriptions | Number of medical and scientific databases subscribed | 35 | Databases |
| Books and E-books | Total number of medical books and e-books available | 8,000 | Titles |
| Annual Visitors | Number of visitors to the library per year | 25,000 | Visitors |
| Research Assistance Requests | Number of research help requests handled annually | 4,500 | Requests |
| Interlibrary Loans | Number of interlibrary loan transactions per year | 1,200 | Transactions |
| Staff Members | Number of professional staff supporting research | 15 | Staff |
Personalized medicine has emerged as a revolutionary concept in oncology, emphasizing tailored treatment strategies based on an individual’s unique genetic makeup and tumor characteristics. This approach recognizes that each patient’s cancer is distinct and may respond differently to various therapies. By utilizing genomic profiling techniques, oncologists can identify specific mutations or alterations within a tumor that may inform treatment decisions.
For instance, next-generation sequencing (NGS) allows for comprehensive analysis of tumor DNA, enabling the identification of actionable mutations that can be targeted with specific therapies. In lung cancer, mutations in the EGFR gene can be effectively treated with EGFR inhibitors like erlotinib or gefitinib. Similarly, patients with melanoma harboring BRAF mutations may benefit from BRAF inhibitors such as vemurafenib.
The ability to match patients with targeted therapies based on their tumor genetics has transformed treatment paradigms and improved outcomes. Moreover, personalized medicine extends beyond targeted therapies to include immunotherapy approaches tailored to individual immune profiles. Biomarkers such as PD-L1 expression levels can guide the use of checkpoint inhibitors in specific patient populations.
By understanding the interplay between a patient’s immune system and their tumor characteristics, oncologists can optimize treatment strategies that enhance efficacy while minimizing unnecessary toxicity.
Advancements in Radiation Therapy
Radiation therapy has undergone significant advancements over recent years, enhancing its precision and effectiveness in treating various cancers. One notable development is intensity-modulated radiation therapy (IMRT), which allows for more precise targeting of tumors while sparing surrounding healthy tissues. IMRT utilizes advanced imaging techniques and computer algorithms to deliver varying radiation doses across different areas of a tumor, optimizing treatment plans based on individual patient anatomy.
Another breakthrough is stereotactic body radiation therapy (SBRT), which delivers high doses of radiation with extreme accuracy over fewer treatment sessions compared to conventional radiation therapy. SBRT is particularly beneficial for patients with early-stage lung tumors or metastatic lesions in other organs where traditional surgery may not be feasible. The ability to deliver concentrated doses while minimizing exposure to adjacent healthy structures has made SBRT a valuable option in modern oncology.
Furthermore, advancements in imaging technologies such as positron emission tomography (PET) and magnetic resonance imaging (MRI) have improved treatment planning and monitoring during radiation therapy. These imaging modalities provide real-time insights into tumor response and changes during treatment, allowing oncologists to adapt strategies as needed for optimal outcomes.
Integrative and Complementary Therapies
In addition to conventional treatments, many patients seek integrative and complementary therapies to enhance their overall well-being during cancer treatment. These approaches encompass a wide range of practices aimed at supporting physical, emotional, and psychological health alongside traditional medical interventions. Mind-body techniques such as meditation, yoga, and mindfulness have gained popularity for their potential to reduce stress and improve quality of life during cancer treatment.
Nutritional support is another critical aspect of integrative care for cancer patients. Evidence suggests that proper nutrition can play a vital role in supporting immune function and overall health during treatment. Dietitians specializing in oncology can provide personalized dietary recommendations that address specific needs based on treatment type and side effects experienced by patients.
Acupuncture has also emerged as a complementary therapy that may help alleviate symptoms associated with cancer treatment, such as pain and nausea. Research indicates that acupuncture can be effective in managing chemotherapy-induced nausea and vomiting, providing patients with additional relief during their treatment journey.
Future Directions in Cancer Treatment Research
The future of cancer treatment research holds immense promise as scientists continue to explore innovative strategies aimed at improving patient outcomes. One area garnering significant attention is the exploration of combination therapies that integrate multiple modalities—such as immunotherapy with targeted therapy or chemotherapy—to enhance efficacy while minimizing resistance. Additionally, ongoing research into the tumor microenvironment is shedding light on how interactions between cancer cells and surrounding tissues influence treatment responses.
Understanding these dynamics may lead to novel therapeutic targets that can disrupt supportive interactions within tumors. Furthermore, advancements in artificial intelligence (AI) and machine learning are poised to revolutionize oncology by enabling more accurate predictions regarding treatment responses based on vast datasets from clinical trials and patient records. AI algorithms can analyze complex patterns within genomic data to identify potential therapeutic targets or predict patient outcomes more effectively than traditional methods.
As we look ahead, collaboration between researchers, clinicians, and patients will be essential in driving forward innovative approaches that continue to redefine cancer care and improve survival rates across diverse populations affected by this challenging disease.